The Child with a Genitourinary Condition
Objectives
1. Define each key term listed.
2. Name the functional unit of the kidney.
3. List four urological diagnostic procedures.
4. Recognize urinary tract anomalies in infants.
5. Differentiate between nephrosis and acute glomerulonephritis.
6. Discuss the skin care pertinent to the child with nephrosis.
7. Explain any alterations in diet applicable to the child with nephrosis.
8. Outline the nursing care for a child who is diagnosed as having Wilms’ tumor.
9. Discuss the impact of undescended testes on fertility.
Key Terms
chordee (KŎR-dē, p. 677)
cryptorchidism (krĭp-TŎR-kĭ-dĭz-ŭm, p. 685)
cystometrogram (sĭs-tō-MĔT-rō-grăm, p. 676)
dysuria (dĭs-YŪ-rē-ă, p. 676)
encopresis (ĕn-kō-PRĒ-sĭs, p. 676)
enuresis (ĕn-yū-RĒ-sĭs, p. 676)
epispadias (ĕp-ĭ-SPĀ-dē-ŭs, p. 677)
frequency (p. 676)
glomeruli (glō-MĔR-yū-lī, p. 680)
hydrocele (HĪ-drō-sēl, p. 684)
hydronephrosis (hī-drō-nĕ-FRŌ-sĭs, p. 678)
hyperkalemia (hī-pŭr-kă-LĒ-mē-ă, p. 683)
hypoalbuminemia (hī-pō-ăl-byū-mĭn-Ē-mē-ă, p. 681)
hypospadias (hī-pō-SPĀ-dē-ŭs, p. 677)
micturition (mĭk-tū-RĬSH-ŭn, p. 676)
nephron (NĔF-rŏn, p. 674)
neutropenia (nū-trō-PĒ-nē-ă, p. 681)
nocturia (nŏk-TŪ-rē-ă, p. 676)
oliguria (ŏl-ĭ-GŪ-rē-ă, p. 677)
orchiopexy (ŏr-kē-ō-PĔK-sē, p. 686)
paraphimosis (păr-ă-fī-MŌ-sĭs, p. 677)
phimosis (fī-MŌ-sĭs, p. 677)
polyuria (pŏl-ē-YŪ-rē-ă, p. 677)
pyelonephritis (pī-ĕ-lō-nĕ-FRĪ-tĭs, p. 679)
testicular torsion (tĕs-TĬK-yū-lăr TŎR-shŭn, p. 686)
ureteritis (yū-rĕ-tŭr-Ī-tĭs, p. 679)
urethritis (yū-rĕ-THRĪ-tĭs, p. 679)
urgency (p. 676)
vesicoureteral reflux (vĕs-ĭ-kō-yū-RĒ-tŭr-ăl RĒ-flŭks, p. 679)
![]() http://evolve.elsevier.com/Leifer
http://evolve.elsevier.com/Leifer
Development of the Urinary Tract
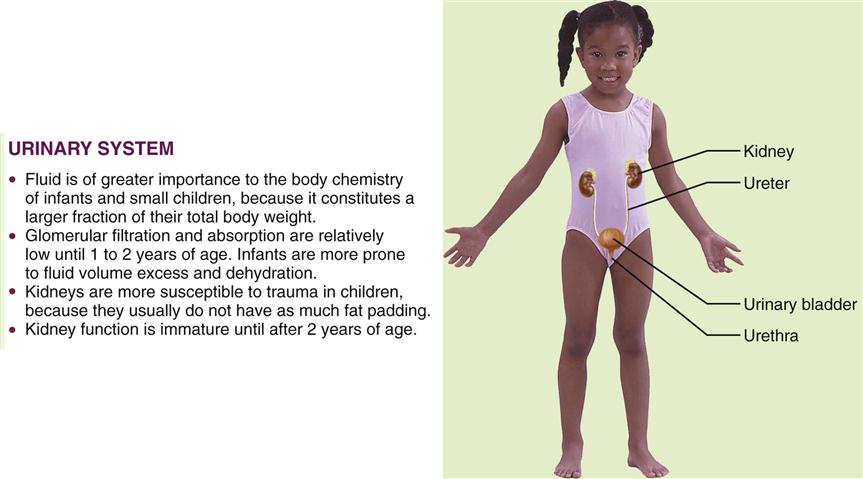
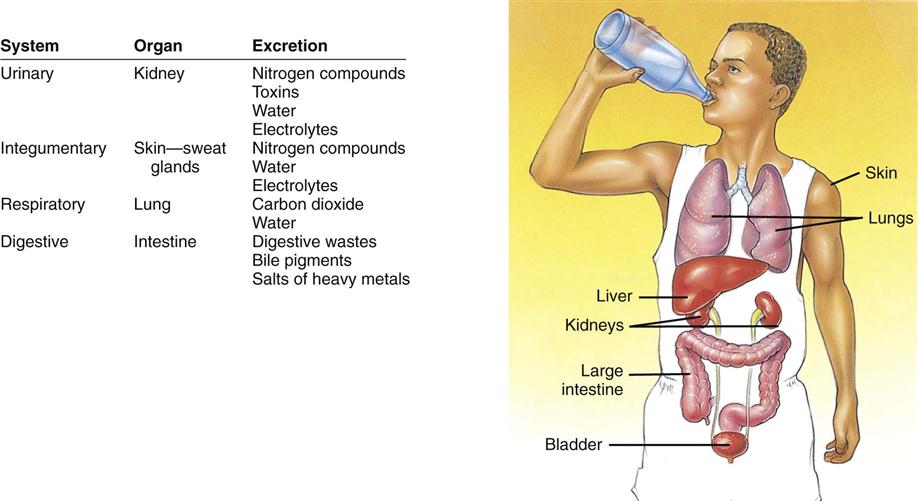
