Nervous system and musculo-skeletal disorders
Objectives
• Define the key terms and key abbreviations listed in this chapter.
• Describe stroke and the care required.
• Describe Parkinson’s disease and the care required.
• Describe multiple sclerosis and the care required.
• Describe amyotrophic lateral sclerosis and the care required.
• Describe traumatic brain injury and spinal cord injury and the care required.
• Describe autonomic dysreflexia and the care required.
• Describe arthritis and the care required.
• Explain how to assist in the care of persons after total joint replacement surgery.
• Describe the care required for osteoporosis.
• Explain how to assist in the care of persons in casts, in traction, and with hip pinnings.
• Describe the effects of amputation.
Key terms
amputation The removal of all or part of an extremity
arthritis Joint (arthr) inflammation (itis)
arthroplasty The surgical replacement (plasty) of a joint (arthr)
closed fracture The bone is broken but the skin is intact; simple fracture
compound fracture See “open fracture”
fracture A broken bone
gangrene A condition in which there is death of tissue
hemiplegia Paralysis (plegia) on one side (hemi) of the body
open fracture The broken bone has come through the skin; compound fracture
paralysis Loss of motor function, loss of sensation, or both
paraplegia Paralysis in the legs and trunk
quadriplegia Paralysis in the arms, legs, and trunk; tetraplegia
simple fracture See “closed fracture”
tetraplegia See “quadriplegia”
KEY ABBREVIATIONS
| ADL | Activities of daily living |
| ALS | Amyotrophic lateral sclerosis |
| CVA | Cerebrovascular accident |
| MS | Multiple sclerosis |
| RA | Rheumatoid arthritis |
| ROM | Range-of-motion |
| TBI | Traumatic brain injury |
| TIA | Transient ischemic attack |
Understanding disorders of the nervous and musculo-skeletal systems gives meaning to the required care. Refer to Chapter 9 while you study this chapter.
Nervous system disorders
Nervous system disorders can affect mental and physical function. They can affect the ability to speak, understand, feel, see, hear, touch, think, control bowels and bladder, and move.
Stroke
Stroke is a disease affecting the arteries that supply blood to the brain. It also is called a brain attack or cerebrovascular accident (CVA). It occurs when one of the following happens:
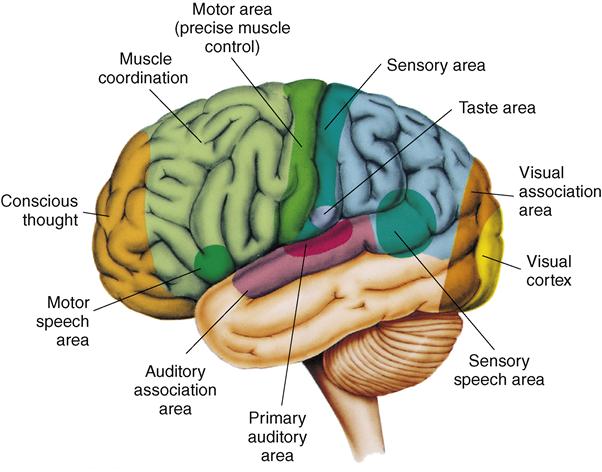
Brain cells in the affected area do not get enough oxygen and nutrients. Brain cells die. Brain damage occurs. Functions controlled by that part of the brain are lost (Fig. 39-1).
Stroke is the third leading cause of death in the United States. It is a leading cause of disability in adults. See Box 39-1 for warning signs. The person needs emergency care. Blood flow to the brain must be restored as soon as possible.
Sometimes warning signs last a few minutes. This is called a transient ischemic attack (TlA). (Transient means temporary or short term. Ischemic means to hold back [ischein] blood [hemic].) Blood supply to the brain is interrupted for a short time. Sometimes a TIA occurs before a stroke. All stroke-like symptoms signal the need for emergency care.
Risk factors
There are several risk factors for stroke. Some can be controlled, others cannot.
• Age. Older persons are at greater risk than younger persons.
• Family history. The risk increases if a parent, sister, or brother had a stroke.
• Gender. Both men and women are affected.
• Heart disease. Heart diseases can increase the risk of stroke. They include heart failure, heart attack, valve diseases, abnormal heart rhythm, and atherosclerosis (Chapter 40).
• Diabetes. Blood vessels are damaged. The person is at risk for high blood pressure and blood clots.
• High blood cholesterol. Fatty materials build up on the walls of the artery and block blood flow.
• Previous stroke or TIA. Persons who had a stroke or a TIA are at great risk.
Signs and symptoms
Stroke can occur suddenly. The person may have warning signs (see Box 39-1). The person also may have nausea, vomiting, and memory loss. Unconsciousness, noisy breathing, high blood pressure, slow pulse, redness of the face, and seizures may occur. So can hemiplegia—paralysis (plegia) on one side (hemi) of the body. The person may lose bowel and bladder control and the ability to speak. (See “Aphasia” in Chapter 37.)
Effects on the person
If the person survives, some brain damage is likely. Functions lost depend on the area of brain damage (see Fig. 39-1). The effects of stroke include:
• Loss of face, hand, arm, leg, or body control
• Changing emotions (crying easily or mood swings, sometimes for no reason)
• Difficulty swallowing (dysphagia)
• Aphasia or slowed or slurred speech (Chapter 37)
• Changes in sight, touch, movement, and thought
• Urinary frequency, urgency, or incontinence
• Loss of bowel control or constipation
Behavior changes occur. The person may forget about or ignore the weaker side. This is called neglect. It is from the loss of vision or movement and feeling on that side. Sometimes thinking is affected. The person may not recognize or know how to use common items. Activities of daily living (ADL) and other tasks are hard to do. The person may forget what to do and how to do it. If the person does know, the body may not respond.
Rehabilitation starts at once. The person may depend in part or totally on others for care. The health team helps the person regain the highest possible level of function (Box 39-2).
Parkinson’s disease
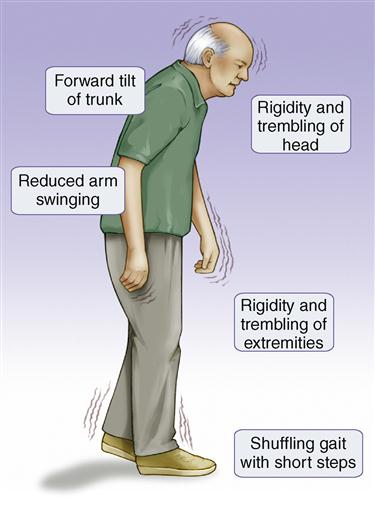
Parkinson’s disease is a slow, progressive disorder with no cure. The area of the brain controlling muscle movement is affected. Persons over the age of 50 are at risk. Signs and symptoms become worse over time (Fig. 39-2). They include:
• Rigid, stiff muscles—in the arms, legs, neck, and trunk.
• Slow movements—the person has a slow, shuffling gait.
• Stooped posture and impaired balance—it is hard to walk. Falls are a risk.
• Mask-like expression—the person cannot blink and smile. A fixed stare is common.
Other signs and symptoms develop over time. They include swallowing and chewing problems, constipation, and bladder problems. Sleep problems, depression, and emotional changes (fear, insecurity) can occur. So can memory loss and slow thinking. The person may have slurred, monotone, and soft speech. Some people talk too fast or repeat what they say.
Medications are ordered to treat and control the disease. Exercise and physical therapy are ordered to improve strength, posture, balance, and mobility. Therapy is needed for speech and swallowing problems. The person may need help with eating and self-care. Normal elimination is a goal. Safety measures are needed to prevent falls and injury.
Multiple sclerosis
Multiple sclerosis (MS) is a chronic disease. Multiple means many. Sclerosis means hardening or scarring. The myelin (which covers nerve fibers) in the brain and spinal cord is destroyed. Nerve impulses are not sent to and from the brain in the normal way. Functions are impaired or lost. There is no cure.
Symptoms often start between the ages of 20 and 40. More women are affected than men. Whites are at greater risk than other groups. A person’s risk increases if a family member has MS.
Signs and symptoms depend on the damaged area. They may include:
• Vision problems—blurred or double vision, blindness in one eye
• Numbness or weakness in the arms and legs
• Balance problems that affect standing and walking
• Tingling, prickling, or numb sensations
• Partial or complete paralysis
• Pain
• Tremors
• Problems with concentration, attention, memory, and judgment
• Problems with sexual function
• Fatigue
The person is kept active and independent as long as possible. The care plan reflects the person’s changing needs. Skin care, hygiene, and ROM exercises are important. So are turning, positioning, and deep breathing and coughing. Bowel and bladder elimination is promoted. Injuries and complications from bedrest are prevented.
Amyotrophic lateral sclerosis
Amyotrophic lateral sclerosis (ALS) attacks the nerve cells that control voluntary muscles. Commonly called Lou Gehrig’s disease, it is rapidly progressive and fatal. (Lou Gehrig was a New York Yankees baseball player. He died of the disease in 1941.)
ALS usually strikes between 40 and 60 years of age. The person usually dies 3 to 5 years after onset. Some survive for 10 or more years.
Motor nerve cells in the brain, brainstem, and spinal cord degenerate or die. They stop sending messages to the muscles. Muscles weaken, waste away (atrophy), and twitch. Over time, the brain cannot start voluntary movements or control them. The person cannot move the arms, legs, and body. Muscles for speaking, chewing, swallowing, and breathing also are affected. Eventually muscles in the chest wall fail. The person needs a ventilator for breathing (Chapter 29). The disease usually does not affect the mind or memory. Sight, smell, taste, hearing, and touch are not affected. Usually bowel and bladder functions remain intact.
ALS has no cure. Medications may slow disease progression. Damage cannot be reversed. The person is kept active and independent as long as possible. The care plan reflects the person’s changing needs. The care plan may include:
• Physical, occupational, and speech/language therapies
• Braces, a walker, or a wheelchair for mobility
• Measures to relieve pain and promote comfort
• Dysphagia diet or feeding tube
• Suctioning to remove excess fluids and saliva
• Safety measures to prevent falls and injuries
• Psychological and social support
Traumatic brain injury
Head injuries result from trauma to the scalp, skull, or brain. Some injuries are minor and do not need health care. Or the person only needs emergency care.
Traumatic brain injury (TBI) occurs when a sudden trauma damages the brain. Brain tissue is bruised or torn. Bleeding is in the brain or in nearby tissues. Spinal cord injuries are likely. Motor vehicle crashes, falls, and firearms are common causes. So are assaults and sports and recreation injuries.
Death can occur at the time of injury or later. If the person survives TBI, some permanent damage is likely. Disabilities depend on the severity and site of the injury. They include:
• Cognitive problems—thinking, memory, reasoning
• Sensory problems—sight, hearing, touch, taste, smell
• Communication problems—expressing or understanding language
• Stupor—an unresponsive state; the person can be briefly aroused
• Coma—the person is unconscious, does not respond, is unaware, and cannot be aroused
• Persistent vegetative state (PVS)—being in a vegetative state for more than one month
Rehabilitation is required. Physical, occupational, speech/language, and mental health therapies are ordered depending on the person’s needs. Nursing care depends on the person’s needs and remaining abilities.
Spinal cord injury
Spinal cord injuries can permanently damage the nervous system. Paralysis (loss of motor function, loss of sensation, or both) can result. Young adult men have the highest risk. Common causes are stab or gunshot wounds, motor vehicle crashes, falls, and sports injuries.
Problems depend on the amount of damage to the spinal cord and the level of injury. Damage may be:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree