Comfort, rest, and sleep
Objectives
• Define the key terms and key abbreviations listed in this chapter.
• Explain why comfort, rest, and sleep are important.
• List the OBRA room requirements for comfort, rest, and sleep.
• Describe four types of pain and the factors affecting pain.
• Explain why pain is personal.
• List the signs and symptoms of pain.
• List the nursing measures that relieve pain.
• Explain why meeting basic needs is important for rest.
• Identify when rest is needed.
• Explain how circadian rhythm affects sleep.
• Describe the stages of sleep.
• Know the sleep requirements for each age-group.
• Describe the factors that affect sleep.
• Describe the common sleep disorders.
• List the nursing measures that promote rest and sleep.
• Explain how dementia affects sleep.
Key terms
acute pain Pain that is felt suddenly from injury, disease, trauma, or surgery
chronic pain Pain that continues for a long time (months or years) or occurs off and on; persistent pain
circadian rhythm Daily rhythm based on a 24-hour cycle; the day-night cycle or body rhythm
comfort A state of well-being; the person has no physical or emotional pain and is calm and at peace
distraction To change the person’s center of attention
enuresis Urinary incontinence in bed at night
guided imagery Creating and focusing on an image
insomnia A chronic condition in which the person cannot sleep or stay asleep all night
NREM sleep The phase of sleep when there is no rapid eye movement; non-REM sleep
pain To ache, hurt, or be sore; discomfort
persistent pain See “chronic pain”
phantom pain Pain felt in a body part that is no longer there
radiating pain Pain felt at the site of tissue damage and in nearby areas
relaxation To be free from mental and physical stress
REM sleep The phase of sleep when there is rapid eye movement
rest To be calm, at ease, and relaxed; no anxiety or stress
sleep A state of unconsciousness, reduced voluntary muscle activity, and lowered metabolism
KEY ABBREVIATIONS
| CMS | Centers for Medicare & Medicaid Services |
| NREM | No rapid eye movement |
| OBRA | Omnibus Budget Reconciliation Act of 1987 |
| REM | Rapid eye movement |
Comfort, rest, and sleep are needed for well-being. The total person—the physical, emotional, social, and spiritual—is affected by comfort, rest, and sleep problems. Discomfort and pain can be physical or emotional. Whatever the cause, they affect rest and sleep. They also decrease function and quality of life.
Rest and sleep restore energy and well-being. Illness and injury increase the need for rest and sleep. The body needs more energy for healing and repair. And more energy is needed for daily functions.
Comfort
Comfort is a state of well-being. The person has no physical or emotional pain. He or she is calm and at peace. Age, illness, and activity affect comfort. So do temperature, ventilation, noise, odors, and lighting. Such factors are controlled to meet the person’s needs (Chapter 18).
See Focus on Communication: Comfort.
 OBRA requirements
OBRA requirements
The Omnibus Budget Reconciliation Act of 1987 (OBRA) and the Centers for Medicare & Medicaid Services (CMS) require care that promotes well-being. Comfort, rest, and sleep are needed for physical, emotional, and mental well-being. Rooms are designed and equipped for comfort.
• No more than 4 persons in a room
• A suspended curtain that goes around the bed for privacy
• A bed of proper height and size for the person
• A clean, comfortable mattress
• Linens (sheets, blankets, spreads) that suit the weather and climate
• A room temperature between 71° and 81° F (Fahrenheit)
• Adequate ventilation and room humidity
Pain
Pain or discomfort means to ache, hurt, or be sore. It is unpleasant. Comfort and discomfort are subjective (Chapter 7). That is, you cannot see, hear, touch, or smell pain or discomfort. You must rely on what the person says. Report complaints to the nurse for the nursing process.
Pain differs for each person. What hurts to one person may ache to another. What one person calls sore, another may call aching. If a person complains of pain or discomfort, the person has pain or discomfort. Believe the person. You cannot see, hear, feel, or smell the person’s pain or discomfort.
Pain is a warning from the body. Often called the fifth vital sign (Chapter 31), pain signals tissue damage. Pain often causes the person to seek health care.
See Focus on Communication: Pain.
Types of pain
There are different types of pain:
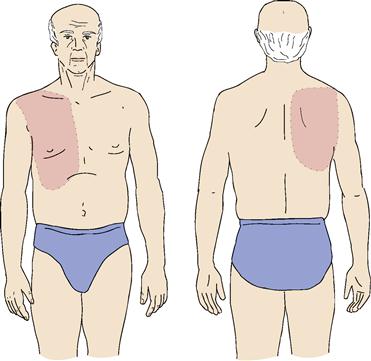
• Radiating pain is felt at the site of tissue damage and in nearby areas. Pain from a heart attack is often felt in the left chest, left jaw, left shoulder, and left arm. Gallbladder disease can cause pain in the right upper abdomen, the back, and the right shoulder (Fig. 27-1).
Factors affecting pain
A person may handle pain well one time and poorly the next time. Many factors affect reactions to pain.
Past experience
We learn from past experiences. They help us know what to do or what to expect. Whether it is going to school, driving, taking a test, shopping, having a baby, or caring for children, the past prepares us for like events at another time. We also learn from the experiences of family and friends.
A person may have had pain before. The severity of pain, its cause, how long it lasted, and if relief occurred all affect the current response to pain. Knowing what to expect can help or hinder how the person handles pain.
Some people have not had pain. When it occurs, pain can cause fear and anxiety. They can make pain worse.
Anxiety
Anxiety relates to feelings of fear, dread, worry, and concern. The person is uneasy and tense. The person may feel troubled or threatened. Or the person may sense danger. Something is wrong but the person does not know what or why.
Pain and anxiety are related. Pain can cause anxiety. Anxiety increases how much pain is felt. Reducing anxiety helps lessen pain. For example, the nurse explains to Mr. Smith about pain after surgery. The nurse also explains that drugs are given for pain relief. Mr. Smith knows the cause of pain and what to expect. This helps lessen anxiety and therefore the amount of pain felt.
Rest and sleep
Rest and sleep restore energy. They reduce body demands. The body repairs itself. Lack of needed rest and sleep affects thinking and coping with daily life. Sleep and rest needs increase with illness and injury. Pain seems worse when tired or restless. Also, the person tends to focus on pain when tired and unable to rest or sleep.
Attention
The more a person thinks about the pain, the worse it seems. Sometimes severe pain is all the person thinks about. Even mild pain can seem worse if the person thinks about it all the time.
Pain often seems worse at night. Activity is less, and it is quiet. There are no visitors. The radio or TV is off. Others are asleep. When unable to sleep, the person has time to think about the pain.
Personal and family duties
Personal and family duties affect pain responses. Often pain is ignored when there are children to care for. Some people go to work with pain. Others deny pain if a serious illness is feared. The illness can interfere with a job, going to school, or caring for children, a partner, or ill parents.
The value or meaning of pain
To some people, pain is a sign of weakness. It may mean a serious illness and the need for painful tests and treatments. Therefore pain is ignored or denied. Sometimes pain gives pleasure. The pain of childbirth is one example.
For some persons, pain means not having to work or assume daily routines. Pain is used to avoid certain people or things. The pain is useful. Some people like doting and pampering by others. The person values and wants such attention.
Support from others
Dealing with pain is often easier when family and friends offer comfort and support. The pain of childbirth is easier when a loving father gives support and encouragement. A child bears pain much better when comforted by a caring parent or family member. The use of touch by a valued person is very comforting. Just being nearby also helps.
Some people do not have caring family or friends. They deal with pain alone. Being alone can increase anxiety. The person has more time to think about the pain. Facing pain alone is hard for everyone, especially children and older persons.
Culture
Culture affects pain responses. In some cultures, the person in pain is stoic. To be stoic means to show no reaction to joy, sorrow, pleasure, or pain. Strong verbal and nonverbal reactions to pain are seen in other cultures. See Caring About Culture: Pain Reactions.
![]() OBRA requires that the care planning process reflect the person’s culture. Non–English-speaking persons may have problems describing pain. The center must know who these persons are. Someone must be available to interpret the person’s needs. All persons have the right to be comfortable and as pain-free as possible.
OBRA requires that the care planning process reflect the person’s culture. Non–English-speaking persons may have problems describing pain. The center must know who these persons are. Someone must be available to interpret the person’s needs. All persons have the right to be comfortable and as pain-free as possible.
Illness
Some diseases cause decreased pain sensations. Central nervous system disorders are examples. The person may not feel pain. Or it may not feel severe. The person is at risk for undetected disease or injury. Pain occurs with tissue damage. The pain signals illness or injury. If pain is not felt, the person does not know to seek health care.
Age
Some older persons have many painful health problems. Chronic pain may mask new pain. Older persons may ignore or deny new pain. They may think it relates to a known health problem. Older persons often deny or ignore pain because of what it may mean.
Older persons may have decreased pain sensations. They may not feel pain. Or it may not feel severe. The person is at risk for undetected disease or injury. Pain occurs with tissue damage. The pain signals illness or injury. If pain is not felt, the person does not know to seek health care.
Thinking and reasoning are affected in some older persons. Some cannot verbally communicate pain. Increased confusion, grimacing, or restlessness may signal pain. So may changes in usual behavior. You must be alert for the signs of pain. Always report changes in the person’s behavior.
See Residents With Dementia: Factors Affecting Pain—Age.
Signs and symptoms
You cannot see, hear, feel, or smell the person’s pain. You must rely on what the person tells you. Promptly report any information you collect about pain. Write down what the person says. Use the person’s exact words when reporting and recording. The nurse needs this information to assess the person’s pain:
• Location. Where is the pain? Ask the person to point to the area of pain (Fig. 27-2). Pain can radiate. Ask the person if the pain is anywhere else and to point to those areas.
• Onset and duration. When did the pain start? How long has it lasted?
• Intensity. Is the pain mild, moderate, or severe? Ask the person to rate the pain on a scale of 1 to 10, with 10 as the most severe (Fig. 27-3). Or use the Wong-Baker Faces Pain Rating Scale (Fig. 27-4). Designed for children, the scale is useful for persons of all ages. To use the scale, tell the person that each face shows how a person is feeling. Read the description for each face. Then ask the person to choose the face that best describes how he or she feels.
• Description. Ask the person to describe the pain. If the person cannot describe the pain, offer some of the words listed in Box 27-1.
• Factors affecting pain. Ask the person what makes the pain better. Also ask what makes it worse.
• Vital signs. Measure the person’s pulse, respirations, and blood pressure (Chapter 31). Increases in these vital signs often occur with acute pain. Vital signs may be normal with chronic pain.
• Other signs and symptoms. Does the person have other symptoms? Box 27-2 lists the signs and symptoms that often occur with pain.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree