CHAPTER 14 1. Define common radiologic terms used to describe an x-ray. 2. Differentiate various densities that are evident on an x-ray. 3. Describe radiologic findings that are commonly seen in neonatal disease states. 4. Differentiate normal from abnormal findings on a chest x-ray. 5. Recognize findings on an x-ray that are consistent with congenital heart disease. 6. Describe an x-ray consistent with necrotizing enterocolitis. 7. Review correct indwelling line and tube placement on an x-ray. Radiographic medical imaging of abnormalities in a sick newborn infant is an established part of diagnostic evaluation. This evaluation assists the clinician in determining a diagnosis or formulating a differential diagnosis for treatment of the patient. Rarely is a newborn infant admitted to the neonatal intensive care unit (NICU) without having at least one x-ray taken, and frequently several additional films are needed during the course of treatment. Nurses need to become familiar with common radiographic findings to add to the knowledge base on which patient care is founded. This chapter reviews essentials of radiologic interpretation, discusses pathologic findings, and presents x-rays with common findings. A. Radiographs are images produced on a radiosensitive surface, such as film, when x-ray beams are passed through an object to the surface below (Stedman’s Medical Dictionary, 2013). B. By comparing densities and shapes from the image produced on the film, information can be deduced or inferred regarding anatomy, pathology, and function. A. Air bronchogram: air in the bronchial tree visualized against a background of generalized alveolar atelectasis (Stedman’s Medical Dictionary, 2013). B. Artifact: an unnaturally occurring silhouette that is artificially reproduced on an x-ray and is not a part of the patient (e.g., electrocardiogram leads, temperature probes). C. Cardiothoracic ratio: computed by dividing the maximum cardiac width by the maximum thoracic width to determine the heart size. D. Carina: bifurcation of the trachea, usually about the level of the third and fourth thoracic vertebrae (Stedman’s Medical Dictionary, 2013). Used in determining location of endotracheal tube. E. Expiratory film: obtained when the infant is in expiration; appears to increase cardiac size, accentuate lung markings, and decrease normal lung expansion. F. Exposure: amount of radiation used, producing a film ranging from light to dark. An underpenetrated (underexposed) film causes images to appear light and hazy. Overpenetration (overexposure) causes the film to be dark and to lack contrast, in comparison with an appropriately penetrated and exposed film. G. Hyperexpanded lungs: lungs expanded to greater than the ninth rib. H. Hypoexpanded lungs: lungs expanded to less than the seventh rib. I. Inspiratory film: obtained when infant is in full inspiration and the lungs project to the eighth rib above the right diaphragmatic dome, with the trachea shown in a straight projection. This is the optimal for chest film interpretation. J. Interlobar fissure: accumulation of fluid in the pleural space between the lung lobes. The fissure may be fluid filled and may appear as a distinctive line. K. Perihilar: pertaining to radiographic area bordering mediastinal structures. L. Pleural effusion: abnormal collection of fluid in the pleural space (Stedman’s Medical Dictionary, 2013). M. Radiolucent: pertaining to substances with varying degrees of transparency (Stedman’s Medical Dictionary, 2013). N. Radiopaque: pertaining to substances that are dense and nonpenetrable to x-rays (Stedman’s Medical Dictionary, 2013). O. Rad: fundamental unit of radiation measurement (Stedman’s Medical Dictionary, 2013). P. Roentgen: unit of exposure (Stedman’s Medical Dictionary, 2013). Q. Rotation: turned from the midline. Chest structures closest to the beam are magnified, making their shadows appear enlarged and distorted. R. Skinfold: the most common artifact seen in the neonate. Manifests as a straight line of variable length that can travel across or outside the chest or across the diaphragm and into the abdomen. Results from folding of excessive skin; may mimic a pneumothorax. However, the obliquity of the line produced by a skinfold is opposite to that produced by the edge of the lung in pneumothorax. S. Proper technique: signifies correct exposure, positioning, and timing in relation to inspiration and proper labeling of a film. T. X-ray: a form of electromagnetic radiation with shorter wavelengths than normal light. X-rays can penetrate most structures (Stedman’s Medical Dictionary, 2013). B. Cross-table lateral view. X-ray beam passes horizontally through infant in the supine position. Used for general assessment, assessment of free air in the chest, and to verify line placement. C. Lateral decubitus view. X-ray beam passes horizontally through the infant, who is positioned with suspect side uppermost. The film is placed on the infant’s back, and the infant is placed perpendicular to the bed, facing the x-ray tube. The infant is usually elevated on foam pads or blankets, with the arm positioned above the head and out of the field of view. Free air will rise to the highest portion of the thorax if a pneumothorax is present. If an abdominal perforation is present, free air will also rise above the liver when the infant is positioned with the left side down. A. Radiodensities of various substances and tissues differ according to their composition. 2. A very dense (radiopaque) object such as lead will radiograph gray or white because no rays or few rays will penetrate it, so the film underneath will remain unchanged. 3. Subcutaneous fat is very radiolucent and produces a dark gray shadow on x-ray film. 4. Blood, muscle, and liver are of similar densities and will be seen as white and medium gray. Moist solid or fluid-filled organs and tissue masses have about the same radiodensity—greater than air but less than bone or metal. 5. Bone is composed of an organic matrix into which the complex bone mineral (primarily calcium) is precipitated. Organic substances will reduce the radiodensity of bone and will be seen as white with a tinge of gray. 6. Metal such as the surgical clip used for patent ductus arteriosus ligation is very dense and radiopaque. All the x-rays are absorbed by the metal, producing a white image on the film. B. Differentiation of densities is the basis for interpretation of an x-ray film. For example, because of the contrast in densities between the fluid-filled heart, which radiographs white, and the air-filled lungs, which radiograph black, the heart can be seen against the lungs. Organs of the same density that are located side by side, such as the heart and the thymus, may be difficult to distinguish from each other. Changes in normal density can indicate a pathologic process, such as severe respiratory distress syndrome. Surfactant-deficient lungs will appear on the film completely white instead of black, indicating areas of alveolar collapse. A. Radiation effects and risks (Daldrup-Link and Gooding, 2010). 1. Adverse effects of x-rays do not occur unless a threshold amount of radiation is delivered. 2. Virtually all radiation doses for diagnostic imaging fall below the threshold for adverse effects. B. Risks to personnel. 1. Risks to personnel in the area, when studies and technique are properly done, are low. B. Labeling. Note name or identification of the patient, date and time of the film, and radiographic labeling on right or left side of the film. C. Assess for correct exposure of the film. D. Note positioning. Clavicles and ribs should be even on both sides of the chest. Rotation distorts structures. E. Individually assess all anatomic and pathologic changes on each film. a. Normal lung expansion: eight ribs projecting above the right diaphragmatic dome, with the trachea in a slightly curved, near-midline position. Consider areas of density and areas of lucency (Daldrup-Link and Gooding, 2010). b. Lung volume, determined by noting the number of ribs expanded on an inspiratory film. c. Pulmonary vascularity: vessels branching from the lung root (hilum) and decreasing in size, with extension into the lung fields. Vascularity will be increased or diminished depending on pathologic state. d. Presence of free air: pneumothorax, pneumoperitoneum, pneumopericardium, and pneumomediastinum. 2. Mediastinum. (2) Malposition: any inappropriate position of the heart—that is, any position other than the usual position in the hemithorax. (3) Contour: variable because of the influence of patient position and angulation of the x-ray beam. (4) Shape: may indicate pathologic change—for example, boot-shaped heart in tetralogy of Fallot and egg-shaped heart in transposition of the great vessels (Daldrup-Link and Gooding, 2010). (5) Pulmonary vascular markings: may be significantly diminished, as in pulmonary atresia, or increased, as in congestive heart failure [CHF] (Daldrup-Link and Gooding, 2010). b. Trachea. (1) Normally located within the mediastinum. (2) Assessment on x-ray film for presence and position of endotracheal tube. c. Thymus. (2) Presence or absence. (3) Presense of “sail sign” when mediastinal air lifts the thymus upward. d. Diaphragm. (1) General pattern: two smooth, curved shadows on either side of the heart, taking off from the midline at the origin of the 10th and 11th ribs (Daldrup-Link and Gooding, 2010). (2) Contour: possibly flattened with lung overdistention or elevated if there is abdominal distention. (3) Diaphragmatic hernia: abdominal contents passing through a hole in the diaphragm. (4) Eventration: herniation of bowel and liver against a weakened hemidiaphragm. The diaphragm remains intact but is abnormally elevated. e. Gastrointestinal (GI) tract. (2) Tracheoesophageal fistula. Fistula is present if an esophageal atresia exists and if air is visible in the stomach and intestine. (3) Passage of air through stomach and intestines. (4) Location of stomach bubble. (5) Bowel gas pattern. (6) Presence of pneumatosis intestinalis. (7) Presence of calcifications as a result of bowel perforation in utero. (8) Fluid, seen as a gasless abdomen. It is necessary to distinguish fluid from masses. (9) Pneumoperitoneum. Free air is seen within the peritoneal cavity. (10) Obstructions. Gaseous distention of the bowel is seen at various levels, depending on the location of the obstruction. f. Skeletal system. (2) Fractures of long bones, clavicles, ribs, and skull. A dark line is seen along any portion of a fractured bone because of the air or tissue that settles between the bone fragments (Stedman’s Medical Dictionary, 2013). g. Tubes and catheters. (1) Position of endotracheal tube, gastric tube, or chest tube. (2) Umbilical catheter placement. (3) Central venous line placement. A. The normal chest (Fig. 14-2). 1. Complete aeration of the chest occurs within a few breaths after onset of respirations at delivery (Kenner and Lott, 2007). 2. Residual fluid may be present in the alveoli after delivery. Early films (< 6 hours after delivery) may show increased bronchovascular markings because of this fluid. 3. Normal lung pattern. a. Uniform radiolucent appearance. b. Hilar and perihilar regions show some increased density because of vascular, bronchial, and hilar structures, which produce some increase in density. c. Periphery shows few, if any, markings. d. Fluid in the various interlobar fissures represents a normal variation. B. Thymus. 1. Occupies the anterior part of the superior portion of the mediastinum and consists of right and left lobes (Daldrup-Link and Gooding, 2010). 2. Appears as a smoothly rounded outline superior to the cardiac shadow and blending imperceptibly with the cardiac silhouette. 3. Definite notch visible in some cases at the junction of the cardiac silhouette and the thymus. 4. Generally more prominent on the right. 5. Shape may alter markedly with degree of inspiration. 6. Rapid involution during times of stress. 7. Aplasia of the thymus (DiGeorge syndrome). 8. Creation of “sail sign” when mediastinal air lifts the thymus upward. C. Trachea. 1. Trachea is normally displaced slightly to the right by the left aortic arch. 2. Deviated trachea supports a mediastinal shift. 3. On inspiration, the trachea dilates and lengthens. 4. On expiration, the trachea constricts and shortens. 5. On deep inspiration, the trachea and major bronchi are well distended and are easily identifiable. A. Respiratory distress syndrome (hyaline membrane disease) (Fig. 14-3, A). 2. Bilateral diffuse alveolar infiltrates. Reticulogranular (ground-glass) appearance is due to microatelectasis of the alveoli (Kenner and Lott, 2007). 3. Homogeneous pattern throughout both lung fields. 4. Air bronchograms. Air-filled bronchi (black) are contrasted against the more radiopaque (whiter) lung fields (Daldrup-Link and Gooding, 2010). 5. With severe disease, a generalized opacity or frank “white-out” appearance (see Fig. 14-3, B). 6. Reticulogranular pattern and air bronchograms. May resemble those seen in group B streptococcal pneumonia and may be impossible to distinguish from respiratory distress syndrome. 7. X-ray findings after surfactant administration (Fig. 14-4). a. Improvement in pulmonary aeration on x-ray. b. Asymmetrical distribution of surfactant, showing areas of improved lung alternating with areas of unchanged respiratory distress syndrome (RDS). c. Poor prognosis with pulmonary interstitial emphysema after surfactant therapy. B. Transient tachypnea of the newborn (retained fetal lung fluid, wet lung disease) (Fig. 14-5). 1. Bilateral, symmetrical perihilar streakiness due to increased interstitial and alveolar fluid (Fanaroff and Martin, 2010). 2. Mild to moderate overaeration of the lungs and streaky appearing densities (Daldrup-Link and Gooding, 2010). 3. Possible fluid in minor (or horizontal) fissure and major (or oblique) lobar fissure. 4. Mildly enlarged cardiothymic silhouette. 5. Lung fields begin to clear in 24 to 48 hours. C. Bronchopulmonary dysplasia (BPD) (Fig. 14-6). 1. Initial x-ray picture shows lung disease (e.g., RDS, meconium aspiration syndrome). 2. Radiologic appearance and course of BPD have changed since Northway and Rosan (1968) described their four stages. b. Subsequently there is gradual development of a bubbly appearance of the lungs in association with hyperaeration, which is more pronounced at the lung bases. This persists after 1 month of age and represents a modified form of BPD (Fanaroff and Martin, 2010). D. Pulmonary interstitial emphysema (Fig. 14-7). 1. Alveolar overdistention is due to assisted ventilation, visualized as multiple small, cystlike radiolucencies that are bilateral, unilateral, localized, or in a diffuse pattern (Kenner and Lott, 2007). 2. Condition may lead to a pneumothorax or other air leak. E. Meconium aspiration syndrome (Fig. 14-8). 1. Mild cases may show a normal lung pattern to mild infiltrates with overexpanded lungs. 2. Bilateral asymmetrical areas of atelectasis; hyperaeration and air trapping due to debris, with flattened hemidiaphragms (Daldrup-Link and Gooding, 2010). 3. Possible air leaks (pneumothorax or pneumomediastinum) resulting from overdistention and rupture of the alveoli. F. Pneumonia. 1. Occasionally asymmetrical, patchy, or streaky bilateral interstitial infiltrate. A nodular pattern may predominate in hazy lungs, and an effusion is a common occurrence (Daldrup-Link and Gooding, 2010). 2. Reticulogranular pattern similar to that of RDS. Some alveoli contain inflammatory exudate, which will appear more opaque on x-ray than those filled with air (Daldrup-Link and Gooding, 2010). 3. Group B streptococcal pneumonia is often difficult to diagnose on x-ray due to variable lung volumes and variable densities. May be indistinguishable from RDS (Kenner and Lott, 2007) (Fig. 14-9).
Radiologic Evaluation
BASIC CONCEPTS
TERMINOLOGY
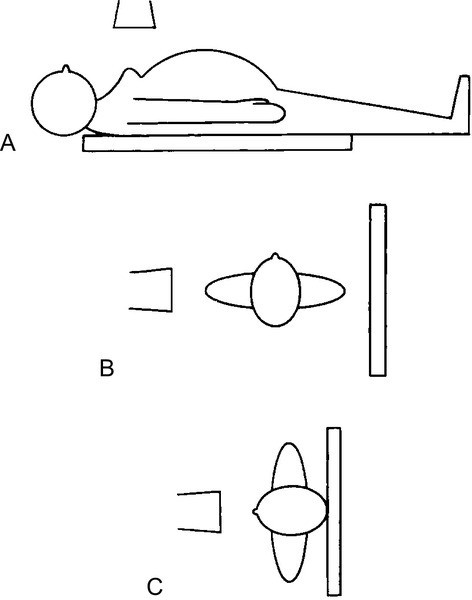
X-RAY VIEWS COMMONLY USED IN THE NEWBORN INFANT (FIG. 14-1)
RADIOGRAPHIC DENSITIES
RISKS ASSOCIATED WITH RADIOGRAPHIC EXAMINATION IN THE NEONATE
APPROACH TO INTERPRETING AN X-RAY
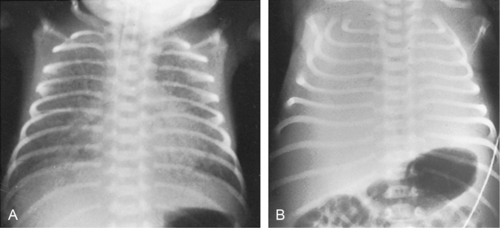
RESPIRATORY SYSTEM

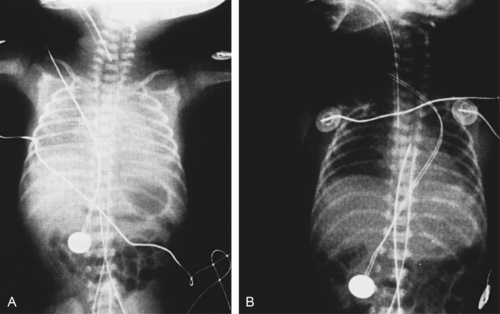
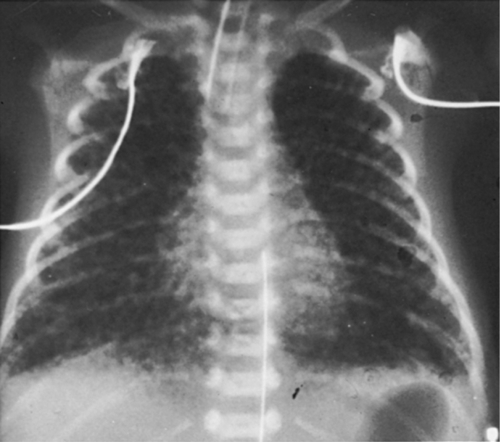
PULMONARY PARENCHYMAL DISEASE


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


14: Radiologic Evaluation
FIGURE 14-1 ■ X-ray views commonly used for the newborn infant. A, Anteroposterior view. B, Cross-table lateral view. C, Lateral decubitus view. (Courtesy Peter Honeyfield, M.D.)
FIGURE 14-2 ■ Normal appearance of chest on x-ray film.
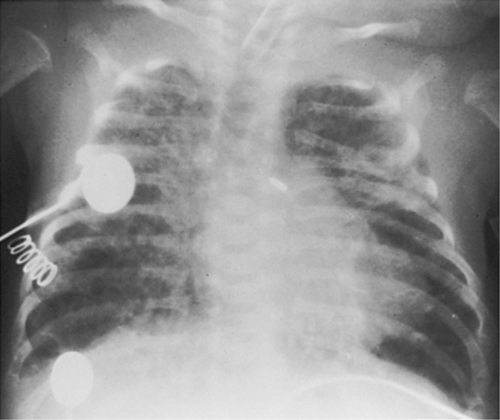
FIGURE 14-3 ■ A, Hyaline membrane disease. Note reticulogranular lung pattern and air bronchograms. B, Severe hyaline membrane disease. Note “white-out” appearance bilaterally with faint air bronchograms visible.
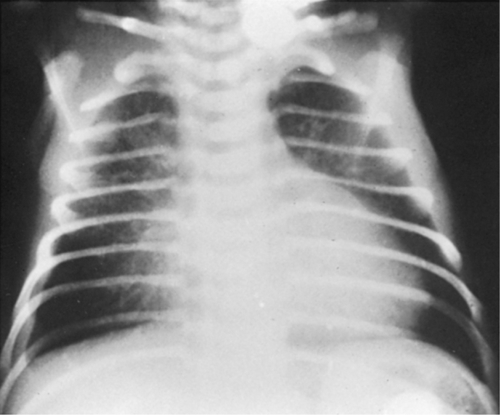
FIGURE 14-4 ■ Hyaline membrane disease before administration of surfactant (A) and significant clearing after administration (B).
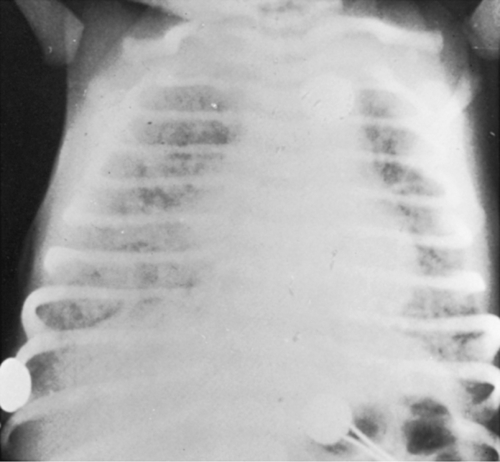
FIGURE 14-5 ■ Transient tachypnea of the newborn. Note mild hyperexpansion and perihilar streakiness. A small pleural effusion is also present on right side.
FIGURE 14-6 ■ Bronchopulmonary dysplasia. Note ill-defined densities bilaterally. Also note fractured rib in upper left portion of chest and pale-appearing ribs.
FIGURE 14-7 ■ Pulmonary interstitial emphysema. Note hyperexpansion bilaterally and pinpoint dark bubbles throughout both lung fields.
FIGURE 14-8 ■ Meconium aspiration syndrome. Note coarse, patchy infiltrates bilaterally.
FIGURE 14-9 ■ Group B streptococcal pneumonia. Note reticulogranular appearance seen with hyaline membrane disease.