The urinary system consists of two kidneys, two ureters, the urinary bladder, and the urethra. Figure 29-1 depicts these structures and illustrates how they differ in the developing child and in the adult. The function of the kidneys is to rid the body of waste products and to maintain body fluid homeostasis (Figure 29-2). The kidneys also produce substances that stimulate red blood cell formation in the bone marrow (e.g., erythropoietin-stimulating factor [ESF]), as well as renin, which regulates blood pressure. Microscopically, the functional unit of the kidneys is the nephron. Each kidney contains more than 1 million nephrons. Although the newborn’s kidneys are immature, they function quite effectively. Nevertheless, the functional limitations must be considered carefully when the newborn is premature or ill. This applies especially to the administration of medications, formula, and parenteral fluids.
Soon after implantation, the embryonic mass differentiates into three distinct layers of cells: the ectoderm, mesoderm, and endoderm. The urinary and reproductive organs originate from the mesoderm. At approximately the third month of gestation the fetal kidney begins to secrete urine. The amount gradually increases as the fetus matures and comprises a portion of the amniotic fluid volume. An absence or small amount of amniotic fluid may indicate genitourinary difficulties.
The kidney and the urinary tract develop about the same time as the ears form during fetal life. There is an unexplained relationship between low-set ears in the newborn and urinary tract anomalies. When assessing the newborn, an imaginary line should be drawn between the outer canthus of the eye and the ear. The line should cross the tip of the auricle. If the tip of the auricle falls below this line, the assessment should be recorded and reported (see Figure 12-6).
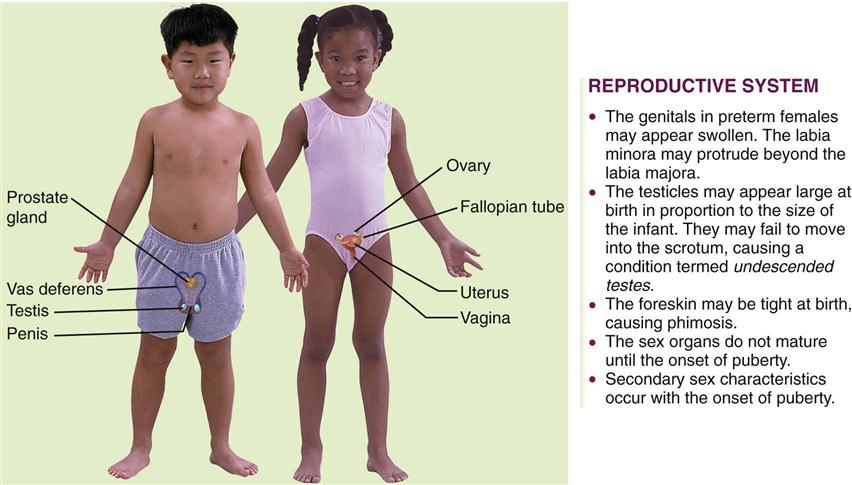
Development of the Reproductive Systems
Figure 29-3 shows the female and male reproductive systems and lists some of the differences between children and adults. The reproductive system provides for perpetuation of the species. Members of each gender are equipped with gonads (which provide reproductive cells) and a set of accessory organs. The gonads (ovaries in the female and testes in the male) produce sex cells and hormones that affect the reproductive organs and other body systems.
Sex is genetically determined at the time of fertilization. The presence of a Y chromosome is essential for the development of the testes and their hormones. Sex differentiation in the embryo occurs early. The organs specific to the male or female child develop. Before this, the embryo has neither male nor female characteristics. The development of the ovaries occurs later than that of the testes. By the twelfth week the external genitalia of the fetus are recognizably male or female.
Several tests are helpful in diagnosing conditions of the reproductive tract. These include a Papanicolaou (Pap) smear, serological blood tests, cultures, ultrasound procedures, pregnancy tests, and routine blood and urine tests. Sexual abuse in children may be manifested by behaviors such as urinary frequency, excessive masturbation, encopresis (fecal soiling beyond 4 years of age), severe nightmares, bedwetting, irritation or pain in the genital area, and a decrease in physical or emotional development. Suggestive posturing by young children or an explicit knowledge of sex acts shown by children under 8 years of age calls for further investigation. Menstrual disorders and premenstrual syndrome are discussed in Chapter 11. Sexually transmitted infections are discussed in Chapters 11 and 32.
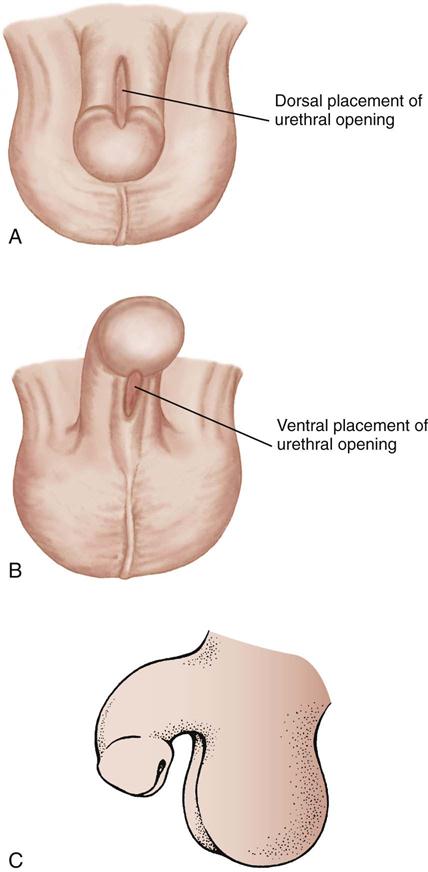
Assessment of Urinary Function
Urological diagnostic procedures include urinalysis, ultrasonography, intravenous (IV) pyelogram, and computed tomography (CT) scan of the kidneys. Renal biopsy is used to diagnose the extent of kidney disease. A uroflow is an assessment procedure used to determine the rate of urine flow. The child voids into a receptacle, and a uroflowmeter graphs the volume and pressure. This is useful in diagnosing stricture or scarring. Cytoscopy is useful for investigating congenital abnormalities or acquired lesions in the bladder and lower urinary tract. Radiographic examination of the bladder and urethra before and during micturition (voiding) is called voiding cystourethrography. The cystometrogram and urethral pressure profile assess bladder capacity and function. Both tests require catheterization and infusion of sterile water. The minimum urine output for infants and toddlers is 2 to 3 mL/kg/hr; for preschoolers and young school-age children, the minimum is 1 to 2 mL/kg/hr; and for school-age children and adolescents, the minimum is 0.5 to 1 mL/kg/hr. Common laboratory tests are reviewed in Table 29-1.
