Nutritional support and IV therapy
Objectives
• Define the key terms and key abbreviations listed in this chapter.
• Identify the reasons for nutritional support and IV therapy.
• Explain how tube feedings are given.
• Describe scheduled and continuous feedings.
• Explain how to prevent aspiration.
• Describe the comfort measures for the person with a feeding tube.
• Describe parenteral nutrition.
• Describe the IV therapy sites.
• Identify the equipment used in IV therapy.
• Describe how to assist with the IV flow rate.
• Identify the safety measures for IV therapy.
• Identify the observations to report when a person has nutritional support or IV therapy.
• Explain how to assist with nutritional support and IV therapy.
Key terms
aspiration Breathing fluid, food, vomitus, or an object into the lungs
enteral nutrition Giving nutrients into the gastro-intestinal (GI) tract (enteral) through a feeding tube
flow rate The number of drops per minute (gtt/min)
gastrostomy tube A tube inserted through a surgically created opening (stomy) in the stomach (gastro); stomach tube
gavage The process of giving a tube feeding
intravenous (IV) therapy Giving fluids through a needle or catheter inserted into a vein; IV and IV infusion
jejunostomy tube A feeding tube inserted into a surgically created opening (stomy) in the jejunum of the small intestine
naso-enteral tube A feeding tube inserted through the nose (naso) into the small bowel (enteral)
naso-gastric (NG) tube A feeding tube inserted through the nose (naso) into the stomach (gastro)
parenteral nutrition Giving nutrients through a catheter inserted into a vein; para means beyond; enteral relates to the bowel
percutaneous endoscopic gastrostomy (PEG) tube A feeding tube inserted into the stomach (gastro) through a small incision (stomy) made through (per) the skin (cutaneous); a lighted instrument (scope) is used to see inside a body cavity or organ (endo)
regurgitation The backward flow of stomach contents into the mouth
KEY ABBREVIATIONS
| GI | Gastro-intestinal |
| gtt | Drops |
| gtt/min | Drops per minute |
| IV | Intravenous |
| mL | Milliliter |
| NG | Naso-gastric |
| NPO | Nothing by mouth |
| oz | Ounce |
| PEG | Percutaneous endoscopic gastrostomy |
| TPN | Total parenteral nutrition |
Many persons cannot eat or drink because of illness, surgery, or injury. They may have chewing or swallowing problems. Aspiration is a risk. Aspiration is breathing fluid, food, vomitus, or an object into the lungs. Some persons have problems eating or refuse to eat or drink. Others cannot eat enough to meet their nutritional needs. The doctor may order nutritional support or intravenous (IV) therapy to meet food and fluid needs.
Enteral nutrition
Some persons cannot or will not ingest, chew, or swallow food. Or food cannot pass from the mouth into the esophagus and into the stomach or small intestine. Poor nutrition results. Common causes are:
• Cancer, especially cancers of the head, neck, and esophagus
• Trauma to the face, mouth, head, or neck
• Coma
• Dementia
• Nervous system disorders (Chapter 39)
• Acquired immunodeficiency syndrome (AIDS)
Enteral nutrition is giving nutrients into the gastro-intestinal (GI) tract (enteral) through a feeding tube. Gavage is the process of giving a tube feeding. Tube feedings replace or supplement normal nutrition.
Types of feeding tubes
These feeding tubes are common:
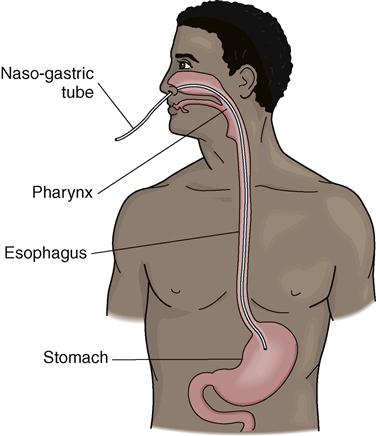
• Naso-gastric (NG) tube. A feeding tube is inserted through the nose (naso) into the stomach (gastro) (Fig. 25-1). A doctor or an RN inserts the tube.
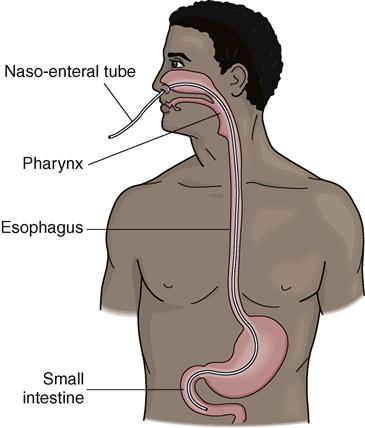
• Naso-enteral tube. A feeding tube is inserted through the nose (naso) into the small bowel (enteral) (Fig. 25-2). A doctor or RN inserts the tube.
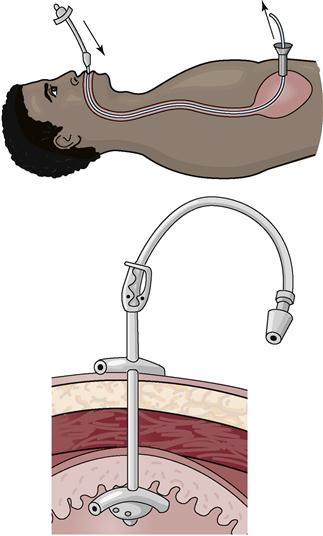
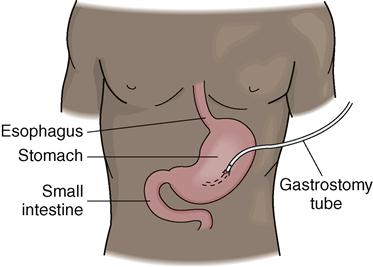
• Gastrostomy tube. Also called a stomach tube, it is inserted into the stomach (Fig. 25-3). A doctor surgically creates an opening (stomy) in the stomach (gastro).
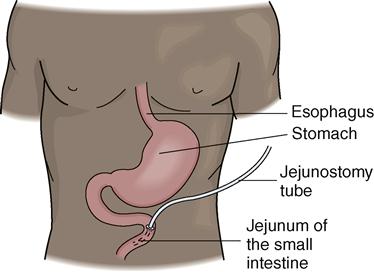
• Jejunostomy tube. A feeding tube inserted into a surgically created opening (stomy) in the jejunum of the small intestine (Fig. 25-4).
• Percutaneous endoscopic gastrostomy (PEG) tube. The doctor inserts the feeding tube with an endoscope. An endoscope is a lighted instrument (scope) used to see inside a body cavity or organ (endo). The tube is inserted through the mouth and esophagus and into the stomach. The doctor makes a small incision (stomy) through (per) the skin (cutaneous) and into the stomach (gastro). A tube is inserted into the stomach through the incision (Fig. 25-5). The endoscope allows the doctor to see correct tube placement in the stomach.
NG and naso-enteral tubes are used for short-term nutritional support—usually less than 6 weeks. Gastrostomy, jejunostomy, and PEG tubes are used for long-term nutritional support—usually longer than 6 weeks.
Formulas
The doctor orders the type of formula, the amount to give, and when to give tube feedings. Most formulas contain protein, carbohydrates, fat, vitamins, and minerals. Commercial formulas are common.
A nurse gives formula through the feeding tube. Formula is given at room temperature. Cold fluids can cause cramping.
Opened formula can remain at room temperature for about 8 hours. Microbes can grow in warm formula.
See Teamwork and Time Management: Formulas.
Feeding times
Tube feedings are given at certain times (scheduled feedings). Or they are given over a 24-hour period (continuous feedings).
Scheduled feedings
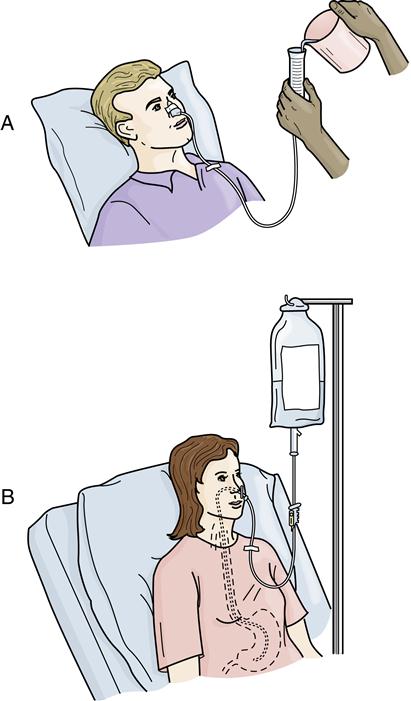
Such feedings also are called intermittent feedings. (Intermittent means to start, stop, and then start again.) Feeding times are scheduled. Four or more feedings are given each day. Usually 8 to 12 ounces (oz) (240 to 360 milliliters [mL]) are given over about 30 minutes. The frequency, amount, and time are like a normal eating pattern.
The nurse uses a syringe or a feeding bag (Fig. 25-6). The syringe attaches to the feeding tube. Connecting tubing connects the feeding bag to the tube. Formula is added to the syringe or to the feeding bag. Then it slowly flows through the feeding tube into the stomach.
The nurse removes the syringe or connecting tubing after the feeding. Then the nurse clamps and covers the end of the feeding tube with a cap or gauze. Gauze is secured in place with a rubber band. Clamping prevents air from entering the tube. It also prevents fluid from leaking out of the tube. Covering the end of the tube also prevents leaking.
Continuous feedings
These feedings are usually given over 24 hours. A feeding pump is used (Fig. 25-7). Formula drips into the feeding tube at a certain rate per minute. The person receives a certain amount every hour.
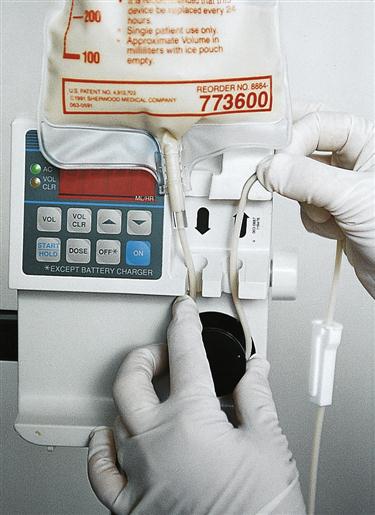
A pump alarm sounds if something is wrong. When you hear an alarm, tell the nurse.
Observations
Diarrhea, constipation, delayed stomach emptying, and aspiration are risks. Report the following at once:
• Nausea
• Discomfort during the feeding
• Vomiting
• Distended (enlarged and swollen) abdomen
• Coughing
• Complaints of indigestion or heartburn
• Redness, swelling, drainage, odor, or pain at the ostomy site
• Fever
• Signs and symptoms of respiratory distress (Chapter 28)
• Increased pulse rate (Chapter 31)
• Complaints of flatulence (Chapter 23)
Preventing aspiration
Aspiration is a major risk from tube feedings. It can cause pneumonia and death. Aspiration can occur:
• From tube movement out of place. Coughing, sneezing, vomiting, suctioning, and poor positioning are common causes. A tube can move from the stomach or intestines into the esophagus and then into the airway. The RN checks tube placement before every scheduled tube feeding. With continuous feedings, the RN checks tube placement every 4 hours. To do so, the RN attaches a syringe to the tube. GI secretions are withdrawn through the syringe. Then the pH of the secretions is measured (Chapter 33). You never check feeding tube placement.
To help prevent regurgitation and aspiration:
Persons with NG or gastrostomy tubes are at great risk for regurgitation. The risk is less with intestinal tubes. Formula passes directly into the small intestine. Also, formula is given at a slow rate. During digestion, food slowly passes from the stomach into the small intestine. The stomach handles larger amounts of food at one time than does the small intestine.
Digestion slows with aging. Stomach emptying also slows. Older persons are at risk for regurgitation and aspiration. Less formula and longer feeding times prevent over-feeding.
Comfort measures
Persons with feeding tubes usually are not allowed to eat or drink. They are NPO—nothing by mouth (Chapter 24). Dry mouth, dry lips, and sore throat cause discomfort. Sometimes hard candy or gum is allowed. These measures are common:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree