The Child with a Respiratory Disorder
Objectives
1. Define each key term listed.
2. Distinguish the differences between the respiratory tract of the infant and that of the adult.
3. Review the signs and symptoms of respiratory distress in infants and children.
4. Discuss the nursing care of a child with croup, pneumonia, or respiratory syncytial virus.
5. Recognize the precautions involved in the care of a child diagnosed with epiglottitis.
6. Compare bed rest for a toddler with bed rest for an adult.
7. Describe smoke inhalation injury as it relates to delivery of nursing care.
8. Discuss the postoperative care of a 5-year-old who has had a tonsillectomy.
9. Recall the characteristic manifestations of allergic rhinitis.
10. Discuss how sinusitis in children is different from that in adults.
11. Assess the control of environmental exposure to allergens in the home of a child with asthma.
12. Express five goals of asthma therapy.
13. Interpret the role of sports and physical exercise for the asthmatic child.
14. Recall four nursing goals in the care of a child with cystic fibrosis.
15. Devise a nursing care plan for the child with cystic fibrosis, including family interventions.
16. Review the prevention of bronchopulmonary dysplasia.
Key Terms
alveoli (ăl-VĒ-ō-lī, p. 591)
atelectasis (ă-tĕ-LĔK-tă-sĭs, p. 602)
carbon dioxide narcosis (p. 584)
clubbing of the fingers (p. 602)
coryza (kō-RĪ-ză, p. 585)
dysphagia (dĭs-FĀ-jhă, p. 586)
laryngeal spasm (p. 588)
meconium ileus (p. 603)
orthopnea (ŏr-thŏp-NĒ-ă, p. 588)
pursed-lip breathing (p. 603)
reactive airway disease (RAD) (p. 591)
stridor (STRĪ-dŏr, p. 587)
surfactant (sŭr-FĂK-tănt, p. 583)
tachypnea (tăk-ĭp-NĒ-ă, p. 590)
ventilation (p. 584)
![]() http://evolve.elsevier.com/Leifer
http://evolve.elsevier.com/Leifer
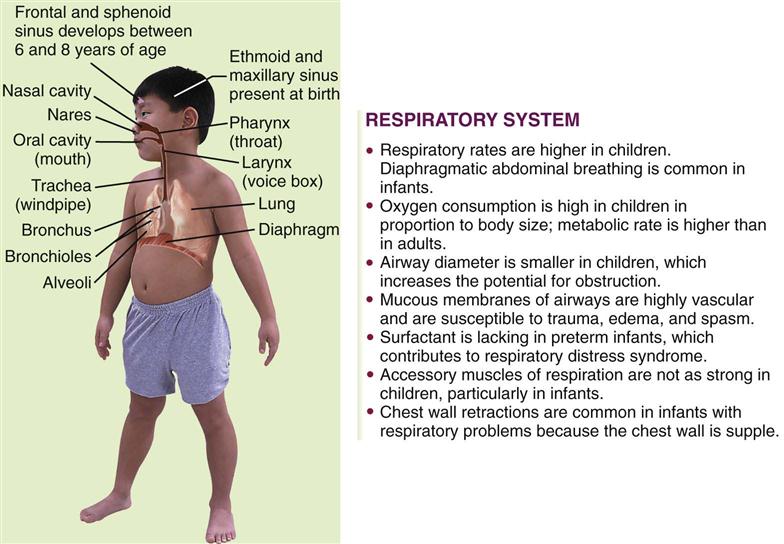
The Respiratory System
Development of the Respiratory Tract
Pulmonary structures differentiate in an orderly fashion during fetal life. This makes it possible to determine at what point a particular defect may have occurred. The laryngotracheal groove appears at 2 to 4 weeks of gestation. The trachea and the esophagus originate as one hollow tube; gradually, by 4 weeks of gestation, a septum forms to completely separate them. If the septum fails to form completely, a tracheoesophageal fistula occurs (see Chapter 28). By the seventh week of fetal life the diaphragm forms and separates the chest from the abdominal cavity. If the diaphragm fails to close completely, a diaphragmatic hernia allows the abdominal contents (intestines, spleen, and stomach) to enter the chest cavity and prevents the lungs from expanding fully. Alveoli and capillaries, which are necessary for gas exchange in the human body, are formed between 24 and 28 weeks of gestation.
At the twenty-fourth week the formed alveolar cells begin to produce surfactant. Surfactant is composed of lecithin and sphingomyelin and prevents the alveoli from collapsing during respirations after birth. A premature birth is accompanied by problems with respiratory gas exchange. During fetal life the lungs are filled with a fluid that has a low surface tension and viscosity; this is rapidly absorbed after birth. Spontaneous respiratory movements occur in the fetus, although gas exchange occurs via placental circulation. When surfactant is present in the lungs, the respiratory movements force some of the surfactant into the amniotic fluid. At about 35 weeks of gestation, the lecithin component is twice that of the sphingomyelin component. The analysis of the lecithin/sphingomyelin ratio (L/S ratio) by amniocentesis (see Table 5-1) is one method of determining fetal maturity and the ability of the fetus to survive outside the uterus.
Normal Respiration
The process of normal respiration is described in Figure 25-1.
Ventilation
Ventilation, the process of breathing air into and out of the lungs, is affected by several elements and their interaction with each other:
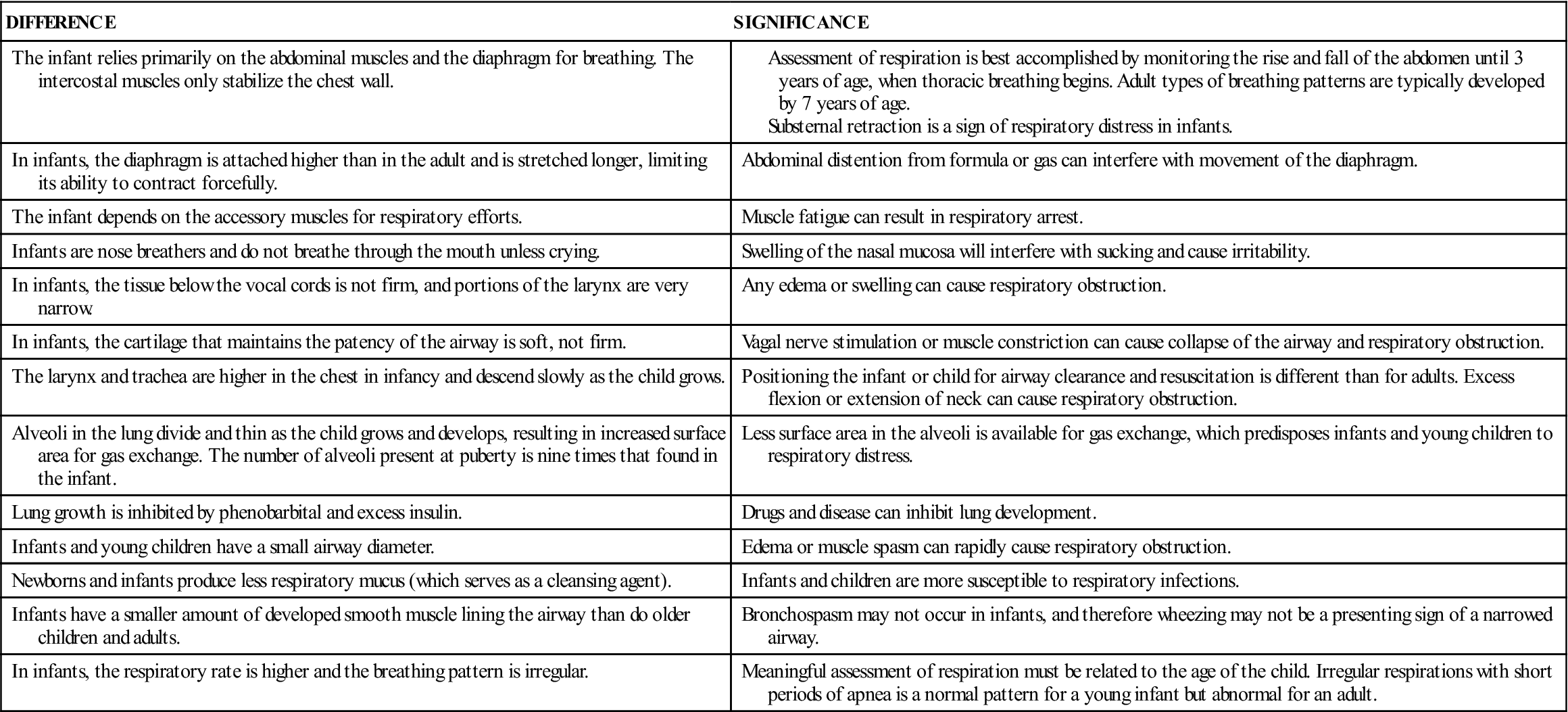
NOTE: A high carbon dioxide (CO2) level in the blood and a low O2 saturation stimulate the brain to increase the respiratory rate. In chronic lung disease, however, the receptors become tolerant to the high CO2 and low O2 concentration in the blood. Administration of supplemental oxygen increases the O2 saturation level and may result in a decreased respiratory effort (carbon dioxide narcosis), leading to respiratory failure. The differences between the respiratory tracts of the growing infant and the adult are shown in Table 25-1.
Table 25-1
Differences in the Respiratory Tracts of the Growing Infant and the Adult
Procedures that may be performed on the child with a respiratory condition include throat and nasopharyngeal cultures, bronchoscopy, lung biopsy, arterial blood gas (PaO2, PaCO2) and pH analysis, pulse oximetry, and various pulmonary function tests (PFTs). Chest x-ray films, computed tomography, radioisotope scan, bronchogram, and angiography may prove useful, depending on symptoms. The inspection, percussion, and auscultation procedures performed by the nurse are of utmost value in data collection.
Disorders and Dysfunction of the Respiratory System
Nasopharyngitis
Pathophysiology.
A cold, also known as acute coryza, is the most common infection of the respiratory tract. It can be caused by a number of viruses, principally the rhinoviruses, which are spread from one child to another by sneezing, coughing, or direct contact. The age, state of nutrition, and general health of the child contribute to the susceptibility level.
The rhinovirus is spread by contact with contaminated fingers that touch the conjunctiva of the eyes or the mucous membranes of the mouth. Routine handwashing practices, especially before rubbing the nose or sucking the fingers, can prevent the spread of the common cold.
The common cold differs from allergic rhinitis in that a child who has allergic rhinitis has no fever, no purulent nasal discharge, and no reddened mucous membranes. Sneezing, watery eyes, and itching of the skin are the primary manifestations of allergic rhinitis. In the older child or adolescent, persistent nasopharyngitis may be related to inhaled cocaine or other drug abuse.
Manifestations.
The symptoms of a cold in an infant or small child are different from those in an adult. Children’s air passages are smaller and more easily obstructed. The virus causes inflammation and edema of the membranes of the upper respiratory tract, which damages cilia and prevents the drainage of mucus. Fever as high as 40° C (104° F) is not uncommon in children under 3 years of age. Nasal discharge, irritability, sore throat, cough, and general discomfort are present, and there may be vomiting and diarrhea. The diagnosis is complicated by the fact that many infectious diseases resemble the common cold during their onset. Complications of a cold include bronchitis, pneumonitis, and ear infections.
Treatment and Nursing Care.
There is no cure for the common cold. Treatment should begin early, when a cold is suspected. The following treatment is designed to relieve symptoms:
• Clear airways: Congested nasal passages cause discomfort and impede nursing or sucking of formula. Because fluid consumption is essential to prevent fever and dehydration, the airways must be cleared before feeding and before bedtime to provide a restful sleep. The nurse can teach the parents that instilling a few drops of saline solution into the nose and then suctioning with a bulb syringe (Skill 12-2) is the best way to clear the nostrils. Medicated nosedrops can be irritating to the mucosa of a young child’s nasal passages. Use of nosedrops with an oily base should be avoided because they are readily aspirated and can cause respiratory problems. Rebound congestion can be avoided by limiting the use of medicated nosedrops to no more than 3 days. Use of over-the-counter combination cold remedies should be avoided. Contents on the label should be checked for safe dosage.
Moist air soothes the inflamed nose and throat. An electric cold air humidifier is safe and convenient. It must be cleaned and disinfected daily. If a great deal of moisture is indicated (as in croup), the infant may be taken to a small room, such as the bathroom, and the hot water faucets or shower can be turned on to produce sufficient steam.
The older child is taught the proper way to remove nasal secretions from the nose. The mouth is opened slightly, and secretions are gently blown through both nostrils at the same time. This method prevents the infection from being forced into the eustachian tubes. Children must be taught to cover the mouth and nose when sneezing and to wash their hands afterward. Tissues must be properly discarded. Antibiotics are not effective against the common cold because it is viral in origin.