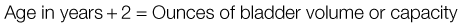
Table 29-1
Common Laboratory Tests for Urinary Tract Function
| TEST | NORMAL LEVELS* | SIGNIFICANCE OF DEVIATION |
| Blood | ||
| Blood urea nitrogen (BUN) | High BUN level indicates renal disease, dehydration, need for steroid therapy | |
| Uric acid | Child: 2-5 mg/dL | Renal disease |
| Creatinine | Severe renal disease | |
| Urine | ||
| Red blood cells | <2 million/mm3 | Trauma, infection, stones |
| Bacteria | Few | Infection |
| Casts | Occasional | Glomerular disease, pyelonephritis |
| White blood cells | <2 million/mm3 | Infection |
| Ketones | 0 | Stress; diabetes mellitus |
| Glucose | 0 | Diabetes mellitus |
| Protein | 0 | Glomerular kidney disease |
| pH | Potassium deficiency, electrolyte imbalance | |
| Specific gravity | ||
*Values for different age-groups are indicated only when relevant.
Terms commonly used to describe urinary dysfunction include the following:
• Dysuria: difficulty in urination
• Frequency: abnormal number of voidings in a short period
• Urgency: strong urges to void, often despite inability to do so
• Nocturia: awakening during the night to void
• Enuresis: uncontrolled voiding after bladder control has been established
• Polyuria: increased urine output
Anomalies of the Urinary Tract
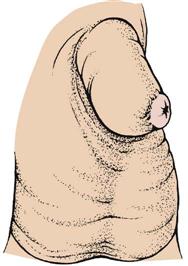
Phimosis
Pathophysiology.
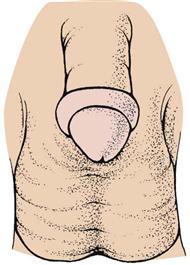
Phimosis is a narrowing of the preputial opening of the foreskin, which prevents the foreskin from being retracted over the penis (Figure 29-4). This is normal in newborns and usually disappears by 3 years of age. In some children this narrowing may obstruct the stream of urine, causing dribbling or irritation. The condition can be corrected by circumcision.
Treatment and Nursing Care.
When circumcision is performed on an older boy, careful explanations and reassurance are provided. The nurse is sensitive to the child’s embarrassment and fear. Postoperatively the penis is covered with a petroleum gauze. The penis is tender and may burn on urination.
Cleansing of the uncircumcised penis and retraction of the foreskin are discussed in Chapter 12. Forcible retraction of a tight foreskin is avoided because it can lead to paraphimosis (Figure 29-5). When this occurs, the foreskin cannot be returned to its normal position. There may be swelling and impaired circulation caused by the constriction. This condition necessitates immediate evaluation by a physician.
Hypospadias and Epispadias
Pathophysiology.
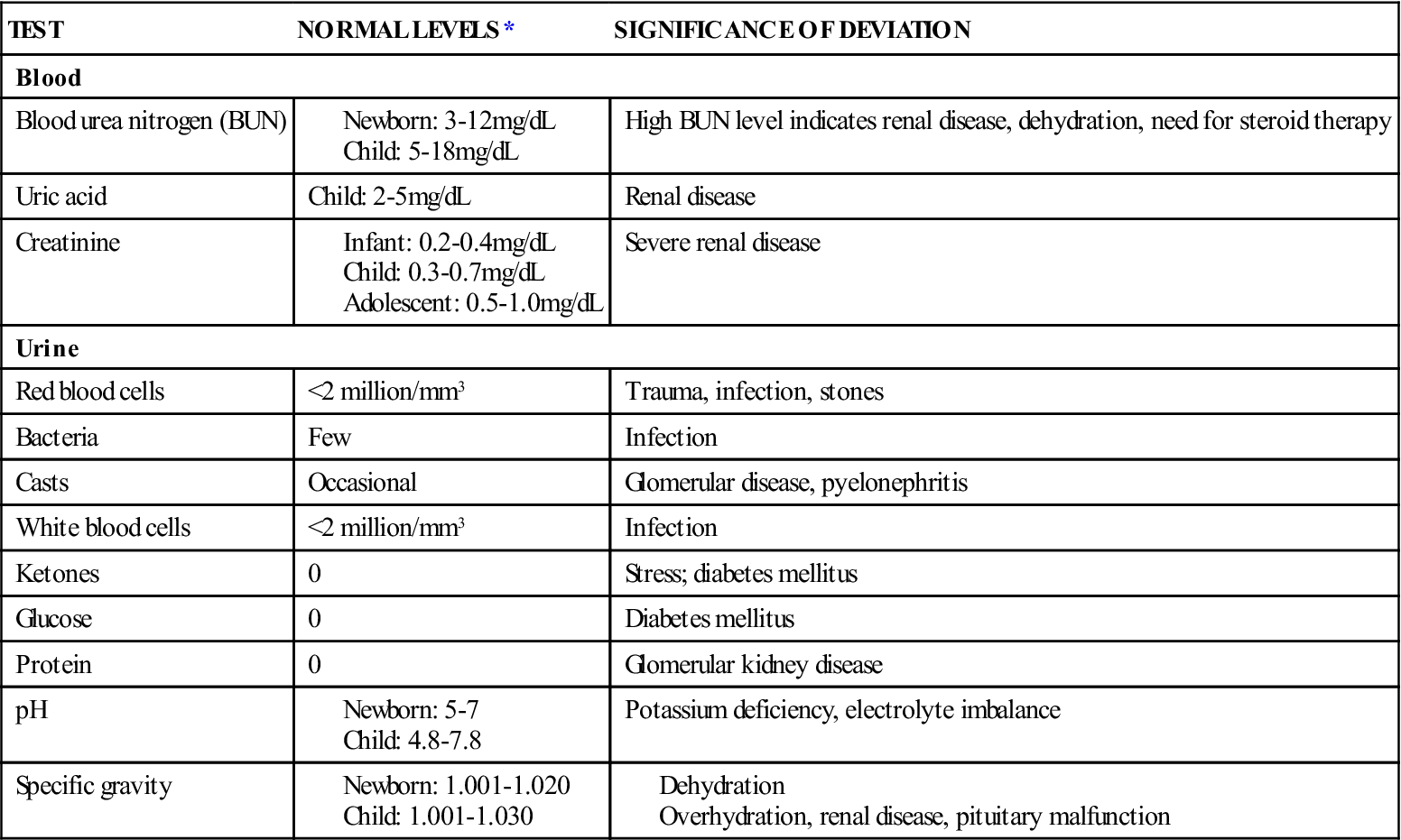
Hypospadias is a congenital defect in which the urinary meatus is located not at the end of the penis but on the lower shaft. In mild cases it lies just below the tip of the penis, but it may be found at the midshaft or near the penile-scrotal junction. With epispadias, the opening of the urinary meatus is on the upper surface of the penis. Unlike epispadias, hypospadias is fairly common, occurring in 1 out of 250 to 500 newborn boys. Hypospadias may be accompanied by chordee, a downward curvature of the penis caused by a fibrotic band of tissue (Figure 29-6).
Treatment and Nursing Care.
The alert nurse may discover hypospadias or epispadias in the nursery during neonatal assessment. In many mild cases surgery is not necessary for either condition unless the location and extent of the defect are such that the child will not be able to stand to void or the defect would cause psychological problems or difficulties in future sexual relations. Treatment consists of surgical repair and is usually performed before age 18 months. It is sometimes done in stages depending on the associated defects. Most techniques can be performed during same-day surgery. Routine circumcision is avoided in these children, because the foreskin may be useful in the repair. A urinary catheter may be required after surgery. Parents are instructed in the home care of the catheterized child. Medication for bladder spasms may be required.
This condition is corrected at a time in childhood when fears of separation and mutilation are great, and therefore attention is directed to psychological considerations. In the older child, questions about virility and reproduction may surface and need to be addressed.
Exstrophy of the Bladder
Pathophysiology.
In exstrophy of the bladder the lower portion of the abdominal wall and the anterior wall of the bladder are missing. As a result, the bladder lies open and exposed on the abdomen. Exstrophy is caused by a failure of the midline to close during embryonic development. Other congenital anomalies may also be present. This anomaly occurs in 1 out of 40,000 live births and is more common in boys than in girls.
Manifestations.
This disorder is noticeable by fetal sonogram. The defect may range from a small cutaneous fistula in the abdominal wall to complete exstrophy (the turning inside out of an organ). Urine leaks continually from the bladder. The skin around the bladder becomes excoriated. Other anomalies are common.
Treatment and Nursing Care.
The bladder is covered with a plastic shield or appropriate dressing to protect its mucosa but allow for urinary drainage. This also protects the bladder from irritation by bedclothes or diapers. The skin is protected by a suitable ointment. Diapers are generally placed under rather than around the infant. The infant is positioned on his or her back or side so that urine drains freely. Antibiotics are given to prevent infection. Surgical closure is ideally performed during the first 48 hours of life.
Obstructive Uropathy
Pathophysiology.
Many conditions, such as calculi (stones), tumors, strictures, and scarring, may cause an obstruction of the normal flow of urine. These conditions may be congenital or acquired, and blockage may be either partial or complete. One or both kidneys may be affected. The pathological changes depend on the nature and location of the problem. Hydronephrosis (hydro, “water,” and nephro, “kidney”) is the distention of the renal pelvis as the result of an obstruction. The pelvis of the kidney becomes enlarged, and cysts form. This may eventually damage renal nephrons, resulting in deterioration of the kidneys. Polycystic kidney refers to a condition in which large, fluid-filled cysts form in place of healthy kidney tissue in the fetus. This is inherited as an autosomal recessive trait. Kidney damage can result in an inability of the kidney to concentrate urine, resulting in metabolic acidosis. Urine that is not excreted promptly can promote the growth of organisms that cause urinary tract infection.
Treatment and Nursing Care.
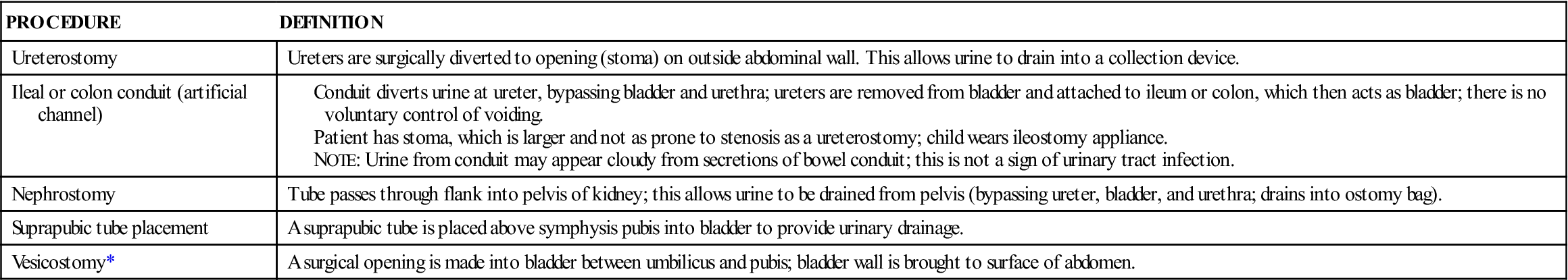
Urinary diversion is necessary in certain conditions and may be accomplished by several procedures (Table 29-2). This type of surgery is a source of great apprehension for parents. The physical care of the child with a urinary stoma (artificially created opening or passage) presents hygiene problems, skin problems, and difficulties in leaving the infant in the care of others. Frequent trips to the health care provider add to the strain of everyday life.
Table 29-2
Surgical Procedures Used in Urinary Diversion
| PROCEDURE | DEFINITION |
| Ureterostomy | Ureters are surgically diverted to opening (stoma) on outside abdominal wall. This allows urine to drain into a collection device. |
| Ileal or colon conduit (artificial channel) | |
| Nephrostomy | Tube passes through flank into pelvis of kidney; this allows urine to be drained from pelvis (bypassing ureter, bladder, and urethra; drains into ostomy bag). |
| Suprapubic tube placement | A suprapubic tube is placed above symphysis pubis into bladder to provide urinary drainage. |
| Vesicostomy* | A surgical opening is made into bladder between umbilicus and pubis; bladder wall is brought to surface of abdomen. |
Stress from the urinary diversion is age related. The toddler may be unable to attain independence in toilet training. The school-age child suffers from being different and may have a distorted body image. The adolescent may have lowered self-esteem and is concerned about sexuality. Parents with affected newborns grieve for the loss of a perfect child and experience concerns about the length and quality of the infant’s life. The nurse anticipates the impact of this type of diagnosis and incorporates suitable psychological interventions into daily care. Providing emotional support and teaching parents how to prevent infection are priorities of care.
Assessing for a distended bladder.
To assess for a distended bladder, the nurse gently palpates below the umbilicus, moving toward the symphysis pubis. The normal bladder is not palpable because it lies behind the symphysis pubis.