Barbara Lauritsen Christensen
Care of the patient with a neurologic disorder
Objectives
1. Name the two structural divisions of the nervous system and give the functions of each.
2. List the parts of the neuron, and describe the function of each part.
6. List physiologic changes that occur in the nervous system with aging.
10. Discuss the Glasgow coma scale
11. List common laboratory and diagnostic examinations for evaluation of neurologic disorders.
13. Discuss various neurologic disturbances in motor function and sensory-perceptual function.
17. Differentiate between trigeminal neuralgia and Bell’s palsy.
19. Explain the mechanism of injury to the brain that occurs with a stroke and traumatic brain injury.
Key terms
bradykinesia (br -d
-d -k
-k -N
-N -z
-z –
– , p. 683)
, p. 683)
deep brain stimulation (DBS) (p. 685)
dysarthria (d s-
s- HR-thr
HR-thr –
– , p. 659)
, p. 659)
Glasgow coma scale (GL S-g
S-g K
K -m
-m sk
sk l, p. 658)
l, p. 658)
global cognitive dysfunction (GL -b
-b l K
l K G-n
G-n -t
-t v d
v d s-F
s-F NK-sh
NK-sh n, p. 706)
n, p. 706)
Guillain-Barré syndrome (GBS) (G -y
-y b
b -R
-R , p. 703)
, p. 703)
hemianopia (h m-
m- –
– -N
-N -p
-p –
– , p. 661)
, p. 661)
hemiplegia (h m-
m- -PL
-PL -j
-j , p. 673)
, p. 673)
hyperreflexia (h -p
-p r-r
r-r -FL
-FL K-s
K-s –
– , p. 710)
, p. 710)
nystagmus (n s-T
s-T G-m
G-m s, p. 681)
s, p. 681)
postictal period (p st-
st- K-t
K-t l P
l P -r
-r –
– d, p. 676)
d, p. 676)
proprioception (pr -pr
-pr –
– -S
-S P-sh
P-sh n, p. 661)
n, p. 661)
unilateral neglect ( -n
-n -L
-L T-
T- r-
r- l n
l n -GL
-GL CT, p. 661)
CT, p. 661)
Anatomy and physiology of the neurologic system
The nervous system is responsible for communication and control within the body. It interprets or processes the information received and sends it to the appropriate area of the brain or spinal cord, where the response is generated. The nervous system is the body’s link with the environment. It works in conjunction with the endocrine system to maintain the body’s homeostasis. The nervous system reacts in split seconds, whereas the hormones secreted by the endocrine glands work more slowly in initiating a response. The clinical picture for the patient with neurologic problems is often complex. Understanding these conditions requires knowledge of the anatomy and physiology of the nervous system.
Structural divisions
The nervous system has two main structural divisions. The first division, the central nervous system (CNS), is made up of the brain and the spinal cord. It occupies a medial position in the body and is responsible for interpreting incoming sensory information and issuing instructions based on past experiences. The second component is the peripheral nervous system, which lies outside the CNS.
The peripheral nervous system contains two main divisions: the somatic nervous system and the autonomic nervous system. The somatic nervous system sends messages from the CNS to the skeletal muscles (voluntary muscles). The autonomic system transmits messages from the CNS to the smooth muscle, the cardiac muscle, and certain glands. The autonomic system is sometimes called the involuntary nervous system because its action takes place without conscious control.
Cells of the nervous system
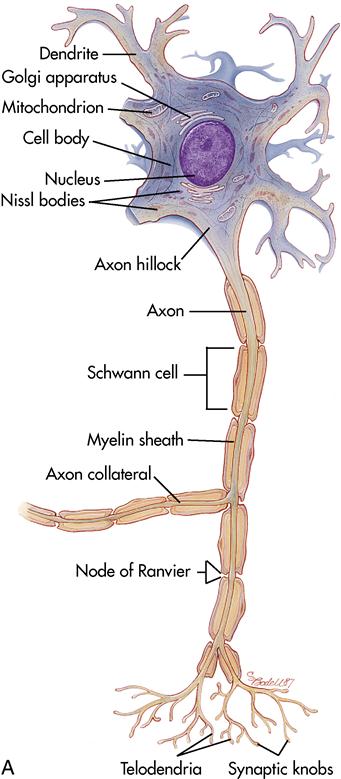
Two broad categories of cells exist within the nervous system. The first category, the neurons, are the transmitter cells (Figure 14-1). They carry messages to and from the brain and spinal cord. The second category, the neuroglial or glial cells, are the support cells to the neurons. They support and protect the neurons while producing cerebrospinal fluid (CSF), which continuously bathes the structures of the CNS.
Neuron
A neuron (nerve cell) is the basic cell of the nervous system. It is a separate unit composed of three main structures: the cell body, the axon, and the dendrites. The cell body contains a nucleus surrounded by cytoplasm. The axon is a cylindric extension of a nerve cell that conducts impulses away from the neuron cell body. The dendrites are branching structures that extend from a cell body and receive impulses. Between each neuron is a gap (space) called the synapse, defined as the region surrounding the point of contact between two neurons or between a neuron and an effector organ, across which nerve impulses are transmitted through the action of a neurotransmitter.
All neurons are governed by the “all or none law,” which means there is never a partial transmission of a message; the impulse is either strong enough to elicit a response or too weak to generate the message.
Neuromuscular junction
The area of contact between the ends of a large myelinated nerve fiber and a fiber of skeletal muscle is called the neuromuscular junction. This area of contact is necessary for the body to function. The neurotransmitters act to make certain that the neurologic impulse passes from the nerve to the muscle.
Neurotransmitters
Numerous chemicals called neurotransmitters modify or result in the transmission of impulses between synapses. The best-known neurotransmitters are acetylcholine, norepinephrine, dopamine, and serotonin.
Acetylcholine plays a role in nerve impulse transmission; it spills into the synapse area and speeds the transmission of the impulse. The enzyme cholinesterase is then released to deactivate the acetylcholine once the message or impulse has been sent. This happens rapidly and continuously as each impulse is relayed.
Norepinephrine has an effect on maintaining arousal (awakening from a deep sleep), dreaming, and regulation of mood (e.g., happiness, sadness).
Dopamine primarily affects motor function; it is involved in gross subconscious movements of the skeletal muscles. It also plays a role in emotional responses. A person with Parkinson’s disease has decreased dopamine levels and suffers tremors, or involuntary, trembling muscle movements.
Serotonin induces sleep, affects sensory perception, controls temperature, and has a role in control of mood.
Neuron coverings
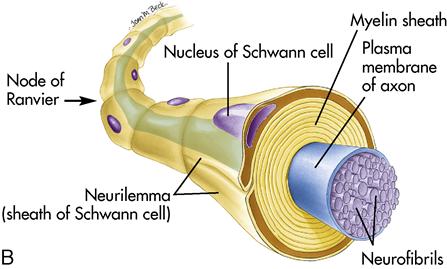
Many neuron fibers (axons and dendrites) (see Figure 14-1) are covered with a white, waxy, fatty material called myelin. Myelin increases the rate of transmission of impulses and protects and insulates the fibers. Axons leaving the CNS are wrapped in layers of myelin with indentations called the nodes of Ranvier. These nodes further increase the rate of transmission because the impulse can jump from node to node.
In the peripheral nervous system the myelin is produced by Schwann cells (see Figure 14-1). The outer membrane of the Schwann cells gives rise to another layer called the neurilemma. The neurilemma is important because it helps regenerate injured axons. Thus regeneration of nerve cells occurs only in the peripheral nervous system. Cells damaged in the CNS result in permanent damage (paralysis) because they do not have neurilemma and are not able to regenerate.
Central nervous system
The CNS—one of the two main divisions of the nervous system, composed of the brain and the spinal cord—functions somewhat like a computer but is much more complex. The cranium protects the brain, and the vertebral column protects the spinal cord.
