Basic Principles of Drug Action and Drug Interactions
Objectives
1 Identify common drug administration routes.
2 Explain the potential problems associated with drug absorption.
3 Describe nursing interventions that can enhance drug absorption.
4 Describe the mechanisms of drug distribution.
5 Describe how the body inactivates drugs.
Key Terms
receptors ( ) (p. 12)
) (p. 12)
pharmacodynamics ( ) (p. 12)
) (p. 12)
agonists ( ) (p. 12)
) (p. 12)
antagonists ( ) (p. 12)
) (p. 12)
partial agonists ( ) (p. 12)
) (p. 12)
enteral ( ) (p. 12)
) (p. 12)
parenteral ( ) (p. 12)
) (p. 12)
percutaneous ( ) (p. 12)
) (p. 12)
pharmacokinetics ( ) (p. 13)
) (p. 13)
absorption ( ) (p. 13)
) (p. 13)
distribution ( ) (p. 13)
) (p. 13)
drug blood level (p. 14)
metabolism ( ) (p. 14)
) (p. 14)
excretion ( ) (p. 14)
) (p. 14)
half-life (p. 14)
Basic Principles Related to Drug Therapy
Drug Responses in the Body
![]() http://evolve.elsevier.com/Clayton
http://evolve.elsevier.com/Clayton
Drugs do not create new responses but rather alter existing physiologic activity. Drug response must be stated in relation to the physiologic activity expected in response to the drug therapy (e.g., an antihypertensive agent is successful if the patient’s blood pressure is lower after receiving the drug than it was before the drug was started). Therefore, it is important to perform a thorough nursing assessment to identify the baseline data. After that is done, results from regular assessments can be compared with the baseline data by the physician, the nurse, and the pharmacist to evaluate the effectiveness of the drug therapy.
Drug Interactions in the Body
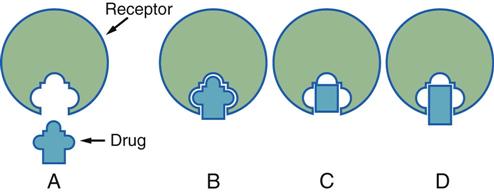
Drugs interact with the body in several different ways. Usually the drug forms chemical bonds with specific sites, called receptors, within the body. This bond forms only if the drug and its receptor have similar shapes and if the drug has a chemical affinity for the receptor. The relationship between a drug and a receptor is similar to that seen between a key and lock (Figure 2-1, A). The study of the interactions between drugs and their receptors and the series of events that result in a pharmacologic response is called pharmacodynamics. Most drugs have several different atoms within each molecule that interlock into various locations on a receptor. The better the fit between the receptor and the drug molecule, the better the response from the drug. The intensity of a drug response is related to how well the drug molecule fits into the receptor and to the number of receptor sites that are occupied. Drugs that interact with a receptor to stimulate a response are known as agonists (Figure 2-1, B). Drugs that attach to a receptor but do not stimulate a response are called antagonists (Figure 2-1, C). Drugs that interact with a receptor to stimulate a response but inhibit other responses are called partial agonists (Figure 2-1, D).
Routes of Drug Administration
The most common routes of drug administration are the enteral, parenteral, and percutaneous routes. When using the enteral route, the drug is administered directly into the gastrointestinal (GI) tract by the oral, rectal, or nasogastric route. The parenteral route bypasses the GI tract with the use of subcutaneous, intramuscular, or intravenous injection. The percutaneous route involves drugs being absorbed through the skin and mucus membranes. Methods of the percutaneous route include inhalation, sublingual (under the tongue), and topical (on the skin) administration.
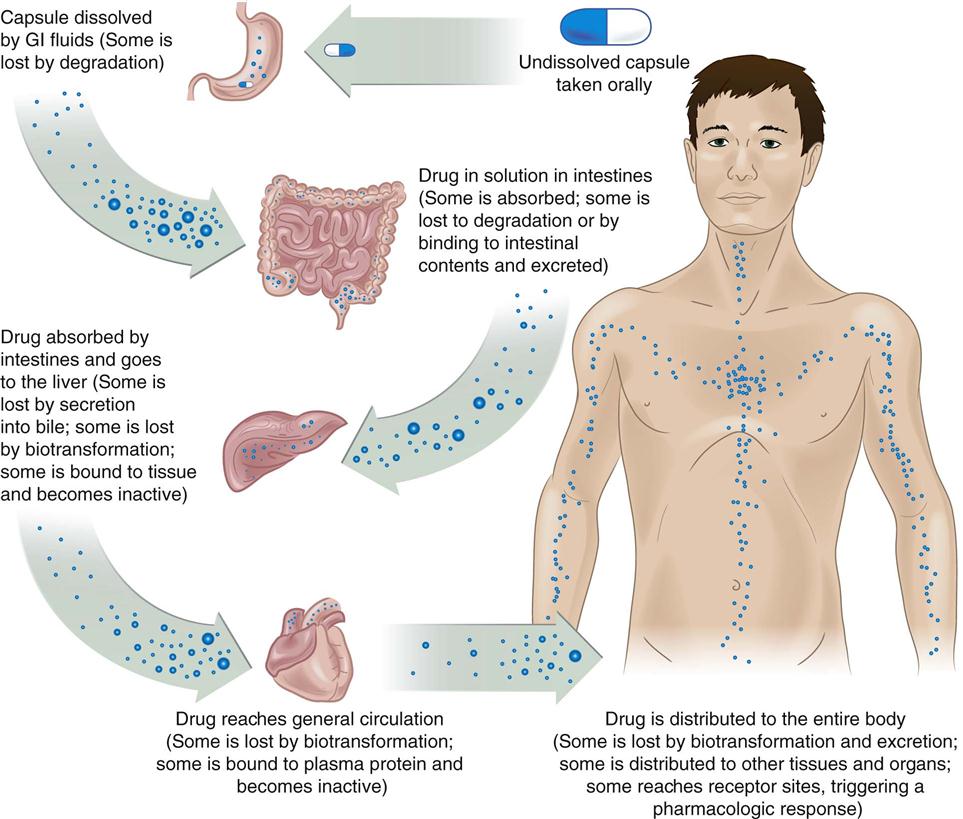
Liberation, Absorption, Distribution, Metabolism, and Excretion
After they have been administered, all drugs go through five stages: liberation, absorption, distribution, metabolism, and excretion (ADME). After liberation from the dosage form, each drug has its own unique ADME characteristics. The study of the mathematic relationships among the ADME features of individual medicines over time is called pharmacokinetics.
Liberation
Regardless of the route of administration, a drug must be released from the dosage form (i.e., liberated) and dissolved in body fluids before it can be absorbed into body tissues. For example, before a solid drug that is taken orally can be absorbed into the bloodstream for transport to the site of action, the dosage form (usually a capsule or tablet) must disintegrate, and the active drug must dissolve in the GI fluids so that it can be transported across the stomach or intestinal lining into the blood. The process of converting the drug into a form that will activate a response can be partially controlled by the pharmaceutical dosage form used (e.g., solution, suspension, capsule, tablet [with various coatings]). This conversion process can also be influenced by administering the drug with or without water or food in the patient’s stomach.
Absorption
Absorption is the process whereby a drug is transferred from its site of entry into the body to the circulating fluids of the body (i.e., blood and lymph) for distribution around the body. The rate at which this occurs depends on the route of administration, the blood flow through the tissue where the drug is administered, and the solubility of the drug. It is therefore important to do the following: (1) administer oral drugs with an adequate amount of fluid (usually a large [8-oz] glass of water); (2) give parenteral forms properly so that they are deposited in the correct tissue for enhanced absorption; and (3) reconstitute and dilute drugs only with the diluent recommended by the manufacturer in the package literature so that drug solubility is not impaired. Equally important are nursing assessments that reveal poor absorption (e.g., if insulin is administered subcutaneously and a lump remains at the site of injection 2 to 3 hours later, absorption from that site may be impaired).
The rate of absorption when a drug is administered by a parenteral route depends on the rate of blood flow through the tissues. Circulation or blood flow must be determined before the administration of drugs by the parenteral route to identify any circulatory insufficiency. If any such insufficiency is noted, injections will not be absorbed properly, and the drug will not be effective. Subcutaneous (subcut) injections have the slowest absorption rate, especially if peripheral circulation is impaired. Intramuscular (IM) injections are more rapidly absorbed because of greater blood flow per unit weight of muscle as compared with subcutaneous tissue. Cooling the area of injection slows the rate of absorption, whereas heat or massage hastens the rate of absorption. Drugs are dispersed throughout the body most rapidly when they are administered by intravenous (IV) injection. The nurse must be thoroughly educated regarding the responsibilities and techniques associated with administering IV medications. It is important to remember that, after a drug enters the patient’s bloodstream, it cannot be retrieved.
