Part 2 Pain Assessment and Management
Children’s ability to describe pain changes as they grow older and as they cognitively and linguistically mature. Three types of measures—behavioral, physiologic, and self-report—have been developed to measure children’s pain, and their applicability depends on the child’s cognitive and linguistic ability.
DEVELOPMENTAL CHARACTERISTICS OF CHILDREN’S RESPONSES TO PAIN
Preterm Infant
1. The preterm infant’s response may be behaviorally blunted or absent; however, there is sufficient evidence that preterm infants are neurologically capable of experiencing pain.
2. Use a preterm infant pain scale.
3. Assume that painful procedures in older child and adult are also painful in preterm infant (e.g., venipuncture, lumbar puncture, endotracheal intubation, circumcision, chest tube insertion, heel puncture).
Young Infant
1. Generalized body response of rigidity or thrashing, possibly with local reflex withdrawal of stimulated area
3. Facial expression of pain (brows lowered and drawn together, eyes tightly closed, and mouth open and squarish)
4. No association demonstrated between approaching stimulus and subsequent pain
Young Child
2. Verbal expressions such as “Ow,” “Ouch,” “It hurts”
4. Attempts to push stimulus away before it is applied
5. Lack of cooperation; need for physical restraint
6. Requests termination of procedure
7. Clings to parent, nurse, or other significant person
8. Requests emotional support, such as hugs or other forms of physical comfort
9. May become restless and irritable with continuing pain
10. Behaviors occurring in anticipation of actual painful procedure
School-Age Child
1. May see all behaviors of young child, especially during actual painful procedure, but less in anticipatory period
2. Stalling behavior, such as “Wait a minute” or “I’m not ready”
3. Muscular rigidity, such as clenched fists, white knuckles, gritted teeth, contracted limbs, body stiffness, closed eyes, wrinkled forehead
NONPHARMACOLOGIC STRATEGIES FOR PAIN MANAGEMENT
General Strategies
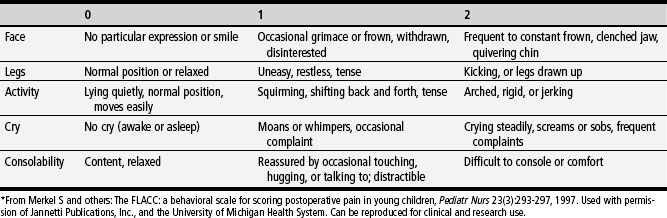
TABLE 2-1 Behavioral Pain Assessment Scales for Infants and Young Children
| AGES OF USE | INSTRUMENT |
|---|---|
| 4 months to 18 years | Objective Pain Score (OPS) (Hannallah and others, 1987) |
| 1 to 5 years | Children’s Hospital of Eastern Ontario Pain Scale (CHEOPS) (McGrath and others, 1985) |
| Newborn to 16 years | Nurses Assessment of Pain Inventory (NAPI) (Stevens, 1990) |
| 3 to 36 months | Behavioral Pain Score (BPS) (Robieux and others, 1991) |
| 4 to 6 months | Modified Behavioral Pain Scale (MBPS) (Taddio and others, 1995) |
| <36 months and children with cerebral palsy | Riley Infant Pain Scale (RIPS) (Schade and others, 1996) |
| 2 months to 7 years | FLACC Postoperative Pain Tool (Merkel and others, 1997) |
| 1 to 7 months | Postoperative Pain Score (POPS) (Attia and others, 1987) |
| Average gestational age 33.5 weeks | Neonatal Infant Pain Scale (NIPS) (Lawrence and others, 1993) |
| 27 weeks gestational age to full term | Pain Assessment Tool (PAT) (Hodgkinson and others, 1994) |
| 1 to 36 months | Pain Rating Scale (PRS) (Joyce and others, 1994) |
| 32 to 60 weeks gestational age | CRIES (Krechel, Bildner, 1995) |
| 28 to 40 weeks gestational age | Premature Infant Pain Profile (PIPP) (Stevens and others, 1996) |
| 0 to 28 days | Scale for Use in Newborns (SUN) (Blauer, Gerstmann, 1998) |
| Birth (23 weeks gestational age) and full-term newborns up to 100 days | Neonatal Pain, Agitation, and Sedation Scale (NPASS) (Puchalski, Hummel, 2002) |
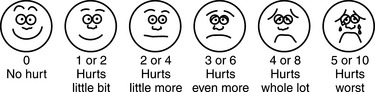
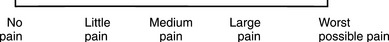
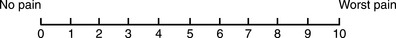
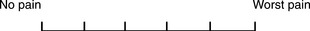
TABLE 2-3 Pain Rating Scales for Children
1. Use nonpharmacologic interventions to supplement, not replace, pharmacologic interventions, and use for mild pain and pain that is reasonably well controlled with analgesics.
2. Form a trusting relationship with child and family. Express concern regarding their reports of pain, and intervene appropriately.
3. Use general guidelines to prepare child for procedure.
4. Prepare child before potentially painful procedures, but avoid “planting” the idea of pain. For example, instead of saying, “This is going to (or may) hurt,” say, “Sometimes this feels like pushing, sticking, or pinching, and sometimes it doesn’t bother people. Tell me what it feels like to you.”
5. Use “nonpain” descriptors when possible (e.g., “It feels like heat” rather than “It’s a burning pain”). This allows for variation in sensory perception, avoids suggesting pain, and gives the child control in describing reactions.
6. Avoid evaluative statements or descriptions (e.g., “This is a terrible procedure” or “It really will hurt a lot”).
7. Stay with child during a painful procedure.
8. Allow parents to stay with child if child and parent desire; encourage parent to talk softly to child and to remain near child’s head.
9. Involve parents in learning specific nonpharmacologic strategies and in assisting child with their use.
10. Educate child about the pain, especially when explanation may lessen anxiety (e.g., that pain may occur after surgery and does not indicate something is wrong); reassure the child that he or she is not responsible for the pain.
11. For long-term pain control, give child a doll, which represents “the patient,” and allow child to do everything to the doll that is done to the child; pain control can be emphasized through the doll by stating, “Dolly feels better after the medicine.”
Specific Strategies
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree