Digestive and endocrine disorders
Objectives
• Define the key terms and key abbreviations listed in this chapter.
• Describe gastro-esophageal reflux disease and the care required.
• Describe the care required for vomiting.
• Describe diverticular disease and the care required.
• Describe gallstones and the care required.
• Describe hepatitis and the care required.
• Describe cirrhosis and the care required.
• Describe diabetes and the care required.
Key terms
heartburn A burning sensation in the chest and sometimes the throat
hyperglycemia High (hyper) sugar (glyc) in the blood (emia)
hypoglycemia Low (hypo) sugar (glyc) in the blood (emia)
jaundice Yellowish color of the skin or whites of the eyes
vomitus Food and fluids expelled from the stomach through the mouth; emesis
KEY ABBREVIATIONS
| GERD | Gastro-esophageal reflux disease |
| HBV | Hepatitis B virus |
| I&O | Intake and output |
| IV | Intravenous |
Problems can develop in any part of the digestive system. This includes the liver, gallbladder, and pancreas—the accessory organs of digestion. The pancreas also is part of the endocrine system. Refer to Chapter 9 while you study this chapter.
Digestive disorders
The digestive system breaks down food for the body to absorb. Solid wastes are eliminated. Diarrhea, constipation, flatulence, and fecal incontinence are discussed in Chapter 23. So is ostomy care.
Gastro-esophageal reflux disease
In gastro-esophageal reflux disease (GERD) stomach contents flow back (reflux) from the stomach (gastro) into the esophagus (esophageal). Stomach contents contain acid. The acid can irritate and inflame the esophagus lining. This is called esophagitis—inflammation (itis) of the esophagus.
Heartburn is the most common symptom of GERD. Heartburn is a burning sensation in the chest and sometimes the throat. The person may have a sour taste in the back of the mouth. Occasional heartburn is not a problem. If it occurs more than twice a week, the person may have GERD. Besides heartburn, other signs and symptoms of GERD include:
• Chest pain, often when lying down
• Feeling like food is stuck in the throat
• Feeling like the throat is tight
GERD risk factors include being over-weight, alcohol use, pregnancy, and smoking. Hiatal hernia is a risk. With hiatal hernia, the upper part of the stomach is above the diaphragm. Large meals and lying down after eating can cause gastric reflux. So can certain foods—citrus fruits, chocolate, caffeine drinks, fried and fatty foods, garlic, onions, spicy foods, tomato-based foods (pasta sauce, chili, pizza).
The doctor may order medications to prevent stomach acid production or to promote stomach emptying. Surgery may be needed if medications and life-style changes do not work. Life-style changes include:
Vomiting
Vomiting means expelling stomach contents through the mouth. It signals illness or injury. Vomitus (emesis) is the food and fluids expelled from the stomach through the mouth. Aspirated vomitus can obstruct the airway. Vomiting large amounts of blood can lead to shock. These measures are needed:
• Follow Standard Precautions and the Bloodborne Pathogen Standard.
• Turn the person’s head well to one side. This prevents aspiration.
• Place a kidney basin under the person’s chin.
• Move vomitus away from the person.
• Provide oral hygiene. This helps remove the bitter taste of vomitus.
• Save a specimen for laboratory study.
• Dispose of vomitus after the nurse observes it.
• Provide for comfort. (See the inside of the front book cover.)
Diverticular disease
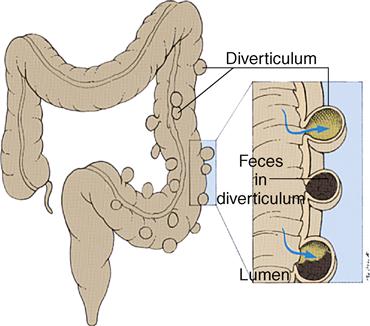
Small pouches can develop in the colon. The pouches bulge outward through weak spots in the colon (Fig. 41-1). Each pouch is called a diverticulum. (Diverticulare means to turn inside out.) Diverticulosis is the condition of having these pouches. (Osis means condition of.) The pouches can become infected or inflamed—diverticulitis. (Itis means inflammation.)
About half of all people over 60 years of age have diverticulosis. Age, a low-fiber diet, and constipation are risk factors.
When feces enter the pouches, they can become inflamed and infected. The person has abdominal pain and tenderness in the lower left abdomen. Fever, nausea and vomiting, chills, cramping, and constipation are likely. Bloating, rectal bleeding, frequent urination, and pain while voiding can occur.
A ruptured pouch is a rare complication. Feces spill out into the abdomen. This leads to a severe, life-threatening infection. A pouch also can cause a blockage in the intestine (intestinal obstruction). Feces and gas cannot move past the blocked part.
Dietary changes are ordered. Sometimes antibiotics are ordered. Surgery is needed for severe disease, obstruction, and ruptured pouches. The diseased part of the bowel is removed. Sometimes a colostomy is necessary (Chapter 23).
Gallstones
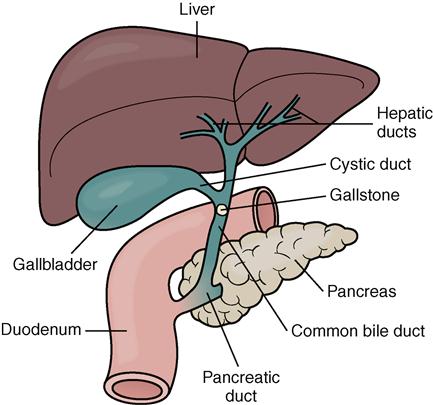
Bile is a greenish liquid made in the liver. It is stored in the gallbladder until needed to digest fat. Gallstones form when the bile hardens into stone-like pieces (Fig. 41-2).
Bile is carried from the liver to the gallbladder through ducts (tubes). The gallbladder contracts and pushes bile through the common bile duct to the small intestine. Gallstones can lodge in any of the ducts (Fig. 41-3). Bile flow is blocked. The trapped bile can cause inflammation of the gallbladder and the ducts. Liver and pancreas involvement are possible. Death can result from severe infections or damage.
Gallstones vary in size. They can be as small as a grain of sand or as large as a golf ball. A person may have one large stone. Some people have large and small stones. Risk factors include:
• Gender. Women are at greater risk than men.
• Family history. A genetic link is possible.
• Diet. A diet high in fat and cholesterol increases the risk. So does a low-fiber diet.
• Age. People over age 60 are at greater risk than younger people.
• Mexican Americans. Men and women of all ages are at risk.
• Being over-weight. Increased cholesterol reduces gallbladder emptying.
• Cholesterol-lowering medications. They increase the amount of cholesterol secreted into bile.
Signs and symptoms of a “gallbladder attack” or “gallstone attack” occur suddenly (Box 41-1, p. 628). They often follow a fatty meal. The most common treatment is surgical removal of the gallbladder.