The absorption of topical drugs that have been applied to the skin can be influenced by the drug concentration, the length of contact time, the size of the affected area, the thickness of the skin surface, the hydration of the tissue, and the degree of skin disruption. Percutaneous (i.e., across-the-skin) absorption is greatly increased in newborns and young infants, who have thin, well-hydrated skin. When drugs are inhaled, their absorption can be influenced by the depth of the patient’s respirations, the fineness of the droplet particles, the available surface area of the patient’s mucous membranes, the contact time, the hydration state, the blood supply to the area, and the concentration of the drug itself.
Distribution
The term distribution refers to the ways in which drugs are transported throughout the body by the circulating body fluids to the sites of action or to the receptors that the drug affects. Drug distribution refers to the transport of the drug throughout the entire body by the blood and lymphatic systems and the transport from the circulating fluids into and out of the fluids that bathe the receptor sites. Organs with the most extensive blood supplies (e.g., heart, liver, kidneys, brain) receive the distributed drug most rapidly. Areas with less extensive blood supplies (e.g., muscle, skin, fat) receive the drug more slowly.
After a drug has been dissolved and absorbed into the circulating blood, its distribution is determined by the chemical properties of the drug and how it is affected by the blood and tissues that it contacts. Two factors that influence drug distribution are protein binding and lipid (fat) solubility. Most drugs are transported in combination with plasma proteins (especially albumin), which act as carriers for relatively insoluble drugs. Drugs that are bound to plasma proteins are pharmacologically inactive because the large size of the complex keeps them in the bloodstream and prevents them from reaching the sites of action, metabolism, and excretion. Only the free or unbound portion of a drug is able to diffuse into tissues, interact with receptors, and produce physiologic effects; it is also only this portion that can be metabolized and excreted. The same proportions of bound and free drug are maintained in the blood at all times. Thus, as the free drug acts on receptor sites or is metabolized, the decrease in the serum drug level causes some of the bound drug to be released from protein to maintain the ratio between bound and free drug.
When a drug leaves the bloodstream, it may become bound to tissues other than those with active receptor sites. The more lipid-soluble drugs have a high affinity for adipose tissue, which serves as a repository site for these agents. Because there is a relatively low level of blood circulation to fat tissues, the more lipid-soluble drugs tend to stay in the body much longer. An equilibrium is established between the repository site (i.e., lipid tissue) and the circulation so that, as the drug blood level drops as a result of binding at the sites of physiologic activity, metabolism, or excretion, more drug is released from the lipid tissue. By contrast, if more drug is given, a new equilibrium is established among the blood, the receptor sites, the lipid tissue repository sites, and the metabolic and excretory sites.
Distribution may be general or selective. Some drugs cannot pass through certain types of cell membranes, such as the blood-brain barrier (i.e., the central nervous system) or the placental barrier (i.e., the placenta), whereas other types of drugs readily pass into these tissues. The distribution process is very important, because the amount of drug that actually gets to the receptor sites determines the extent of pharmacologic activity. If little of the drug actually reaches and binds to the receptor sites, the response will be minimal.
Metabolism
Metabolism is the process whereby the body inactivates drugs. The enzyme systems of the liver are the primary sites for the metabolism of drugs, but other tissues and organs (e.g., white blood cells, GI tract, lungs) metabolize certain drugs to a minor extent. Genetic, environmental, and physiologic factors are involved in the regulation of drug metabolism reactions. The most important factors for the conversion of drugs to their metabolites are genetic variations of enzyme systems, the concurrent use of other drugs, exposure to environmental pollutants, concurrent illnesses, and age. (For more information, see Chapter 3.)
Excretion
The elimination of drug metabolites and, in some cases, of the active drug itself from the body is called excretion. The two primary routes of excretion are through the GI tract into the feces and through the renal tubules into the urine. Other routes of excretion include evaporation through the skin, exhalation from the lungs, and secretion into saliva and breast milk.
Because the kidneys are major organs of drug excretion, the nurse should review the patient’s chart for the results of urinalysis and renal function tests. A patient with renal failure often has an increase in the action and duration of a drug if the dosage and frequency of administration are not adjusted to allow for the patient’s reduced renal function.
Figure 2-2 shows a schematic review of the ADME process of an oral medication. It is important to note how little of the active ingredient actually reaches the receptor sites for action.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree