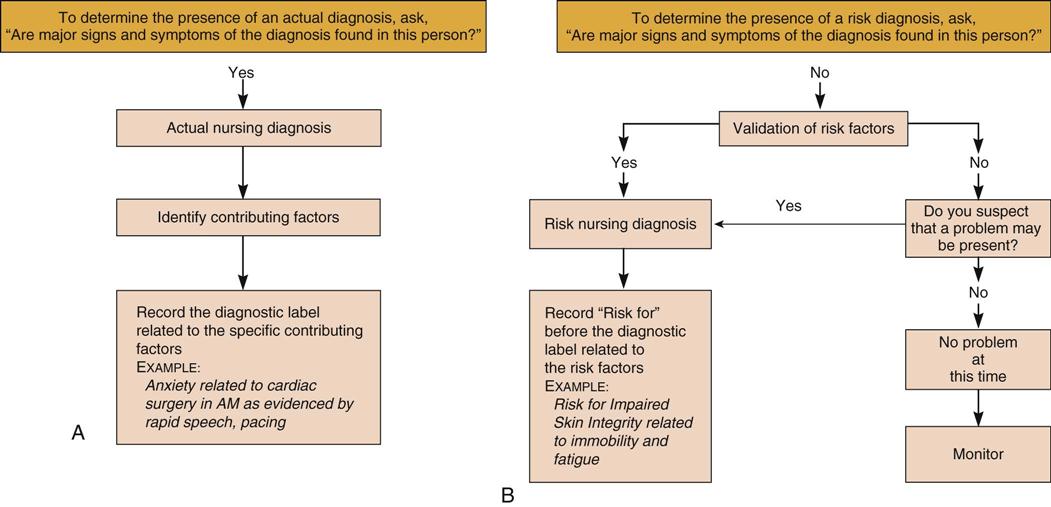
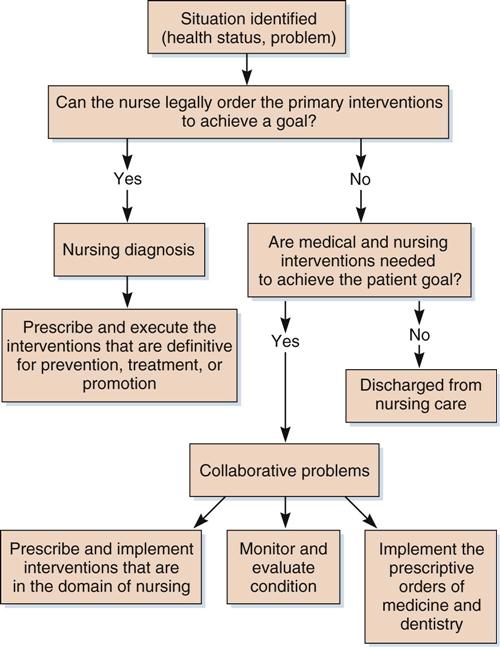
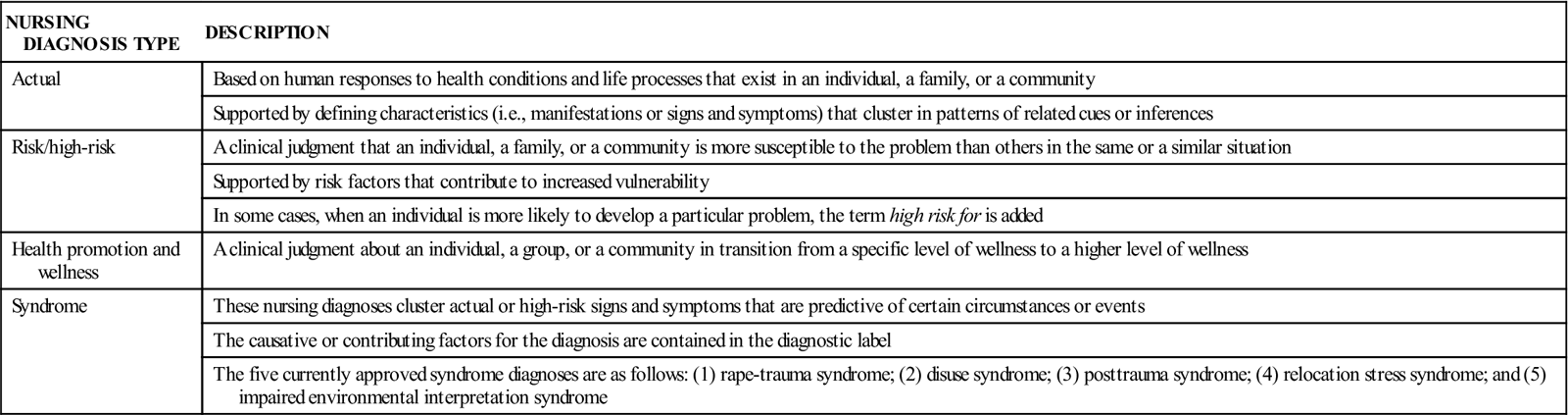
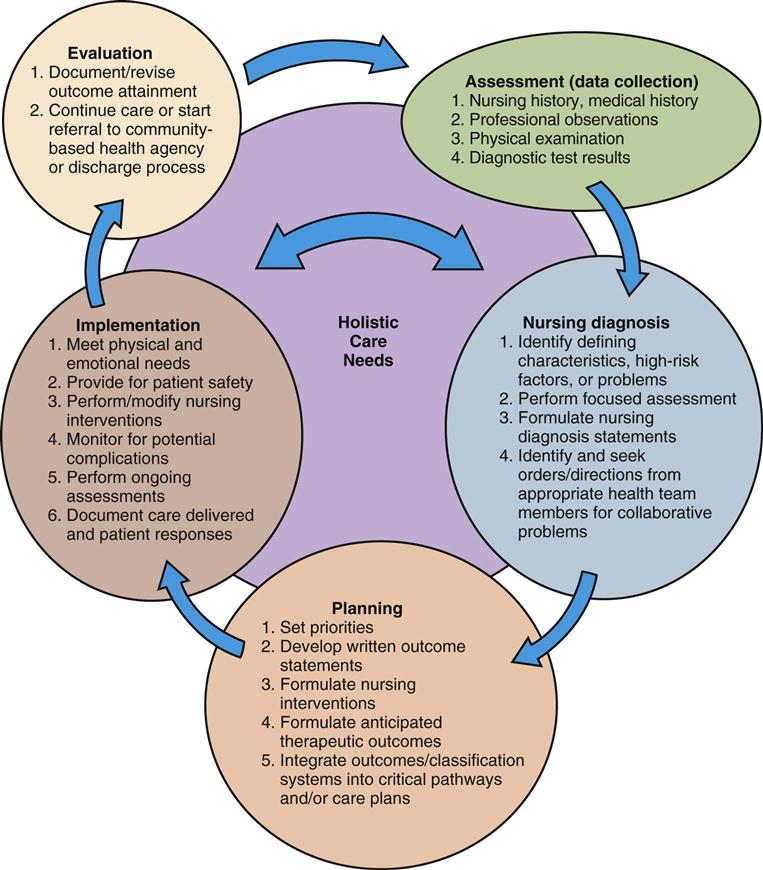
nursing process ( nursing classification systems ( multidisciplinary team ( The practice of nursing is an art and science that uses a systematic approach to identify and solve the potential problems that individuals may experience as they strive to maintain basic human function along the wellness–illness continuum. The focus of all nursing care is to help individuals maximize their potential for maintaining the highest possible level of independence for the meeting of self-care needs. Conceptual frameworks for the basis of nursing practice—such as Henderson’s Complementary-Supplement Model (1980), Roger’s Life Process Theory (1979, 1980), Roy’s Adaptation Model (1976), and the Canadian Nurses Association Testing Service (1980)—are examples of the models that are used today. The nursing process is the foundation for the clinical practice of nursing. It provides the framework for consistent nursing actions and involves the use of a problem-solving approach rather than an intuitive approach. When implemented properly, the nursing process also provides a method for evaluating the outcomes of the therapy delivered. In addition to quality of care, the nursing process provides a scientific, transferable method for health care planners to assign nursing staff to patients and to determine and justify the cost of providing nursing care in this age of soaring health care costs. Nursing classification systems such as the Nursing Minimum Data Set (NMDS), the Nursing Interventions Classification (NIC), and the Nursing Outcomes Classification (NOC) are designed to provide a standardized language for reporting and analyzing nursing care delivery that has been individualized for the patient. These information systems promote input from multidisciplinary team members who provide valuable clinical expertise, a holistic approach, and collaboration for the health care of individual patients. These systems can measure and validate the impact of actual nursing diagnoses and interventions on outcomes for patients, families, and communities. Many nursing education programs and health care facilities use the following five-step model: (1) assessment; (2) nursing diagnosis; (3) planning; (4) implementation; and (5) evaluation (Box 4-1). These five steps are actually an overlapping process (Figure 4-1). Information from each step is used to formulate and develop the next step in the process. Box 4-1 illustrates the process that is used to assemble data and organize information into categories that help the learner to identify the patient’s strengths and problem areas. Thereafter, nursing diagnosis statements can be developed, and focused nursing assessments can be initiated. Planning can be individualized, and measurable goals and anticipated therapeutic outcomes can be identified. Concurrently, individualized nursing interventions can be developed to coincide with the individual’s abilities and resources as well as the disease processes being treated. During the implementation process, the individual’s physical, psychosocial, and cultural needs must be considered. The assessment process should continue to focus not only on the evolving changes in the presenting symptoms and problems but also on the detection of potential complications that may occur (see Table 4-1 on p. 37 for the definitions of nursing diagnoses). Nurses should familiarize themselves with the nurse practice act in the state in which they practice to identify the educational and experiential qualifications that are necessary for the performing of assessments and the development of nursing diagnoses. The formulation of nursing diagnoses requires a broad knowledge base to make the discriminating judgments needed to identify the individual patient’s care needs. All members of the health care team need to contribute data regarding the patient’s care needs and his or her response to the prescribed treatment regimen. Just as body functions are constantly undergoing adjustments to maintain homeostasis in the internal and external environments, the nursing process is an ongoing cyclic process that must respond to the changing requirements of the patient. The nurse must continually interact with people in a variety of settings to establish and execute nursing functions creatively and cooperatively to meet the holistic care needs of patients (see Figure 4-1). Assessment is the first phase of the five-step nursing process. Assessment starts when the patient is admitted and continues until the patient is discharged from care. It is the problem-identifying phase of the nursing process. The initial assessment must be performed by a registered nurse with the necessary skills to complete the physical examination and the knowledge base to analyze the data, and who can identify patient problems based on defining characteristics (i.e., signs, symptoms, and clinical evidence). In addition, the nurse should identify risk factors that make an individual or group of people more vulnerable to developing certain problems in response to a disease process or to its prescribed therapy (e.g., adverse effects of drugs that may require modification of the regimen). During the assessment, the nurse collects a comprehensive information base about the patient from the physical examination, the nursing history, the medication history, and professional observations. Formats commonly used for data collection, organization, and analysis are the head-to-toe assessment, body systems assessment, and Gordon’s Functional Health Patterns Model. The head-to-toe and body systems approaches focus on the patient’s physiology, whereas the Gordon’s Functional Health Patterns Model includes sociocultural, psychological, spiritual, and developmental factors that affect the individual’s needs. Box 4-2 shows Gordon’s Functional Health Patterns Model. Nursing diagnosis is the second phase of the five-step nursing process. The North American Nursing Diagnosis Association International (NANDA-I) approved the following official definition of the term nursing diagnosis: “[a] clinical judgment about individual, family, or community responses to actual or potential health problems/life processes.” Nursing diagnoses provide the basis for the selection of nursing interventions to achieve outcomes for which the nurse is accountable (Figure 4-2). (See the inside back cover of this text for the full list of NANDA-I–approved nursing diagnoses.) A systematic method of working with patients is used to identify four types of nursing diagnoses: (1)actual; (2) risk/high-risk; (3) health promotion and wellness, and (4) syndrome (Table 4-1). This text will focus on actual and risk/high-risk nursing diagnoses (particularly those related to drug therapy) that influence the actions that the nurse must initiate to correct the problems that are encountered. Table 4-1 Using knowledge and skills related to anatomy, physiology, nutrition, psychology, pharmacology, microbiology, nursing practice skills, and communication techniques, the nurse analyzes the data collected to identify whether certain major and minor defining characteristics (i.e., manifestations or signs and symptoms) relate to a particular patient problem. If so, the nurse may conclude that certain actual problems are present. These patient-related problems are referred to as nursing diagnoses (see Figure 4-2). Not all patient problems identified during an assessment are treated by the nurse alone. Many of these problems require a multidisciplinary approach. When the nurse cannot legally order the definitive interventions required under the presenting circumstances, a collaborative problem exists (Figure 4-3). A medical diagnosis is a statement of the patient’s alterations in structure and function, and this results in the diagnosis of a disease or disorder that impairs normal physiologic function. A nursing diagnosis usually refers to the patient’s ability to perform activities of daily living (ADLs) in relation to the impairment induced by the medical diagnosis; it identifies the individual’s or group’s response to the illness. A medical diagnosis also tends to remain unchanged throughout the illness, whereas nursing diagnoses may vary, depending on the patient’s state of recovery. Concepts that help to distinguish a nursing diagnosis from a medical diagnosis include the following: The wording of an actual nursing diagnosis takes the form of a three-part statement. These statements consist of the following: (1) a diagnostic label from the NANDA-I–approved list (see inside back cover); (2) the contributing factors or cause, which may include deficits in ADLs or the medical diagnosis; and (3) the defining characteristics (i.e., manifestations or signs and symptoms). The risk/high-risk nursing diagnosis statement consists of two parts: (1) the diagnostic label from the NANDA-I–approved list; and (2) the risk factors that make the individual or group more susceptible to the development of the problem. A risk diagnosis is validated by the presence of risk factors that would contribute to the individual or group developing the stated problem. High-risk diagnoses are used for patients who are particularly vulnerable to a problem. A health promotion or wellness nursing diagnosis statement only has a one-part label. This label is initiated by the words “readiness for enhanced” followed by the nursing diagnosis being applied to the situation or group. The individual or group must understand that the higher level of functioning is feasible. This diagnosis can be applied only to individuals or groups when the potential for a higher level of wellness is realistic. Further discussion of the philosophy and clinical use of nursing diagnoses—including the specifics regarding the wording of actual and risk/high-risk diagnoses as well as the new categories of health promotion and wellness and syndrome nursing diagnoses—can be found in other primary texts and references, especially in those developed solely for the purpose of explaining nursing diagnoses. Not all patient problems identified by the nurse can be resolved by nursing actions; many care plans include interdisciplinary input and planning to maximize patient outcomes. However, the nurse is responsible for monitoring the patient on a continuum for potential complications that are associated with the medical diagnosis, the diagnostic procedures, or the treatments prescribed. To differentiate between a problem that requires a nursing diagnosis and a collaborative problem, the nurse must decide whether the definitive interventions can be ordered to prevent or treat the problem to maintain the health status of the patient (Carpenito-Moyet, 2004). A collaborative problem statement is worded as a potential complication, which is abbreviated as PC. An example would be “PC: Hypokalemia.” Outcome criteria for collaborative problems are found on critical pathways or multidisciplinary plans. A focused assessment is the process of collecting additional data specific to a patient or family that validates a suggested problem or nursing diagnosis. The questions asked or the data collected are used to confirm or rule out the defining characteristics associated with a specific nursing diagnosis statement. During the focused assessment, collaborative problems that require prescriptive orders can be identified and differentiated from solutions that the nurse can implement and that are within the nurse’s scope of practice.
The Nursing Process and Pharmacology
Objectives
Key Terms
 ) (p. 34)
) (p. 34)
 ) (p. 34)
) (p. 34)
 ) (p. 34)
) (p. 34)
The Nursing Process
![]() http://evolve.elsevier.com/Clayton
http://evolve.elsevier.com/Clayton
Assessment
Objectives
Key Term
Nursing Diagnosis
Objectives
Key Terms
NURSING DIAGNOSIS TYPE
DESCRIPTION
Actual
Based on human responses to health conditions and life processes that exist in an individual, a family, or a community
Supported by defining characteristics (i.e., manifestations or signs and symptoms) that cluster in patterns of related cues or inferences
Risk/high-risk
A clinical judgment that an individual, a family, or a community is more susceptible to the problem than others in the same or a similar situation
Supported by risk factors that contribute to increased vulnerability
In some cases, when an individual is more likely to develop a particular problem, the term high risk for is added
Health promotion and wellness
A clinical judgment about an individual, a group, or a community in transition from a specific level of wellness to a higher level of wellness
Syndrome
These nursing diagnoses cluster actual or high-risk signs and symptoms that are predictive of certain circumstances or events
The causative or contributing factors for the diagnosis are contained in the diagnostic label
The five currently approved syndrome diagnoses are as follows: (1) rape-trauma syndrome; (2) disuse syndrome; (3) posttrauma syndrome; (4) relocation stress syndrome; and (5) impaired environmental interpretation syndrome
Collaborative Problems
Focused Assessment
Planning
Objectives
< div class='tao-gold-member'>
4. The Nursing Process and Pharmacology
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree


 ) (
) ( ) (
) ( ) (
) ( ) (
) (