Human Reproductive Anatomy and Physiology
Objectives
1. Define each key term listed.
2. Describe changes of puberty in males and females.
3. Identify the anatomy of the male reproductive system.
4. Explain the functions of the external and internal male organs in human reproduction.
5. Describe the influence of hormones in male reproductive processes.
6. Identify the anatomy of the female reproductive system.
7. Explain the functions of the external, internal, and accessory female organs in human reproduction.
8. Discuss the importance of the pelvic bones to the birth process.
9. Explain the menstrual cycle and the female hormones involved in the cycle.
Key Terms
biischial diameter (p. 26)
climacteric (klī-MĂK-tĕr-ĭk, p. 29)
diagonal conjugate (p. 26)
dyspareunia (dĭs-păh-RŪ-nē-ă, p. 23)
embryo (p. 24)
external os (p. 24)
follicle-stimulating hormone (FSH) (p. 27)
internal os (p. 24)
luteinizing hormone (LH) (p. 22)
menarche (mĕ-NĂR-kē, p. 27)
menopause (MĔN-ō-păwz, p. 29)
obstetric conjugate (p. 26)
obstetrical perineum (p. 22)
oxytocin (p. 29)
ovulation (p. 27)
ovum (p. 25)
prostate gland (p. 22)
puberty (p. 20)
rugae (RŪ-jē, p. 23)
semen (p. 22)
smegma (SMĔG-mă, p. 21)
spermatogenesis (spuĭr-maĭ-tō-JĔN-ĕ-sĭs, p. 21)
transverse diameter (p. 26)
zygote (ZĪ-gōt, p. 25)
![]() http://evolve.elsevier.com/Leifer
http://evolve.elsevier.com/Leifer
Understanding childbirth requires an understanding of the structures and functions of the body that make childbearing possible. This knowledge includes anatomy, physiology, sexuality, embryology of the growing fetus, and the psychosocial changes that occur in both the male and the female. This chapter addresses the anatomy and physiology of the male and female reproductive systems.
Puberty
Before puberty, male and female children appear very much alike except for their genitalia. Puberty involves changes in the whole body and the psyche as well as in the expectations of society toward the individual.
Puberty is a period of rapid change in the lives of boys and girls during which the reproductive systems mature and become capable of reproduction. Puberty begins when the secondary sex characteristics (e.g., pubic hair) appear. Puberty ends when mature sperm are formed or when regular menstrual cycles occur. This transition from childhood to adulthood has been identified and often celebrated by various rites of passage. Some cultures have required demonstrations of bravery, such as hunting wild animals or displays of self-defense. Ritual circumcision is another rite of passage in some cultures and religions. In the United States today, some adolescents participate in religious ceremonies such as bar or bat mitzvah or confirmation, but for others, these ceremonies are unfamiliar. The lack of a universal “rite of passage” to identify adulthood has led to confusion for some contemporary adolescents in many industrialized nations.
Male
Male hormonal changes normally begin between 10 and 16 years of age. Outward changes become apparent when the size of the penis and testes increases and there is a general growth spurt. Testosterone, the primary male sex hormone, causes the boy to grow taller, become more muscular, and develop secondary sex characteristics such as pubic hair, facial hair, and a deeper voice. The voice deepens but is often characterized by squeaks or cracks before reaching its final pitch. Testosterone levels are constant, not cyclical like female hormones, although levels may decrease with age to 50% of peak levels by age 80 years. Nocturnal emissions (“wet dreams”) may occur without sexual stimulation. These emissions usually do not contain sperm.
Female
The first outward change of puberty in females is development of the breasts (see Figure 2-7). The first menstrual period (menarche) occurs 2 to  years later (age 11 to 15 years). Female reproductive organs mature to prepare for sexual activity and childbearing. The female experiences a growth spurt, but her growth spurt ends earlier than the male’s. Her hips broaden as her pelvis assumes the wide basin shape needed for birth. Pubic hair and axillary hair appear. The quantity varies, as it does in males.
years later (age 11 to 15 years). Female reproductive organs mature to prepare for sexual activity and childbearing. The female experiences a growth spurt, but her growth spurt ends earlier than the male’s. Her hips broaden as her pelvis assumes the wide basin shape needed for birth. Pubic hair and axillary hair appear. The quantity varies, as it does in males.
Reproductive Systems
Male
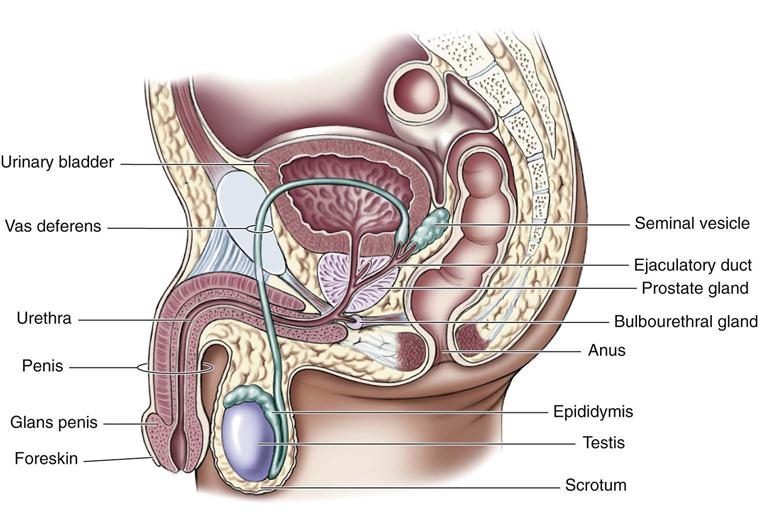
The male reproductive system consists of external and internal organs (Figure 2-1).
External Genitalia
The penis and the scrotum, which contains the testes, are the male external genitalia.
Penis.
The penis consists of the glans and the body. The glans is the rounded, distal end of the penis. It is visible on a circumcised penis but is hidden by the foreskin on an uncircumcised one. Smegma is a cheeselike sebaceous substance that collects under the foreskin and is easily removed with basic hygiene. At the tip of the glans is an opening called the urethral meatus. The body of the penis contains the urethra (the passageway for sperm and urine) and erectile tissue (the corpus spongiosum and two corpora cavernosa). The usually flaccid penis becomes erect during sexual stimulation when blood is trapped within the spongy erectile tissues. The erection allows the male to penetrate the female’s vagina during sexual intercourse. The penis has two functions:
Scrotum.
The scrotum is a sac that contains the testes. The scrotum is suspended from the perineum, keeping the testes away from the body and thereby lowering their temperature, which is necessary for normal sperm production (spermatogenesis).
Internal Genitalia
The internal genitalia include the testes, vas deferens, prostate, seminal vesicles, ejaculatory ducts, urethra, and accessory glands.
Testes.
The testes (testicles) are a pair of oval glands housed in the scrotum. They have two functions:
Sperm are made in the convoluted seminiferous tubules that are contained within the testes. Sperm production begins at puberty and continues throughout the life span of the male.
The production of testosterone, the most abundant male sex hormone, begins with the anterior pituitary gland. Under the direction of the hypothalamus, the anterior pituitary gland secretes follicle-stimulating hormone (FSH) and luteinizing hormone (LH). FSH and LH initiate the production of testosterone in the Leydig cells of the testes.
Testosterone has the following effects not directly related to sexual reproduction:
• Increases muscle mass and strength
• Promotes growth of long bones
• Increases basal metabolic rate (BMR)
• Enhances production of red blood cells
• Produces enlargement of vocal cords
These effects result in the greater strength and stature and a higher hematocrit level in males than in females. Testosterone also increases the production of sebum, a fatty secretion of the sebaceous glands of the skin, and may contribute to the development of acne during early adolescence. However, as the skin adapts to the higher levels of testosterone, acne generally recedes.
Ducts.
Each epididymis, one from each testicle, stores and carries the sperm to the penis. The sperm may remain in the epididymis for 2 to 10 days, during which time they mature and then move on to the vas deferens. Each vas deferens passes upward into the body, goes around the symphysis pubis, circles the bladder, and passes downward to form (with the ducts from the seminal vesicles) the ejaculatory ducts. The ejaculatory ducts then enter the back of the prostate gland and connect to the upper part of the urethra, which is in the penis. The urethra transports both urine from the bladder and semen from the prostate gland to the outside of the body, although not at the same time.
Accessory Glands.
The accessory glands are the seminal vesicles, the prostate gland, and the bulbourethral glands, also called Cowper’s glands. The accessory glands produce secretions (seminal plasma). The secretions of these glands have three functions:
The combined seminal plasma and sperm are called semen. Semen may be secreted during sexual intercourse before ejaculation. Therefore pregnancy may occur even if ejaculation occurs outside the vagina. Increased heat in the environment around the sperm (testes) increases the motility but shortens the life span of the sperm. A constant increase in temperature around the testes can prevent spermatogenesis and lead to permanent sterility. (Refer to a medical-surgical nursing textbook for the testicular self-examination procedure.)
Female
The female reproductive system consists of external genitalia, internal genitalia, and accessory structures such as the mammary glands (breasts). The bony pelvis is also discussed in this chapter because of its importance in the childbearing process.
External Genitalia
The female external genitalia are collectively called the vulva. They include the mons pubis, labia majora, labia minora, fourchette, clitoris, vaginal vestibule, and perineum (Figure 2-2).
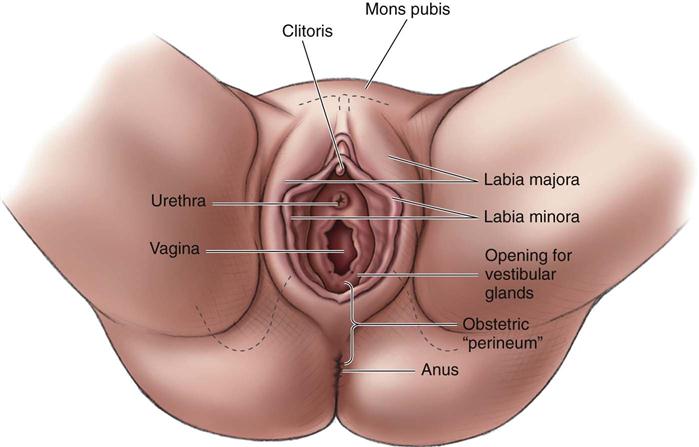
Mons Pubis.
The mons pubis (mons veneris) is a pad of fatty tissue covered by coarse skin and hair. It protects the symphysis pubis and contributes to the rounded contour of the female body.
Labia Majora.
The labia majora are two folds of fatty tissue on each side of the vaginal vestibule. Many small glands are located on the moist interior surface.
Labia Minora.
The labia minora are two thin, soft folds of tissue that are seen when the labia majora are separated. Secretions from sebaceous glands in the labia are bactericidal to reduce infection and also lubricate and protect the skin of the vulva.
Fourchette.
The fourchette is a fold of tissue just below the vagina, where the labia majora and the labia minora meet. It is also known as the obstetrical perineum. Lacerations in this area often occur during childbirth.
Clitoris.
The clitoris is a small, erectile body in the most anterior portion of the labia minora. It is similar in structure to the penis. Functionally, it is the most erotic, sensitive part of the female genitalia, and it produces smegma. Smegma is a cheeselike secretion of the sebaceous glands.
Vaginal Vestibule.
The vaginal vestibule is the area seen when the labia minora are separated and includes five structures:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