Otitis media is an inflammation of the middle ear. The middle ear is connected to the throat by the eustachian tube, which provides drainage of middle ear secretions into the nasopharynx and equalizes pressure between the middle ear and the outside atmosphere. When the lining of the eustachian tube becomes infected as a complication of nasopharyngitis, otitis media often develops, usually following an upper respiratory infection. Infants are more prone to middle ear infections because their eustachian tubes are shorter, straighter, and wider than those of older children or adults. For a detailed discussion of otitis media, see Chapter 23.
Acute Pharyngitis
Pathophysiology.
Acute pharyngitis is an inflammation of the structures in the throat. This infection is common among children between 5 and 15 years of age. In 80% of cases the causative organism is a virus. Group A beta-hemolytic streptococcus (strep throat) occurs in 20% of the cases. The bacterium Haemophilus influenzae is common in children under 3 years of age.
Manifestations, Treatment, and Nursing Care.
Symptoms include fever, malaise, dysphagia (dys, “difficult,” and phagia, “swallowing”), and anorexia. It is difficult to distinguish viral from bacterial types by symptoms only. Conjunctivitis, rhinitis, cough, and hoarseness with a gradual onset and persisting no longer than 5 days are characteristic of viral pharyngitis. In a child over 2 years of age, streptococcal pharyngitis characteristically includes high fever (40° C [104° F]) and difficulty in swallowing, and it may last longer than 1 week. A strep throat is determined by throat culture. When the culture is positive, antimicrobial therapy such as penicillin is administered orally for 10 days. Compliance may be a problem; therefore the nurse carefully explains to parents the need for the child to finish all of the medication. Erythromycin may be prescribed if the child is allergic to penicillin. Acetaminophen may be taken to relieve soreness of the throat. If the child is old enough to gargle, a solution of warm water and salt may be used.
Prompt treatment of strep throat is important to prevent serious complications such as rheumatic fever, glomerulonephritis, peritonsillar abscess, otitis media, mastoiditis, meningitis, osteomyelitis, or pneumonia. The persistence of a positive streptococcal culture after careful follow-up and therapy may indicate that the child is a group A beta-hemolytic streptococcus carrier. However, it may also mean that the child did not complete the 10-day course of medication or that a drug-resistant organism has evolved. The child with strep throat is no longer infectious to others once drug therapy has begun and fever has decreased.
Sinusitis in Children
The frontal sinuses are present at 8 years of age but may not be fully developed until age 18. Some ethmoid sinus cells are present at birth. The sphenoid sinus is present by 3 years of age and is fully developed by age 12. The maxillary sinuses are present at birth and develop as long as teeth are erupting. The proximity of this sinus to the tooth roots often results in tooth pain when the sinus is infected. The maxillary and ethmoid sinuses are most often involved in childhood sinusitis. Therefore the signs and symptoms of sinusitis in children are different from those in adults, depending on the age of the child and which sinus is fully developed. An acute sinusitis is suspected when an upper respiratory infection lasts longer than 10 days, with a daytime cough. Halitosis is often present. Untreated sinusitis can lead to periorbital cellulitis, because the infection spreads from the ethmoid sinus to the subperiosteal space around the eye. Treatment involves a 10- to 14-day course of antibiotic therapy.
Croup Syndromes
Pathophysiology.
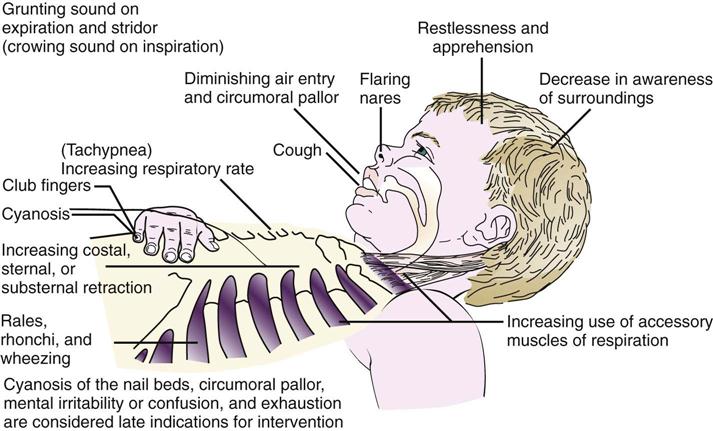
Croup is a general term applied to a number of conditions whose chief symptom is a “barking” (croupy) cough and varying degrees of inspiratory stridor (a harsh, high-pitched sound). When the larynx is involved, the clinical picture becomes more intense because of possible alterations in respiratory status, such as airway obstruction, acute respiratory failure, and hypoxia (Figure 25-2). Acute spasmodic laryngitis is the milder form of the syndrome. Acute laryngotracheobronchitis is the most common. It is also referred to as subglottic croup because edema occurs below the vocal cords. Croup can be benign or acute. Benign croup is frightening but rarely life threatening. Acute croup can develop into a respiratory emergency.
Benign Crouplike Conditions
Congenital laryngeal stridor (laryngomalacia).
Some infants are born with a weakness of the airway walls and a floppy epiglottis that causes a stridor on inspiration. There may be inspiratory retractions. The symptoms lessen when the infant is placed prone or propped in the side-lying position. Respiratory infection and crying may cause the symptoms to become frightening to the parents. The condition usually clears spontaneously as the child grows and the muscles strengthen. The nurse should provide reassurance and suggest slow, small feedings and a prone or side-lying position for the infant.
Spasmodic laryngitis (spasmodic croup).
Spasmodic croup usually occurs in children between 1 to 3 years of age and can be caused by a virus, allergy, or psychological trigger. Very often, gastroesophageal reflux (GER) will trigger an attack. Spasmodic croup has a sudden onset, usually at night, and is characterized by a barking, brassy cough and respiratory distress. The child appears anxious, and the parents become frightened. The attack lasts a few hours, and by morning the child appears normal and is in no distress. Increasing humidity and providing fluids are helpful treatment measures.
Acute Croup
Laryngotracheobronchitis.
The viral condition laryngotracheobronchitis is manifested by edema, destruction of respiratory cilia, and exudate, resulting in respiratory obstruction. A mild upper respiratory infection usually precedes the development of a characteristic barking or brassy cough. Stridor develops, and classic symptoms of respiratory distress follow (see Figure 25-2). The infant prefers to be held upright or sit up in bed (orthopnea). Crying and agitation worsen the symptoms. Hypoxia can develop and be accompanied by tachycardia and diminished breath sounds.
Treatment and nursing care.
When the child is treated at home, parents are often instructed to increase humidity levels around the child. This can be accomplished by using an electric cold water humidifier. The humidifier must be emptied, washed, and disinfected each day to prevent the growth of microorganisms that occur in stagnant tap water. The child can also be taken into the bathroom, where the hot water in the shower is turned on to increase humidity. The child inhales the moist air, which usually relieves the respiratory distress and laryngeal spasm (constriction of laryngeal muscles).
When continuing symptoms of respiratory distress necessitate hospitalization, the child may be given nebulizer therapy or placed in a mist tent, or croupette (see Figure 22-19). The cool air, well saturated in microdroplets that can enter the small airway of a child, causes mucosal cooling and vasoconstriction and relieves the respiratory obstruction and distress. However, the value of mist tent therapy in the acutely ill child is unproven. Intravenous (IV) fluids are prescribed to prevent dehydration and to decrease the risk of vomiting and aspiration that can occur after a coughing episode. Organization of care is essential to enable the child to have long periods of rest. The child is placed on a cardiorespiratory monitor (CRM), and the vital signs are observed closely. Oxygen is given to reduce hypoxia (see Chapter 22). Oxygen saturation is monitored, and saturation levels are maintained above 90% (see Skill 13-1 for sensor application).
Opiates are contraindicated because they depress respiration. Sedatives are contraindicated because increased restlessness is a primary sign of increased respiratory obstruction, and sedatives can mask signs of restlessness. Nebulized epinephrine may be used to relieve the symptoms of respiratory obstruction (Figure 25-3). Corticosteroids are often prescribed to reduce the edema caused by inflammation and to prevent further destruction of ciliated epithelium in children hospitalized with croup, providing there is no history of recent exposure to varicella (chickenpox) (Lenney et al., 2009).
Epiglottitis
Pathophysiology.
Epiglottitis is a swelling of the tissues above the vocal cords, that is, supraglottic swelling. This results in narrowing of the airway inlet, with the possibility of total obstruction. It is caused by H. influenzae type B and most often occurs in children 3 to 6 years of age. It can occur in any season. The course is rapid and progressive. Epiglottitis is a life-threatening medical emergency. Blood gases fluctuate, and there is leukocytosis.
Manifestations.
The onset of epiglottitis is abrupt, and the child presents with classic symptoms. The child insists on sitting up, leans forward with the mouth open, and drools saliva because of the difficulty in swallowing. The child appears wide-eyed, anxious, and restless, and he or she may emit a froglike croaking sound on inspiration. Cough is absent. Inspection of the throat shows an enlarged, reddened edematous epiglottis much like a “beefy-red thumb.” However, the examining tongue blade may trigger a laryngospasm and result in sudden respiratory arrest.
Treatment.
The treatment of choice is immediate tracheotomy or endotracheal intubation and oxygen to prevent hypoxia, brain damage, and sudden death caused by respiratory arrest. Parenteral antibiotic therapy usually results in a dramatic improvement within a few days.
Prevention.
The AAP recommends that H. influenzae type B conjugate vaccines be administered beginning at 2 months of age as part of a regular immunization program for all children. This type of program decreases the incidence of acute epiglottitis in children.
Bronchitis
Pathophysiology.
A study of the respiratory system reveals that the air tubes leading to the lungs resemble an upside-down tree. The trachea is the main trunk, with the bronchi, bronchioles, and alveoli as branches. These passages proceed from large to small and are lined with a continuous membrane. If there is an infection of the bronchial tree, it is seldom confined to one area but more often involves other structures.
Acute bronchitis is an infection of the bronchi. It seldom occurs as a primary infection but is usually secondary to a cold or other communicable disease. It is caused by a variety of organisms. Poor nutrition, allergy, and chronic infection of the respiratory tract may precipitate this condition. Most patients are under 4 years of age.
Manifestations.
The gradual onset of an unproductive “hacking” cough is preceded by an upper respiratory infection, or cold. The cough may become productive with purulent sputum. Children under 7 years of age cannot voluntarily cough and usually swallow their sputum.
Treatment.
The use of cough suppressants before bedtime may be helpful in promoting restful sleep. Antihistamines, expectorants, and antibiotics are usually not helpful. Most children recover uneventfully with symptomatic care at home.
Bronchiolitis
Pathophysiology.
Acute bronchiolitis is a viral infection of the small airways (bronchioles) in the lower respiratory tract. It occurs in infants and children 6 months to 2 years of age, with a peak at 6 months of age. The small diameter of the bronchioles in the infant are susceptible to obstruction when inflammation results in edema and excess mucus. The obstruction often leads to atelectasis. The gas exchange in the lungs becomes impaired, and hypoxia can occur.
Manifestations.
An upper respiratory infection or cold with a mild fever and serous (clear) nasal discharge is followed by the development of a wheezing cough and signs of respiratory distress. The increase in respiratory rate interferes with successful feeding, and the infant becomes irritable and dehydrated. The respiratory syncytial virus (RSV) is the causative organism in 50% of cases in infants. An apneic episode is usually the cause of hospitalization. Infants who have bronchiolitis may develop a hyperreactive airway or asthma later in life.
Treatment and Nursing Care.
The treatment of an infant with bronchiolitis is symptomatic and similar to that of the child with croup. A semi- Fowler’s position with a slightly hyperextended neck facilitates respirations. Oral feedings are often supplemented by IV fluids. Intake and output are recorded. Bronchodilating aerosol therapy and high-humidity tents are prescribed. Frequent assessment of vital signs and monitoring of oxygen saturation levels are essential.
Respiratory Syncytial Virus
Respiratory syncytial virus (RSV) is responsible for 50% of cases of bronchiolitis in infants and young children and is the most common cause of viral pneumonia. RSV is the single most important respiratory pathogen in infancy. RSV occurs worldwide and causes annual epidemics during the winter months. Most children are infected with RSV before their second birthday, and reinfection is common, especially in children attending day care centers. Infants between 2 and 7 months of age can become seriously ill with this condition because their airways are so small and prone to obstruction by the thick mucus produced. Older children and adults are not as seriously ill and continue to go to work or school, becoming carriers and spreading the infection.
Transmission.
RSV is spread by direct contact with respiratory secretions, usually by contaminated hands to the mucous membranes (eyes, mouth, nose). RSV survives for more than 6 hours on countertops, tissues, and soap bars. RSV is not spread via the airborne route. The incubation period is approximately 4 days.
Hospital-acquired infection can be a major problem because caregivers may be carrying the organism. For this reason, an infant diagnosed with RSV infection is placed on transmission-based contact isolation precautions to prevent the spread of RSV to other sick children.
RSV immunoglobulin may be used for preterm newborns with bronchopulmonary dysplasia who are at risk for infection.
Diagnosis.
An examination of nasopharyngeal washings for RSV antigens can be done while the child waits in the admitting unit so that the diagnosis is established before the infant is admitted to the pediatric unit.
Prevention.
Prevention of RSV is available via a monoclonal antibody, palivizumab (Synagis), given in monthly intramuscular injections. This medication is started at the onset of RSV season and terminated at the end of the season (usually November through March). The AAP practice guidelines state that candidates for preventive therapy include infants with bronchopulmonary dysplasia, severe immunodeficiencies, or significant congenital heart disease and those on continuous mechanical respiratory support (Meissner & Bocchini, 2009). The powder form of palivizumab should be administered within 6 hours of reconstitution because it is preservative free.
Treatment and Nursing Care.
The care of infants with RSV infection should be assigned to personnel who are not caring for patients at high risk for adverse response to RSV. Infection prevention and control techniques (see Appendix A) are used to prevent the spread of infection to others on the unit. Contact isolation precautions are used to prevent fomite spread. Frequent handwashing is essential. Liquid soap dispensers should be available at the sink, because the organism survives for a long time on a dry bar of soap.
Support of the Infant and Family.
Effective communication skills are necessary to provide support for parents of the infant who is seriously ill. The parent can be familiarized with the mist tent and encouraged to participate in the care and feeding of the infant. Adults who have RSV can shed the virus for 1 week after the infection, and precautions should be taken if that adult is caring for infants (see Appendix A for infection prevention and control precautions).
Symptomatic Care.
An ineffective breathing pattern is the priority nursing diagnosis for an infant hospitalized with RSV infection. Reporting tachypnea (increased respiration) and tachycardia (increased heart rate) is essential because these vital sign changes may be indicative of hypoxemia. It is also important to auscultate breath sounds and report wheezing, rales, or rhonchi. A child who has been wheezing and suddenly has a “quiet chest” on auscultation may be at risk for respiratory arrest. The higher-pitched the wheeze, the more constricted the airway. Signs of respiratory distress should be assessed and reported. Oxygen saturation levels are monitored, and oxygen is administered at levels needed to maintain a minimum of 90% to 95% saturation. Suctioning of mucus may be necessary to maintain a patent airway. Monitoring IV fluids and recording intake and output are essential to prevent dehydration. Urine output should be a minimum of 1 to 2 mL/kg/hr for infants and children. Pedialyte or Ricelyte are examples of clear liquid electrolyte formulas prescribed for infants at risk of dehydration. The child should be weighed daily to detect early signs of dehydration. Inhaled bronchodilators or steroids are not helpful with RSV infections.
Antiviral Medication.
Antiviral medication such as ribavirin (Virazole) may be prescribed for use with severely ill infants or infants who have heart or lung problems that place them at high risk for serious complications. The medication has been found to be effective in the treatment of RSV infection but is rarely used prophylactically because of its serious side effects. The medication is administered by fine-droplet aerosol mist while the infant is in a mist tent. It is administered 18 to 24 hours a day for a minimum of 3 days. If the infant is on a ventilator, the nurse must monitor the ventilator tubes, which may be warped by ribavirin. Caregivers and visitors who are of childbearing age, pregnant, or breastfeeding should not care for infants receiving ribavirin, because teratogenic effects have been reported. The ribavirin mist can cause precipitation on the surface of plastics, and caregivers with contact lenses may develop conjunctivitis because of the lens changes this causes. When providing care to an infant receiving ribavirin therapy, the nurse should turn off the nebulizer and allow the mist to settle before opening the mist tent and providing care. Linen removed from the bed should be slowly rolled and carefully folded to avoid releasing droplets of ribavirin into the air.
An IV immune globulin (RespiGam) may be prescribed for high-risk infants to prevent complications from RSV disease. RespiGam is administered intravenously and necessitates close observation for fluid volume overload. Routine immunizations may have to be postponed for 9 months if antiviral medication for RSV is prescribed. Intramuscular palivizumab can also be given to high-risk infants and does not interfere with mumps-measles-rubella (MMR) or varicella vaccines.
Complications.
Infants who have a small airway size and are severely ill and hospitalized with RSV infection may be at risk for wheezing and reactive airway disease (RAD) later in life. Some studies (Kliegman et al., 2007) have shown that the inflammation caused by RSV injures the respiratory epithelial cells, resulting in exposed sensory nerve fibers that respond easily to environmental irritants.
Pneumonia
Pathophysiology.
Pneumonia or pneumonitis is an inflammation of the lungs in which the alveoli (air sacs) become filled with exudate and surfactant may be reduced. The affected portion of the lung does not receive enough air. Breathing is shallow. As a result, the bloodstream is denied sufficient oxygen.
Pneumonia may occur as the initial or primary disease, or it may complicate another illness, in which case it is termed secondary pneumonia. There are many types of pneumonia. Classification may be by causative organism (i.e., bacterial or viral) or by the part of the respiratory system involved (i.e., lobar or bronchial). Group B streptococci are the most common cause of pneumonia in newborns, whereas Chlamydia are the most common cause of pneumonia in infants 3 weeks to 3 months of age. The incidence of H. influenzae type B infection has been decreasing with current immunization programs. RSV, rhinovirus, adenovirus, and pneumococcus are other organisms that are responsible for pneumonia in infants and children. Immunocompromised children may develop pneumonia caused by a gram-negative organism or a fungi such as Pneumocystis jiroveci (formerly known as Pneumocystis carinii).
Toddlers often aspirate small objects such as peanuts or popcorn and develop pneumonia as a result; therefore such foods are to be discouraged for this age-group. Lipoid pneumonia occurs when the infant inhales an oil-based substance into the airways. It is less common today because children are seldom given cod liver oil or castor oil routinely, as they were in the past. Nosedrops with an oil base must not be used for children because the oil can be aspirated and cause lipoid pneumonia. A toddler who drinks kerosene may also develop a type of pneumonia. Hypostatic pneumonia may occur in patients who have poor circulation in their lungs and remain in one position too long. The child recovering from anesthesia must be turned frequently to stimulate circulation through the lungs. Early ambulation also accomplishes this.
Severe acute respiratory syndrome (SARS) is a severe type of pneumonia caused by the coronavirus (SARS-CoV). Symptoms are similar to pneumonia, but often the severity of the respiratory distress necessitates assisted ventilation and treatment in the intensive care unit (ICU). Nursing care and treatment involve supportive care. Airborne infection isolation precautions are recommended in the care and treatment of these patients (see Appendix A).
Manifestations.
The symptoms of pneumonia vary with the patient’s age and the causative organism. They may develop suddenly or may be preceded by an upper respiratory tract infection. The cough is dry at first, but it gradually becomes productive. Fever rises as high as 39.5° to 40° C (103° to 104° F) and may fluctuate widely during a 24-hour period. The respiratory rate may increase (tachypnea) to 40 to 80 breaths/min in infants and to 30 to 50 breaths/min in older children. Respirations are shallow as the child attempts to reduce the amount of chest pain. The chest pain may be caused by a pleural irritation or a musculoskeletal irritation from frequent coughing. Sternal retractions may be seen when the accessory muscles of respiration are used. The nostrils may flare. The child is listless, has a poor appetite, and tends to lie on the affected side. X-ray films confirm the diagnosis and determine whether there are complications such as atelectasis. A differential white blood cell count is routinely performed. Blood specimens show a marked increase in the number of white blood cells (16,000 to 40,000/mm3). Culture specimens may be obtained from the nose, the throat, or sputum.
Treatment.
Treatment depends on the causative organism. Antipyretics are given to reduce fever. Oxygen is administered for dyspnea or cyanosis. When this treatment is begun early, the child is less restless and does not require as many sedatives or drugs to relieve pain. Because drug therapy has become so effective, many uncomplicated cases can be treated at home. Fluid intake should be increased, particularly clear fluids and “flattened” soft drinks. Pediazole, (a combination of erythromycin ethylsuccinate and sulfisoxazole acetyl) may be prescribed for infants younger than 6 months of age, but amoxicillin is the drug of choice for children up to 5 years of age.
Rest, fluids, and a cough suppressant before bedtime are the basics of home care. Parent education concerning the need to complete all medication prescribed is essential. Tobacco use in the environment should be avoided, and the need for H. influenzae type B (Hib) immunizations is stressed. The proper use and disposal of tissues, covering the mouth during a cough, and the modeling of proper handwashing techniques are preventive measures the nurse should teach the family.
Nursing Care.
Nursing care in all types of pneumonia is basically the same. The age of the patient determines the nurse’s approach and the type of equipment used. (The newborn receives oxygen in the Isolette, whereas the older child requires a croupette or a larger tent.) Rest is an important part of the treatment. The nurse must organize care so that the child is not disturbed unnecessarily. Planned, quiet activities for the child are recommended (Pictorial Pathway 25-1).
Pictorial Pathway 25-1
Care of a Child with Pneumonia