Drugs Used to Treat Peripheral Vascular Disease
Objectives
1 Differentiate between peripheral vascular disease and Raynaud’s disease.
2 Describe the baseline assessments needed to evaluate a patient with peripheral vascular disease.
4 Identify the systemic effects to expect when peripheral vasodilating agents are administered.
5 Explain why hypotension and tachycardia occur frequently with the use of peripheral vasodilators.
6 Develop measurable objectives for the education of patients with peripheral vascular disease.
7 Cite both pharmacologic and nonpharmacologic goals of the treatment for peripheral vascular disease.
Key Terms
arteriosclerosis obliterans (
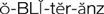 ) (p. 416)
) (p. 416)
intermittent claudication (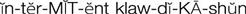 ) (p. 416)
) (p. 416)
paresthesias ( ) (p. 416)
) (p. 416)
Raynaud’s disease ( ) (p. 416)
) (p. 416)
vasospasm (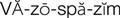 ) (p. 416)
) (p. 416)
Peripheral Vascular Disease
![]() http://evolve.elsevier.com/Clayton
http://evolve.elsevier.com/Clayton
The term peripheral vascular disease can be applied to a variety of illnesses associated with blood vessels outside the heart, but it generally refers to diseases of the blood vessels of the arms and legs (the extremities). These illnesses can be subdivided into two types based on arterial or venous origin: (1) peripheral arterial diseases; and (2) venous disorders, such as acute deep vein thrombosis (see Chapter 27). The arterial disorders are subdivided into those that result from arterial narrowing and occlusion (obstructive) and those caused by arterial spasm (vasospastic).
The most common form of obstructive arterial disease is arteriosclerosis obliterans, also called atherosclerosis obliterans. It results from atherosclerotic plaque formation, with narrowing of the lower aorta and the major arteries that provide circulation to the legs. As with atherosclerosis of the coronary arteries, the risk factors that play an important role in the development of this disease are high levels of low-density lipoprotein cholesterol (LDL-C), hypertension, cigarette smoking, low levels of high-density lipoprotein cholesterol (HDL-C), and diabetes mellitus.
Patients tend to remain free of symptoms until there is significant narrowing (75% to 90%) in key locations of the major arteries and arterioles of the legs. The typical pain pattern described is one of aching, cramping, tightness, or weakness that occurs during exercise. The primary pathophysiology is obstruction of blood flow through the arteries, resulting in ischemia to the tissues supplied by those arteries. A term commonly applied to this condition is intermittent claudication; it manifests as pain secondary to lack of oxygen to the muscles during exercise. During the early stages of symptoms, the patient finds relief by stopping the exercise for a few minutes. Without treatment, as the disease progresses over time, the arteries become obstructed, resulting in thrombosis and the potential for gangrene. Additional symptoms that develop are pain at rest, numbness, and paresthesias (numbness with a tingling sensation). The disease is often accompanied by increased blood viscosity. Physical findings on the lower extremities are reduced arterial pulsations on palpation; systolic bruits over the involved arteries; waxy, pale, and dry skin; a lower temperature of the skin of the extremity; edema; and numbness to sensation.
Peripheral vascular disease caused by arterial vasospasm is known as Raynaud’s disease, named after the man who first described the illness in 1862. It is unfortunate that, more than a century later, the pathophysiology and treatment of this condition are still not well defined. Raynaud’s disease is classified as either primary, in which the cause is unknown, or as secondary, in which other conditions contribute to the symptoms. Secondary causes are frequent exposure to cold weather, obstructive arterial disease, occupational trauma (e.g., pneumatic hammer users, pianists), and certain drugs (e.g., beta blockers, imipramine, nicotine, bromocriptine, vinblastine, clonidine). Heredity may also play a role in this disease. The onset of Raynaud’s disease is usually during the teenage years to the 40s, and it occurs four times more frequently in women.
Raynaud’s disease is thought to be caused by vasospasm (vasoconstriction of blood vessels) and subsequent ischemia of the arteries of the skin of the hands, fingers, and sometimes toes. The physiologic mechanisms that trigger the vasospasm are unknown. Sudden coldness applied to the extremity, such as cold water, can induce an attack. The signs and symptoms associated with Raynaud’s disease are numbness, tingling, a sense of skin tightness in the affected area, and blanching of the skin because of sudden vasoconstriction followed by cyanosis. As the attack subsides, vasodilation causes a redness, or rubor, to the pale skin. The skin appears normal except during spasm. During the early years of the illness, only the fingertips of both hands are involved. However, as the disease progresses, the skin on the hands is also affected by the arteriospasm.
Treatment of Peripheral Vascular Disease
The goals of treatment of arteriosclerosis obliterans are reversal of the progression of the atherosclerosis, improved blood flow, pain relief, and prevention of skin ulceration and gangrene. An important concept that must be stressed to most patients is that other diseases that they may have (e.g., diabetes, hypertension, angina, dyslipidemia) are all interrelated. Control of diet, high blood pressure, smoking, weight, and diabetes will significantly help all these diseases.
Implementation of the American Heart Association’s diet—an eating plan for healthy Americans—can arrest the progression of atherosclerosis. Lipid-lowering agents can be started if diet modifications do not successfully treat the hypercholesterolemia. A daily exercise program (usually walking) can significantly improve collateral blood circulation around areas of obstruction and reduce the frequency of intermittent claudication. Proper foot care (e.g., keeping feet warm and dry, wearing properly fitting shoes), especially if the patient has diabetes, is also extremely important to prevent ulcerative complications. Other nonpharmacologic treatments for improving blood flow to the extremities include avoiding cold, elevating the head of the bed by 12 to 16 inches, and arterial angioplasty and surgery.
Most vasospastic attacks of Raynaud’s disease can be stopped by avoiding cold temperatures, emotional stress, tobacco, and drugs that are known to induce attacks. Keeping the hands and feet warm with gloves and socks and using foam wraparounds when handling iced beverages can reduce exposure to cold.
Drug Therapy for Peripheral Vascular Disease
Actions
As the causes of peripheral vascular disease have come to be better understood, clinical studies have defined which pharmacologic therapies are truly successful. It has been shown that nonpharmacologic treatment of arteriosclerosis obliterans is substantially more successful in treating the underlying pathologic condition. Pentoxifylline has had modest success; it is classified as a hemorheologic agent. It acts by enhancing red blood cell flexibility, which reduces blood viscosity, thus providing better oxygenation to muscle tissue to stop intermittent claudication. Vasodilator therapy, the mainstay of treatment until the 1980s, has little long-term benefit in most cases. A new approach to treatment became available in the form of the platelet aggregation inhibitor cilostazol. Clopidogrel, a newer platelet aggregation inhibitor, is also approved for the treatment of peripheral arterial disease (see Chapter 27). When drug therapy for Raynaud’s disease is required, such as when the disease interferes with an individual’s ability to work, agents with a vasodilating effect are used.
Uses
Pentoxifylline and cilostazol are the only agents approved by the U.S. Food and Drug Administration (FDA) that are specifically indicated for the treatment of intermittent claudication caused by chronic occlusive arterial disease of the limbs. Classes of drugs that have been somewhat successful in treating Raynaud’s disease are calcium channel blockers, adrenergic antagonists, angiotensin-converting enzyme inhibitors, and direct vasodilators.
The three calcium ion antagonists studied for the treatment of Raynaud’s disease are diltiazem, verapamil, and nifedipine. Of the three, nifedipine has had the greatest success in reducing the frequency of vasospastic attack in about two thirds of patients.
Adrenergic antagonists (e.g., prazosin, reserpine, methyldopa) have been used for many years for the treatment of Raynaud’s disease. Unfortunately, treatment has been only moderately successful, and many adverse effects are associated with the use of these drugs.
The angiotensin-converting enzyme (ACE) inhibitors cause an increase in bradykinin, a potent vasodilator. Captopril has been the most extensively tested, and it has been shown to reduce the frequency and severity of attacks.
For more than 50 years, nitroglycerin, a direct vasodilator, has been applied as an ointment base to the hands of patients with Raynaud’s disease. The treatment reduces the frequency and severity of attacks, but the adverse effects of dizziness, headache, and postural hypotension limit its use.
Other vasodilators (e.g., papaverine, isoxsuprine) have been used extensively over the years to treat Reynaud’s disease, but these agents have not undergone testing in controlled studies. However, they are still used occasionally as adjunctive therapy to treat peripheral vascular diseases.
 Nursing Implications for Peripheral Vascular Disease Therapy
Nursing Implications for Peripheral Vascular Disease Therapy
Assessment
A baseline assessment of the patient should be completed that includes the following for evaluating the history and degree of oxygenation existing in the extremities. Subsequent regular assessments should be performed for comparison and analysis of therapeutic effectiveness or lack of response to any treatments initiated.
History of Risk Factors.
Determine the patient’s age, gender, and race, and obtain a family history of the incidence of symptoms of peripheral vascular disease, hypertension, and cardiac disease.
Impotence.
If the patient is male, has he experienced impotence?
Hypertension.
Take the patient’s blood pressure in sitting and supine positions daily. Ask about medications that have been prescribed. Are the medications being taken regularly? If not, why not?
Smoking.
Obtain a history of the number of cigarettes or cigars that the patient smokes daily; include other sources of nicotine, such as chewing tobacco and replacement therapy. How long has the person smoked? Has the person ever tried to stop smoking? Ask if the patient understands the effect of smoking on the vascular system. How does the individual feel about modifying his or her smoking habit?
Dietary Habits
Glucose Intolerance.
Ask specific questions about whether the individual currently has or has ever had an elevated serum glucose (blood sugar) level. If yes, what dietary modifications have been made? How successful have they been? What medications are being taken for the elevated serum glucose level (e.g., oral hypoglycemic agents, insulin)?
Elevated Serum Lipid Levels.
Find out whether the patient is aware of having elevated lipid, triglyceride, or cholesterol levels. If any of these levels are elevated, what measures has the patient tried for reduction, and what effect have the interventions had on the blood levels during subsequent examinations? Review any laboratory data available (e.g., LDL, very low-density lipoprotein [VLDL], liver function tests, clotting time).
Infection.
Has the individual developed any slow-to-heal or nonhealing sores?
Obesity.
Weigh the patient. Ask about any recent weight gains or losses and whether it was intentional or unintentional.
Psychomotor Functions
Type of Lifestyle.
Ask the patient to describe his or her exercise level in terms of amount (e.g., walking three blocks), intensity (e.g., how long does it take to walk three blocks?), and frequency (e.g., walking every other day). Is the patient’s job physically demanding or sedentary?
Psychological Stress.
How much stress does the individual estimate having in his or her life? How does the individual cope with stressful situations at home and at work?
Assessment of Tissue
Oxygenation.
Observe the color of each hand, finger, leg, and foot; report cyanosis or reddish-blue areas. Does the patient have dependent cyanosis (cyanosis when the legs are in the dependent position)? Examine the skin of the extremities for any signs of ulceration.
Temperature.
Feel the temperature in each hand, finger, leg, and foot. Report any paleness or coldness. (NOTE: These symptoms will be increased if the limb is elevated above the level of the heart.)
Edema.
Assess, record, and report edema and its extent, and determine whether it is relieved or unchanged when the limb is dependent.
Peripheral Pulses.
Record the pedal and radial pulses (Figure 26-1) at least every 4 hours if circulatory impairment is found in that limb. Compare findings among the extremities and report diminished or absent pulses immediately. When pulses are difficult to palpate or absent, a Doppler ultrasound device may help determine peripheral blood flow.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


