Bowel elimination
Objectives
• Define the key terms and key abbreviations listed in this chapter.
• List the observations to make about defecation.
• Identify the factors that affect bowel elimination.
• Describe the common bowel elimination problems.
• Explain how to promote comfort and safety during defecation.
• Explain why enemas are given.
• Describe the common enema solutions.
• Describe the rules for giving enemas.
• Describe how to care for a person with an ostomy.
• Perform the procedures described in this chapter.
Key terms
colostomy A surgically created opening (stomy) between the colon (colo) and abdominal wall
constipation The passage of a hard, dry stool
defecation The process of excreting feces from the rectum through the anus; a bowel movement
dehydration The excessive loss of water from tissues
diarrhea The frequent passage of liquid stools
enema The introduction of fluid into the rectum and lower colon
fecal impaction The prolonged retention and buildup of feces in the rectum
fecal incontinence The inability to control the passage of feces and gas through the anus
feces The semi-solid mass of waste products in the colon that is expelled through the anus
flatulence The excessive formation of gas or air in the stomach and intestines
flatus Gas or air passed through the anus
ostomy A surgically created opening for the elimination of body wastes; see “colostomy” and “ileostomy”
peristalsis The alternating contraction and relaxation of intestinal muscles
stoma An opening that can be seen through the abdominal wall; see “colostomy” and “ileostomy”
stool Excreted feces
suppository A cone-shaped, solid drug that is inserted into a body opening; it melts at body temperature
KEY ABBREVIATIONS
| BM | Bowel movement |
| C | Centigrade |
| F | Fahrenheit |
| GI | Gastro-intestinal |
| ID | Identification |
| IV | Intravenous |
| mL | Milliliter |
| oz | Ounce |
| SSE | Soapsuds enema |
Bowel elimination is a basic physical need. It is the excretion of wastes from the gastro-intestinal system (GI) (Chapter 9). Many factors affect bowel elimination. They include privacy, habits, age, diet, exercise and activity, fluids, and drugs. Problems easily occur. Promoting normal bowel elimination is important. You assist residents in meeting elimination needs.
Normal bowel elimination
Foods and fluids are partially digested in the stomach. The partially digested food and fluids are called chyme. Chyme passes from the stomach into the small intestine. It enters the large intestine (large bowel or colon) where fluid is absorbed. Chyme becomes less fluid and more solid in consistency. Feces refers to the semi-solid mass of waste products in the colon that is expelled through the anus.
Feces move through the intestines by peristalsis. Peristalsis is the alternating contraction and relaxation of intestinal muscles. The feces move through the large intestine to the rectum. Feces are stored in the rectum until excreted from the body. Defecation (bowel movement [BM]) is the process of excreting feces from the rectum through the anus. Stool refers to excreted feces.
Some people have a BM every day. Others have one every 2 to 3 days. Some people have 2 or 3 BMs a day. Many people have a BM after breakfast. Others do so in the evening. Many older persons expect to have a BM every day. They are very concerned if they do not do so. The nurse teaches them about normal elimination.
Stools are normally brown. Bleeding in the stomach and small intestine causes black or tarry stools. Bleeding in the lower colon and rectum causes red-colored stools. So do beets, tomato juice or soup, red Jell-O, and foods with red food coloring. A diet high in green vegetables can cause green stools. Diseases and infection can cause clay-colored or white, pale, orange-colored, or green-colored stools.
Stools are normally soft, formed, moist, and shaped like the rectum. They have a normal odor caused by bacterial action in the intestines. Certain foods and drugs also cause odors.
Observations
Your observations are used for the nursing process. Carefully observe stools before disposing of them. Ask the nurse to observe abnormal stools. Observe and report the following to the nurse. If allowed to chart, also record the following:
See Focus on Communication: Observations.
Factors affecting bowel elimination
These factors affect stool frequency, consistency, color, and odor. The nurse considers them when using the nursing process to meet the person’s elimination needs. Normal, regular elimination is the goal.
• Disability. Some people cannot control bowel movements. They have a BM whenever feces enter the rectum. A bowel training program is needed (p. 359).
Safety and comfort
The care plan includes measures to meet the person’s elimination needs. It may involve diet, fluids, and exercise. Follow the measures in Box 23-1 to promote safety and comfort.
See Teamwork and Time Management: Safety and Comfort.
Common problems
Common problems include constipation, fecal impaction, diarrhea, fecal incontinence, and flatulence.
Constipation
Constipation is the passage of a hard, dry stool. The person usually strains to have a BM. Stools are large or marble-size. Large stools cause pain as they pass through the anus. Constipation occurs when feces move slowly through the bowel. This allows more time for water absorption. Common causes of constipation include:
Dietary changes, fluids, and activity prevent or relieve constipation. So do drugs and enemas.
Fecal impaction
A fecal impaction is the prolonged retention and build-up of feces in the rectum. Feces are hard or putty-like. Fecal impaction results if constipation is not relieved. The person cannot defecate. More water is absorbed from the already hard feces. Liquid feces pass around the hardened fecal mass in the rectum. The liquid feces seep from the anus.
The person tries many times to have a BM. Abdominal discomfort, abdominal distention (swelling), nausea, cramping, and rectal pain are common. Older persons may have poor appetite or confusion. Some persons may have a fever. Report these signs and symptoms to the nurse.
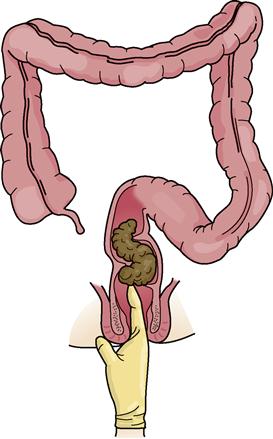
The nurse does a digital (finger) exam to check for an impaction. A lubricated, gloved finger is inserted into the rectum to feel for a hard mass (Fig. 23-1). The mass is felt in the lower rectum. Sometimes it is higher in the colon and out of reach. The digital exam often causes the urge to have a BM. The doctor may order drugs and enemas to remove the impaction.
Sometimes the nurse removes the fecal mass with a gloved finger. This is called digital removal of an impaction.
Diarrhea
Diarrhea is the frequent passage of liquid stools. Feces move through the intestines rapidly. This reduces the time for fluid absorption. The need for a BM is urgent. Some people cannot get to a bathroom in time. Abdominal cramping, nausea, and vomiting may occur.
Causes of diarrhea include infections, some drugs, irritating foods, and microbes in food and water. Diet and drugs are ordered to reduce peristalsis. You need to:
• Assist with elimination needs promptly.
• Dispose of stools promptly. This prevents odors and the spread of microbes.
Fluid lost through diarrhea is replaced. Otherwise dehydration occurs. Dehydration is the excessive loss of water from tissues. The person has pale or flushed skin, dry skin, and a coated tongue. The urine is dark and scant in amount (oliguria). Thirst, weakness, dizziness, and confusion also occur. Falling blood pressure and increased pulse and respirations are serious signs. Death can occur. The nursing process is used to meet the person’s fluid needs. The doctor may order IV (intravenous) fluids in severe cases (Chapter 25).
Microbes can cause diarrhea. Preventing the spread of infection is important. Always follow Standard Precautions and the Bloodborne Pathogen Standard when in contact with stools.
See Promoting Safety and Comfort: Diarrhea.
Fecal incontinence
Fecal incontinence is the inability to control the passage of feces and gas through the anus. Causes include:
• Nervous system diseases and injuries
• Diarrhea
• Aging
• Mental health problems or dementia (Chapters 43 and 44)—the person may not recognize the need for or act of having a BM
• Not answering signal lights when help is needed with elimination
• Not getting to the bathroom in time
• Not finding the bathroom when in a new setting
Fecal incontinence affects the person emotionally. Frustration, embarrassment, anger, and humiliation are common. The person may need:
• Help with elimination after meals and every 2 to 3 hours
• Incontinence products to keep garments and linens clean
See Residents With Dementia: Fecal Incontinence.
Flatulence
Gas and air are normally in the stomach and intestines. They are expelled through the mouth (burping, belching, eructating) and anus. Gas or air passed through the anus is called flatus. Flatulence is the excessive formation of gas or air in the stomach and intestines. Causes include:
• Bacterial action in the intestines.
• Gas-forming foods (onions, beans, cabbage, cauliflower, radishes, and cucumbers).
• Bowel and abdominal surgeries.
If flatus is not expelled, the intestines distend. That is, they swell or enlarge from the pressure of gases. Abdominal cramping or pain, shortness of breath, and a swollen abdomen occur. “Bloating” is a common complaint. Exercise, walking, moving in bed, and the left-side lying position often produce flatus. Doctors may order enemas and drugs to relieve flatulence.
Bowel training
Meals, especially breakfast, stimulate the urge for a BM. The person’s usual time of day for a BM is noted on the care plan. So is toilet, commode, or bedpan use. Offer help with elimination at the times noted. Factors that promote elimination are part of the care plan and bowel training program. These include a high-fiber diet, increased fluids, warm fluids, activity, and privacy. The nurse tells you about a person’s bowel training program.
The doctor may order a suppository to stimulate a BM. A suppository is a cone-shaped, solid drug that is inserted into a body opening. It melts at body temperature. A nurse inserts a rectal suppository into the rectum (Fig. 23-2, p. 360). A BM occurs about 30 minutes later.
Enemas
An enema is the introduction of fluid into the rectum and lower colon. Doctors order enemas:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree