Drugs Used to Treat Dyslipidemias
Objectives
1 Describe atherosclerosis and its effects on the cardiovascular system
2 Identify the four major types of lipoproteins.
3 Describe the primary treatment modalities for lipid disorders.
Key Terms
atherosclerosis ( ) (p. 344)
) (p. 344)
hyperlipidemia ( ) (p. 344)
) (p. 344)
dyslipidemias ( ) (p. 344)
) (p. 344)
triglycerides ( ) (p. 344)
) (p. 344)
lipoproteins ( ) (p. 344)
) (p. 344)
chylomicrons ( ) (p. 344)
) (p. 344)
metabolic syndrome ( ) (p. 345)
) (p. 345)
Atherosclerosis
![]() http://evolve.elsevier.com/Clayton
http://evolve.elsevier.com/Clayton
For an introduction to cardiovascular diseases, see Chapter 21. Coronary artery disease (CAD), (also called coronary heart disease) is a major cause of premature death in the United States and most other industrialized nations. Major treatable causes of CAD are a sedentary lifestyle, poor eating habits, hypertension, cigarette smoking, type 2 diabetes mellitus, and atherosclerosis. Atherosclerosis is characterized by the accumulation of fatty deposits on the inner walls of the arteries and arterioles throughout the body that reduces the blood supply to vital organs, resulting in strokes, angina pectoris, myocardial infarction, and peripheral vascular disease. A primary cause of atherosclerosis is the abnormal elevation of cholesterol and triglyceride levels in the blood as part of a disease known as hyperlipidemia. Dyslipidemias are defined as abnormalities that involve one or more of the blood fats (lipids). Dyslipidemias can be the result of genetic abnormalities, secondary causes (e.g., lifestyle, drugs, underlying diseases), or both. A diet that is high in saturated fats, cholesterol, carbohydrates, total calories, and alcohol as well as a sedentary lifestyle contribute significantly to dyslipidemias.
Types Of lipoproteins
Cholesterol is a naturally occurring substance that is essential for synthesizing the body steroids that are used by the endocrine system, for synthesizing the bile acids that are needed for food absorption, and for cell membrane synthesis. The body is able to manufacture enough cholesterol to meet its metabolic needs. However, the body also converts excess dietary carbohydrates into triglycerides (a precursor of cholesterol), and it converts dietary fat into cholesterol. After being absorbed from the gastrointestinal (GI) tract, fats (lipids), triglycerides, and cholesterol are bound to circulating proteins called lipoproteins for transport through the body.
Lipoproteins are subdivided into five categories on the basis of their composition: chylomicrons, very low-density lipoproteins (VLDLs), intermediate-density lipoproteins (IDLs), low-density lipoproteins (LDLs), and high-density lipoproteins (HDLs). The five types differ in relative concentrations of triglycerides, cholesterol, and proteins. Clinically, the IDL is included in the LDL measurement. Chylomicrons consist of about 90% triglycerides and 5% cholesterol; VLDLs represent about 15% to 20% of total serum cholesterol and most of the total blood triglyceride concentration, whereas HDLs contain about 20% to 30% cholesterol and 1% to 7% triglycerides.
The purpose of HDLs appears to be to transport cholesterol from peripheral cells to the liver for metabolism. HDLs are sometimes referred to as the “good” lipoproteins, because high levels indicate that cholesterol is being removed from vascular tissue, where it may participate in the development of CAD. Low HDL levels are considered a positive risk factor for the development of CAD; high HDL levels are a negative risk factor for CAD. LDLs account for 60% to 70% of total serum cholesterol, and they are the major contributor to atherosclerosis. The probability that atherosclerosis will develop is related directly to the concentration of LDL cholesterol (LDL-C) in the blood circulation.
LDL is the primary target of cholesterol-lowering therapy. High triglyceride levels are also associated with an increased risk of CAD. Consequently, patient assessment and cholesterol-lowering treatment goals are based on the total cholesterol, LDL-C, HDL cholesterol (HDL-C), and triglyceride levels (Table 22-1). Other markers being tested to see whether they are better predictors of the risk for impending heart disease are the concentration of apolipoprotein A-1 (the major protein component of HDL), apolipoprotein B (a measure of the total number of atherogenic particles); C-reactive protein (an indicator of inflammation); and non-HDL cholesterol, the sum of the cholesterol in both LDL-C and triglyceride-rich lipoproteins.
Table 22-1
| OPTIMAL | NEAR OPTIMAL | BORDERLINE HIGH RISK | HIGH RISK | VERY HIGH RISK | |
| Total cholesterol (mg/dL) | <200 | — | 200 to 239 | ≥240 | — |
| Low-density lipoprotein (LDL) cholesterol (mg/dL) | <100 | 100 to 129 | 130 to 159 | 160 to 189 | ≥190 |
| High-density lipoprotein (HDL)cholesterol* (mg/dL) | ≥60† | — | — | — | — |
| Triglycerides (mg/dL) | <150 | — | 150 to 199 | 200 to 499 | ≥500 |
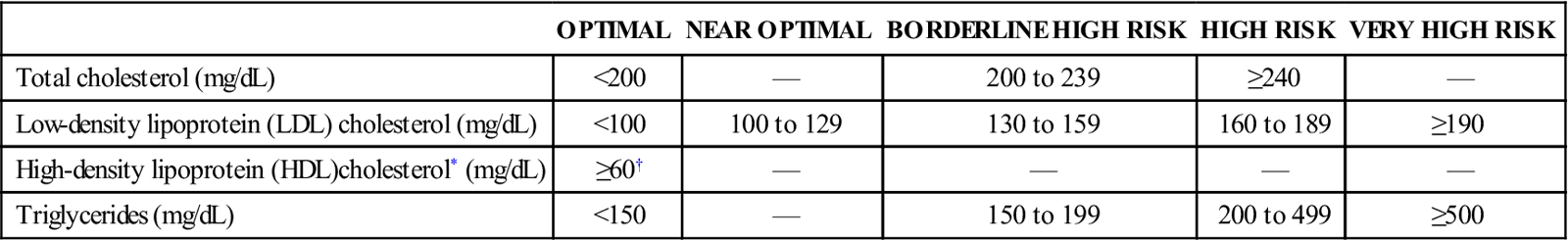
*Low high-density lipoprotein cholesterol ≤40 mg/dL.
†>70 mg/dL for people at very high risk for cardiovascular disease.
From the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults: Third Report of the National Cholesterol Education Program, Bethesda, Md., National Institutes of Health Publication No. 02-5215, September 2002. National Heart, Lung, and Blood Institute; National Institutes of Health.
Treatment of Hyperlipidemias
An estimated 105 million American adults have total blood cholesterol levels of 200 mg/dL or more. Of these, about 37 million American adults have levels of 240 mg/dL or more. Some of the most common hyperlipidemias of genetic origin are treatable with medicines (Table 22-2). However, it is becoming recognized that lifestyle may be the greatest contributor to the development of hyperlipidemia. A cluster of risk factors that relate directly to excesses in lifestyle is now recognized as metabolic syndrome (see Chapter 21).
Table 22-2
Lipoprotein Disorders Treatable With Diet and Drug Therapy*
| DYSLIPIDEMIA | ABNORMAL LIPIDS | SINGLE DRUG TREATMENT | COMBINATION DRUG TREATMENT |
| Familial hypercholesterolemia | ↑ Low-density lipoprotein cholesterol | Statin Bile-acid–binding resin, niacin | Bile-acid–binding resin + niacin; bile-acid–binding resin + statin; niacin + statin |
| Polygenic hypercholesterolemia | ↑ Low-density lipoprotein cholesterol | Bile-acid–binding resin, niacin, statin | Bile-acid–binding resin + niacin; bile-acid–binding resin + statin; niacin + statin |
| Familial hypertriglyceridemia | ↑ Triglycerides | Fibrate, niacin | Fibrate + niacin |
| Mixed hyperlipidemia | ↑ Low-density lipoprotein cholesterol, ↑ triglycerides | Niacin, statin, fibrate† | Niacin + statin; niacin + bile-acid–binding resin; niacin + fibrate |
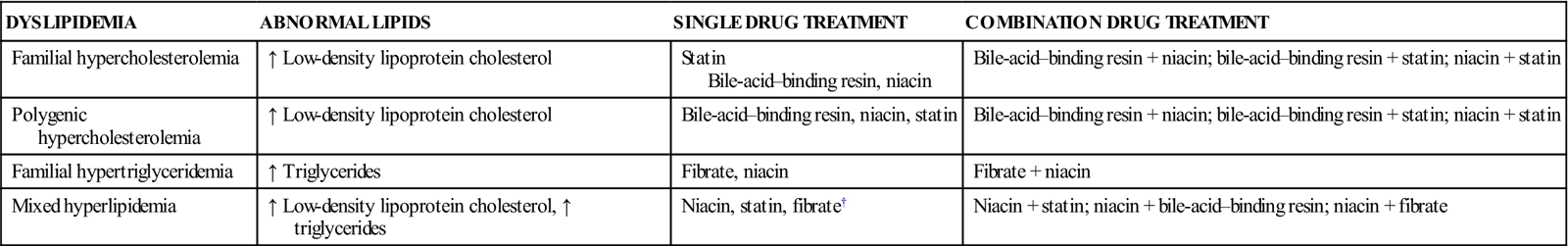
*Diet, exercise, and weight loss are the primary treatments. The primary drug treatment is listed first, followed by other treatments in decreasing order.
†Combined fibrate and statin therapy is not recommended as a result of the increased risk for myopathy.
The National Cholesterol Education Program (NCEP) recommends that treatment regimens be based on the presence of CAD, the level of total cholesterol, the level of HDL-C, and the success of appropriate diet interventions. The primary treatment of hyperlipidemia is with what are called therapeutic lifestyle changes (TLCs), which include weight reduction, exercise, and a diet that is low in cholesterol and fat. Studies show that, with a reduction in elevated LDL-C and triglyceride levels and an increase in the HDL-C level, the frequency of heart attacks and strokes is substantially reduced.
The NCEP Guidelines recommend reduced intake of saturated fatty acids (<7% of total calories), with the remainder of total fats from polyunsaturated and monounsaturated fatty acids (25% to 35% of total calories), and intake of less than 200 mg of cholesterol per day. The addition of plant stanols and sterols (2 g/day) and soluble fiber (10 to 15 g/day) can further reduce LDL-C level by approximately 10%. Carbohydrates should be limited to 60% of the total daily caloric intake. Weight reduction can substantially reduce the LDL-C level while raising HDL levels. Regular exercise can also raise HDL levels, promote weight loss, lower blood pressure, reduce the risk of diabetes mellitus, and improve coronary blood flow. If a good trial of changes in diet and exercise habits does not produce an acceptable decrease in blood lipid levels, antilipemic agents may be added to the patient’s regimen. In general, for every 1% reduction in the LDL level, there is a 1% reduction in the rate of coronary artery disease events.
Drug Therapy for Hyperlipidemias
Actions
Antilipemic agents may be used to treat hyperlipidemias only if diet, exercise, and weight reduction are not successful for adequately lowering LDL-C levels. (See the individual drug monographs for information about the mechanisms of action of different antilipemic agents.)
Uses
The NCEP Guidelines recognize bile-acid–binding resins (e.g., cholestyramine, colestipol, colesevelam), niacin, and the 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors (i.e., statins, including atorvastatin, fluvastatin, lovastatin, pitavastatin, pravastatin, rosuvastatin, simvastatin) as the primary drugs for lowering serum cholesterol levels. The fibric acids (e.g., gemfibrozil, fenofibrate) are effective triglyceride-lowering agents, but they are not the first-line drugs for the treatment of hyperlipidemias because they do not usually produce substantial reductions in LDL-C. Omega-3 fatty acids have been approved by the U.S. Food and Drug Administration for treatment of very high triglyceride levels (>500 mg/dL) in adults. Niacin is the most effective therapy for raising HDL-C levels (20% to 35% increase); followed by fibrate therapy (10% to 25% increase), and statin therapy (2% to 15% increase).
Selection of initial antilipemic therapy depends on the type of dyslipidemia present. Pharmacologic antilipemic therapy is often started with a statin because of their safety record and success in lowering cholesterol levels. The statins are the most potent and highly effective drugs for lowering LDL-C levels, and they appear to be relatively safe. However, they are substantially more expensive than other treatments. Prescription-strength niacin is effective for lowering total cholesterol and triglyceride levels and for raising HDL-C levels.
After starting drug therapy, the LDL-C level should be measured at 4 to 6 weeks and again at 3 months. If the response to initial drug therapy is inadequate, the dosage of the statin should be increased or another drug should be added to the treatment regimen. The combination of a bile-acid–binding resin with either niacin or a statin can potentially lower LDL-C levels by 40% to 50%. In rare cases of particularly high cholesterol levels, triple therapy with a bile-acid–binding resin, niacin, and a statin may be required. Drug therapy is likely to continue for many years or the patient’s lifetime; plasma lipid levels return to pretreatment levels after 2 to 3 weeks if therapy is discontinued.
 Nursing Implications for Hyperlipidemia Therapy
Nursing Implications for Hyperlipidemia Therapy
Assessment
History of Risk Factors.
Obtain the patient’s age, note gender and race, and take a family history of the incidence of elevated cholesterol and lipid levels. Ask whether any first-generation family members have a history of or have died from CAD. Obtain the ages and details of individuals with a history of CAD. Are there any living relatives with elevated cholesterol or elevated triglyceride levels?
Hypertension.
Ask whether the patient has ever been told that he or she has elevated blood pressure. If yes, obtain details. Ask about medications that have been prescribed. Are the medications being taken regularly? If not, why not? Take the patient’s blood pressure in lying, sitting, and standing positions daily.
Smoking.
Obtain a history of the number of cigarettes or cigars smoked daily. How long has the patient smoked? Has the patient ever tried to stop smoking? Determine the patient’s knowledge of the effects of smoking on the vascular system. How does the individual feel about modifying his or her smoking habit?
Dietary Habits
Glucose Intolerance.
Ask specific questions regarding whether the individual has now or has ever had an elevated serum glucose (blood sugar) level. If yes, what dietary modifications have been made? How successful are they? What medications are being taken for the elevated serum glucose level (e.g., oral hypoglycemic agents, insulin)?
Elevated Serum Lipid Levels.
Find out whether the patient is aware of having elevated lipid, triglyceride, or cholesterol levels. If so, what measures has the patient tried for reduction, and what effect have the interventions had on the blood levels at subsequent examinations? Review available laboratory data (e.g., LDL, VLDL). A fasting lipoprotein profile that includes total cholesterol, LDL-C, HDL-C, and triglyceride levels is recommended for all adults 20 years old or older at least once every 5 years.
Obesity.
Weigh the patient. Ask about any recent weight gain or loss and whether it was intentional or unintentional. Using the person’s height and weight, determine the person’s body mass index (see Chapter 21). If obesity is present, what strategies for weight reduction have been tried?
Psychomotor Functions
 Patient Education
Patient Education
Nutrition.
Patients who take bile-acid–sequestering resins may require supplemental vitamins. (The fat-soluble vitamins—D, E, A, and K—may become deficient with long-term resin therapy.)
Vitamin K Deficiency.
If the patient is receiving a prescription for a bile-acid–sequestering resin, teach the patient about the signs and symptoms of vitamin K deficiency, including bleeding gums, bruising, dark tarry stools, and coffee-ground emesis. This interaction is rare but, if symptoms occur, they should be reported immediately to the health care provider.
Follow-Up Care.
Stress the need for long-term regular assessment of the required serum levels (e.g., lipid profile values, liver studies, bleeding times) to track progress, identify the need for modifications in therapeutic interventions, and detect possible adverse effects of the medications. To obtain this information, blood studies and regular visits to the health care provider are necessary.
Relating to Medication Regimen.
Examine the individual drug monographs for details about mixing drugs, scheduling medication administration, and techniques for improving compliance of patients taking these medications.
Fostering Health Maintenance
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