Brain
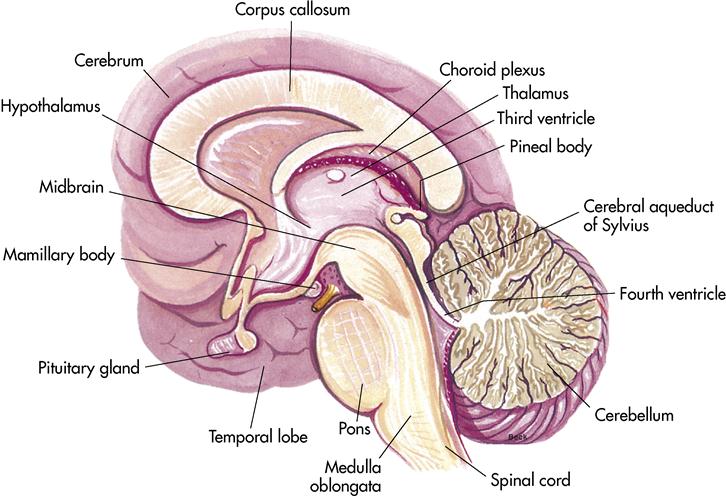
Specialized cells in the brain’s mass of convoluted, soft, gray or white tissue coordinate and regulate the functions of the CNS. The brain is one of the largest organs, weighing approximately 3 pounds (1.4 kg). It is divided into four principal parts: the cerebrum, the diencephalon, the cerebellum, and the brainstem.
Cerebrum
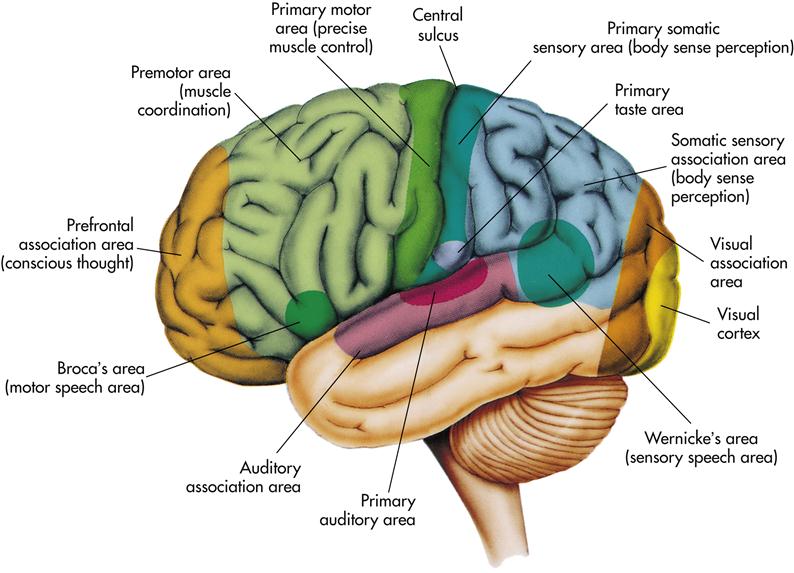
The cerebrum is the largest part of the brain (Figure 14-2). It is divided into the left and right hemispheres. The outer portion of the cerebrum is composed of gray matter and is called the cerebral cortex. It is arranged in folds, called gyri (convolutions); the grooves are called sulci (fissures). The connecting structure or bridge is called the corpus callosum. Two deep sulci subdivide the two hemispheres into four lobes that are named for the bones lying over them: the frontal lobe, the parietal lobe, the temporal lobe, and the occipital lobe. Each hemisphere of the cerebrum controls initiation of movement on the opposite side of the body. The functions of the cerebrum are multiple and complex. Specific areas of the cerebral cortex are associated with specific functions (Figure 14-3, Box 14-1).
Basal ganglia
The basal ganglia are additional bands of gray matter buried deep within the two cerebral hemispheres that form the subcortical associated motor system (the extrapyramidal system). They control automatic movement of the body associated with skeletal muscle activity (e.g., the arms swing alternating with the legs during walking; swallowing; saliva; and blinking) (Lewis et al., 2007).
Diencephalon
The diencephalon is often called the interbrain. It lies beneath the cerebrum and contains the thalamus and the hypothalamus. The thalamus serves as a relay station on the way to the cerebral cortex for some sensory impulses; it interprets other sensory messages, such as pain, light touch, and pressure. The hypothalamus, which lies beneath the thalamus, plays a vital role in the control of body temperature; fluid balance; appetite; sleep; and certain emotions, such as fear, pleasure, and pain. Both the sympathetic and parasympathetic divisions of the autonomic system are under the control of the hypothalamus, as is the pituitary gland. Thus the hypothalamus influences the heartbeat, the contraction and relaxation of the walls of the blood vessels, hormone secretion, and other vital body functions (see Figure 14-2).
Cerebellum
The cerebellum lies posterior and inferior to the cerebrum and is the second largest portion of the brain. It contains two hemispheres with a convoluted surface much like the cerebrum. It is mainly responsible for coordination of voluntary movement and maintenance of balance, equilibrium, and muscle tone. It coordinates and smoothes movement (e.g., the complex and quick coordination of many different muscles needed in playing the piano, swimming, or juggling). It is like the automatic pilot on an airplane in that it adjusts and corrects the voluntary movement, but operates entirely below the conscious level (Jarvis, 2008). Sensory messages from the semicircular canals in the inner ear send their messages to the cerebellum (see Figure 14-2).
Brainstem
The brainstem is located at the base of the brain and contains the midbrain, the pons, and the medulla oblongata (see Figure 14-2). These structures connect the spinal cord and the cerebrum. The brainstem carries all nerve fibers between the spinal cord and the cerebrum.
Midbrain
The midbrain forms the superior portion of the brainstem. It merges into the thalamus and the hypothalamus. It is responsible for motor movement, relay of impulses, and auditory and visual reflexes. It is the origin of cranial nerves III and IV.
Pons
The pons connects the midbrain to the medulla oblongata; the word pons means “bridge.” It is the origin of cranial nerves V through VIII. The pons is composed of myelinated nerve fibers and is responsible for sending impulses to the structures that are inferior and superior to it. It also contains a respiratory center that complements respiratory centers located in the medulla.
Medulla oblongata
The medulla oblongata is the distal portion of the brainstem. It is the origin of cranial nerves IX and XII. The medulla controls heartbeat, rhythm of breathing, swallowing, coughing, sneezing, vomiting, and hiccups (singultus). A vasomotor center regulates the diameter of the blood vessels, which aids in the control of blood pressure.
Coverings of the brain and the spinal cord
The brain and the spinal cord are surrounded by three protective coverings called the meninges: (1) the dura mater, the outermost layer; (2) the arachnoid membrane, the second layer; and (3) the pia mater, the innermost layer, which provides oxygen and nourishment to the nervous tissue. These layers also bathe the spinal cord and the brain in CSF.
Ventricles
The four ventricles are spaces or cavities located in the brain. The CSF, which is clear and resembles plasma, flows into the subarachnoid spaces around the brain and the spinal cord and cushions them. It contains protein, glucose, urea, and salts; it also contains certain substances that form a protective barrier (the blood-brain barrier) that prevents harmful substances from entering the brain and the spinal cord.
Spinal cord
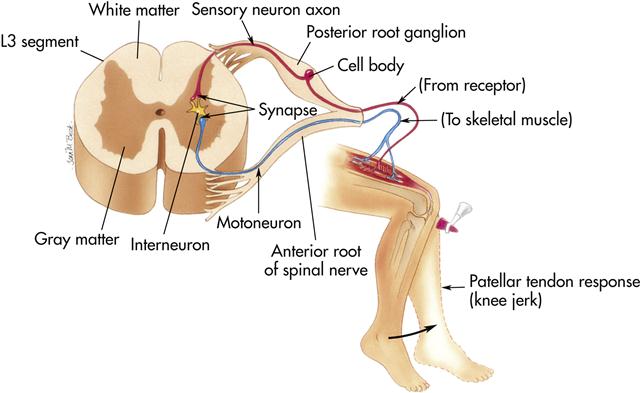
The spinal cord is a 17- to 18-inch cord that extends from the brainstem to the second lumbar vertebra. It has two main functions: conducting impulses to and from the brain and serving as a center for reflex actions such as a knee jerk (Figure 14-4). A sensory neuron sends the information to the cord, a central neuron (located within the cord) interprets the impulse, and a motoneuron sends the message back to the muscle or organ involved. Thus a message is sent, interpreted, and acted on without traveling to the brain.
Peripheral nervous system
The peripheral nervous system is made up of the motor nerves, the sensory nerves, and ganglia outside the brain and the spinal cord. It is composed of 31 pairs of spinal nerves, 12 pairs of cranial nerves, and the autonomic nervous system.
Spinal nerves
The 31 pairs of spinal nerves are all mixed nerves. This means that they transmit sensory information to the spinal cord through afferent neurons and motor information from the CNS to the various areas of the body through efferent neurons. The spinal nerves are named according to the corresponding vertebra (e.g., C1, C2).
Cranial nerves
There are 12 pairs of cranial nerves, which attach to the posterior surface of the brain, mainly the brainstem. Eleven of the pairs conduct impulses between the head, the neck, and the brain; the vagus nerve (X) also serves organs in the thoracic and abdominal cavities (Figure 14-5). Table 14-1 lists the cranial nerves, their impulses, and functions.
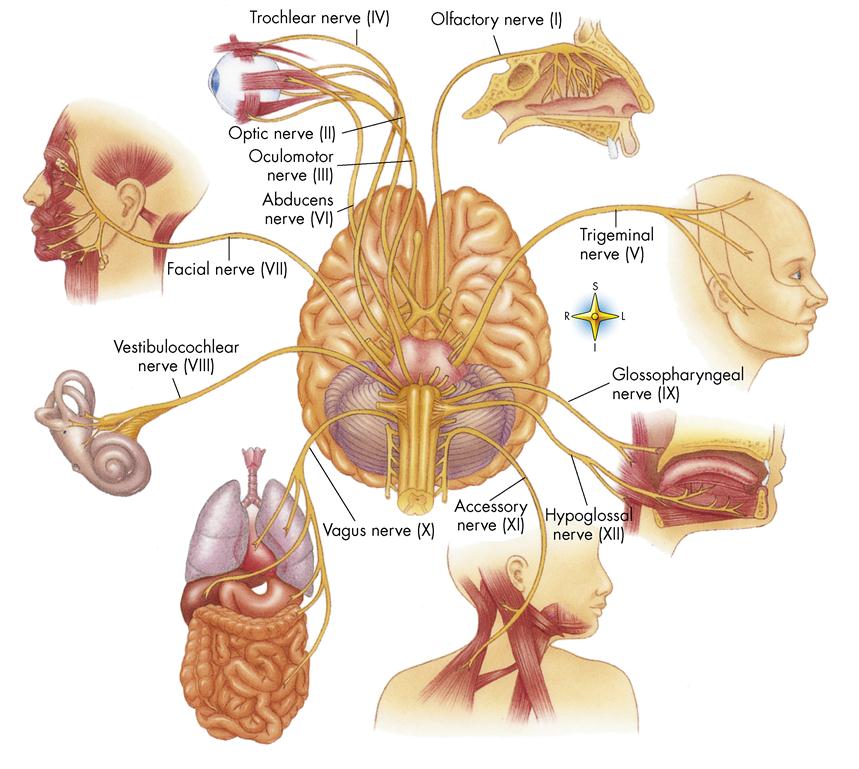
Table 14-1
| NERVE* | CONDUCTS IMPULSES | FUNCTIONS | |
| I | Olfactory | From nose to brain | Sense of smell |
| II | Optic | From eye to brain | Vision |
| III | Oculomotor | From brain to eye muscles | Eye movements, extraocular muscles, pupillary control (pupillary constriction) |
| IV | Trochlear | From brain to external eye muscles | Down and inward movement of eye |
| V | From skin and mucous membrane of head to brain; from teeth to brain; from brain to chewing muscles | Sensations of face, scalp, and teeth; chewing movements | |
| VI | Abducens | From brain to external eye muscles | Lateral movement of eye |
| VII | Facial | From taste buds of tongue to brain; from brain to facial muscles | Sense of taste on anterior two thirds of tongue; contraction of muscles of facial expression |
| VIII | Acoustic (vestibulocochlear) | From ear to brain | Hearing; sense of balance (equilibrium) |
| IX | Glossopharyngeal | From throat and taste buds of tongue to brain; from brain to throat muscles and salivary glands | Sensations of throat, taste, swallowing movements, gag reflex, taste posterior one third of tongue, secretion of saliva |
| X | Vagus | From throat, larynx, and organs in thoracic and abdominal cavities to brain; from brain to muscles of throat and to organs in thoracic and abdominal cavities | Sensations of throat, larynx, and thoracic and abdominal organs; swallowing, voice production, slowing of heartbeat, acceleration of peristalsis |
| XI | Spinal accessory | From brain to certain shoulder and neck muscles | Shoulder movements (trapezius muscle) and turning movements of head (sternocleidomastoid muscles) |
| XII | Hypoglossal | From brain to muscles of tongue | Tongue movements |
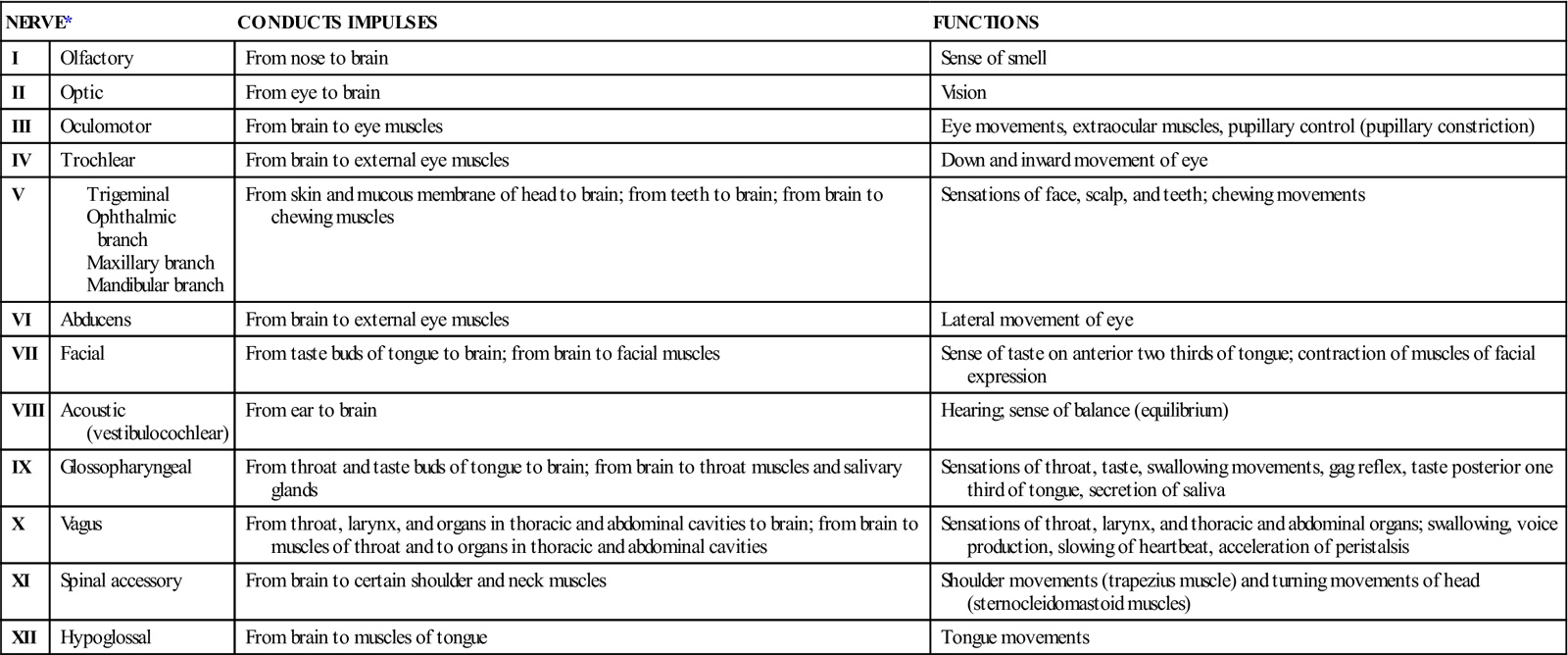
*The first letter of the words in the following sentence are the first letters of the names of cranial nerves: “On Old Olympus’s Towering Tops A Finn And German Viewed Some Hops.” Many generations of students have used this or a similar mnemonic to help them remember the names of cranial nerves.
Autonomic nervous system
The autonomic nervous system controls the activities of the smooth muscle, the cardiac muscle, and all glands. The autonomic nervous system is not a separate nervous system but a subdivision of the peripheral nervous system.
It is misleading to think of this system as the automatic system, although most activity is performed on an unconscious level. Its primary function is to maintain internal homeostasis; for example, it strives to maintain a normal heartbeat, a constant body temperature, and a normal respiratory pattern.
To maintain this homeostasis, the autonomic system has two divisions: the sympathetic nervous system and the parasympathetic nervous system. These two divisions are antagonistic: one slows an action, and the other accelerates the action. These systems function simultaneously, but they are able to dominate each other as the need arises. In times of stress the sympathetic system takes over to prepare the body for “fight or flight.” Heartbeat accelerates, blood pressure rises, and adrenal glands increase their secretions. To calm the body after a crisis, the parasympathetic system becomes dominant, slowing the heartbeat and decreasing the blood pressure and adrenal hormone output.
Effects of normal aging on the nervous system
The effects of aging on the nervous system are variable. The changes that occur include a loss of brain weight and a substantial loss of neurons (1% a year after age 50), with the cortex losing cells faster than the brainstem. The remaining cells undergo structural changes. Aging also brings about a general decline in interconnections of dendrites, a reduction in cerebral blood flow, and a decrease in brain metabolism and oxygen utilization. The neurons may contain senile plaques, neurofibrillary tangles, and the age pigment lipofuscin. Older adults often have an altered sleep/wakefulness ratio, a decrease in the ability to regulate body temperature, and a decrease in the velocity of nerve impulses. The blood supply to the spinal cord is decreased, resulting in slower reflexes.
Normal changes in the nervous system associated with aging are not the same as senility, organic brain disease, or Alzheimer’s disease (AD). Many older people reach old age with no functional deterioration of the nervous system. However, these normal changes may make care or rehabilitation of the older patient a challenge (see Life Span Considerations box).
Prevention of neurologic problems
Many conditions of the nervous system have no known cause. Other neurologic problems can be prevented or their effects reduced by modifying lifestyle factors. Neurovascular diseases are in part associated with defined risk factors—the same factors that increase the risk of cardiac disease, including high blood pressure, high blood cholesterol levels, cigarette smoking, obesity, stress, and lack of exercise.
Avoidance of cigarette smoking has been found to decrease the incidence of lung cancer. This is significant for the nervous system, because cancer of the lung often metastasizes to the brain.
Prevention of neurologic problems resulting from trauma is a major challenge. These injuries include spinal cord injury and head injury, which occur frequently in young people. Patient teaching on avoiding such injuries should include avoidance of drug and alcohol use, safe use of motor vehicles (e.g., using automobile seatbelts; wearing helmets with bicycles, motorcycles, and snowmobiles), safe swimming practices (e.g., not diving in shallow water), safe handling and storage of firearms, use of hardhats in dangerous construction areas, and use of protective gear as needed for sports (see Safety Alert box).
Neurologic diseases, such as meningitis or brain abscess, that occur as a result of infection can sometimes be prevented by prompt treatment of ear and sinus infections. The practice of safe and responsible sex is important, since some neurologically related diseases, such as syphilis and human immunodeficiency virus (HIV) disease, are spread by sexual contact. Safe practices include abstinence, monogamy, and the use of condoms. Treatment for drug abuse, especially intravenous (IV) use, is important, as is the prevention of HIV disease.
Assessment of the neurologic system
History
A comprehensive history is essential for diagnosing neurologic disease. This includes specifics about symptoms experienced and the patient’s understanding and perception of what is happening. Obtaining information from family members or significant others may also be helpful. Follow the same format routinely to make certain information is complete.
For patients with suspected neurologic conditions, the presence of many symptoms or subjective data may be significant. These include the following.
Mental status
Assessment of the neurologic patient’s mental status generally includes orientation (person, place, time, and purpose), mood and behavior, general knowledge (such as the names of U.S. presidents), and short- and long-term memory. The patient’s attention span and ability to concentrate may also be assessed.
It is important to document mental status in specific terms. For instance, it is better to note “oriented to name, date, hospital, and purpose” than to note simply “oriented.” Record actual patient statements. Vary orientation questions because some patients may learn the correct answers through repetition.
Level of consciousness
Level of consciousness (LOC) is the earliest and most sensitive indicator of the patient’s neurologic status. Changes in LOC are a result of impaired cerebral blood flow, which deprives the cells of the cerebral cortex and the reticular activating system (RAS) of oxygen. The RAS is located in the brainstem with neural connections to many parts of the nervous system (Lewis et al., 2007). The RAS is a functional system in the brain essential for wakefulness, attention, concentration, and introspection (Mosby’s Dictionary of Medicine, Nursing, and Health Professions, 2006). A decreasing LOC is the earliest sign of increased intracranial pressure (ICP). LOC has two components: arousal (or wakefulness) and awareness. Wakefulness is the most fundamental part of LOC. If the patient can open the eyes spontaneously to voice or to pain, the wakefulness center in the brainstem is still functioning. Awareness, a higher function controlled by the RAS in the brainstem, is the ability to interact with and interpret the environment. Awareness has four components, which are assessed as follows:
1. Orientation: Ask questions about orientation to person, place, time, and purpose.
2. Memory: Assess short-term memory; do not ask yes or no questions.
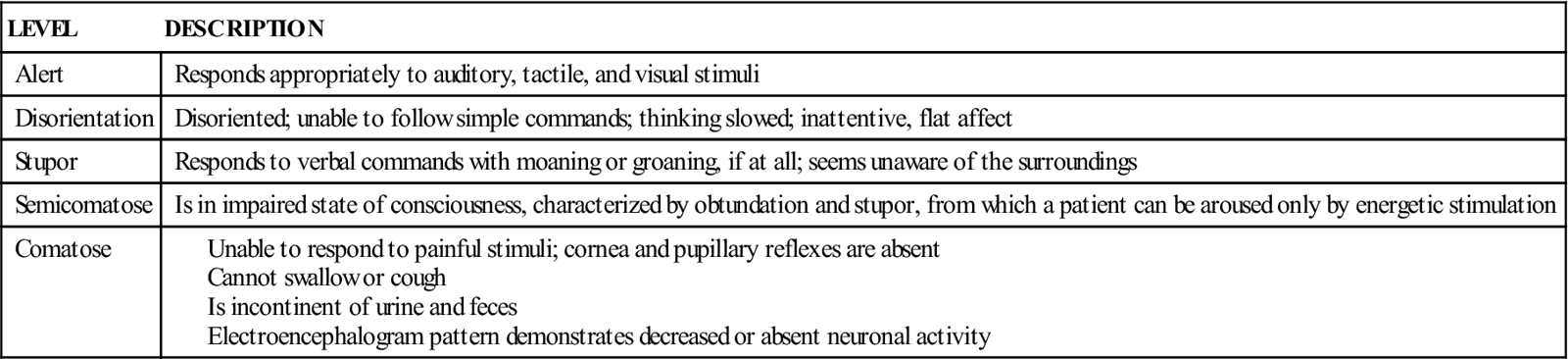
Restlessness, disorientation, and lethargy may be seen first. Record observations in terms of behavior and signs—not labels such as “disoriented.” See Table 14-2 for one method of classifying LOC.
Table 14-2
Glasgow coma scale
The Glasgow coma scale (Table 14-3) is a quick, practical, and standardized system for assessing the degree of consciousness impairment in the critically ill and for predicting the duration and ultimate outcome of coma, particularly with head injuries. The Glasgow coma scale was developed in 1974 and consists of a three-part neurologic assessment: eye opening, best motor response, and best verbal response.
Table 14-3
Glasgow Coma Scale: Demonstrating Measurement of Level of Consciousness
| CATEGORY OF RESPONSE | APPROPRIATE STIMULUS | RESPONSE | SCORE |
| Eyes Open | Spontaneous response | 4 | |
| Opening of eyes to name or command | 3 | ||
| Lack of opening of eyes to previous stimuli but opening to pain | 2 | ||
| Lack of opening of eyes to any stimulus | 1 | ||
| Untestable | U | ||
| Best Verbal Response | Appropriate orientation, conversant; correct identification of self, place, year, and month | 5 | |
| Confusion; conversant, but disorientation in one or more spheres | 4 | ||
| Inappropriate or disorganized use of words (e.g., cursing), lack of sustained conversation | 3 | ||
| Incomprehensible words, sounds (e.g., moaning) | 2 | ||
| Lack of sound, even with painful stimuli | 1 | ||
| Untestable | U | ||
| Best Motor Response | Obedience of command | 6 | |
| Localization of pain, lack of obedience but presence of attempts to remove offending stimulus | 5 | ||
| Flexion withdrawal,* flexion of arm in response to pain without abnormal flexion posture | 4 | ||
| Abnormal flexion, flexing of arm at elbow and pronation, making a fist | 3 | ||
| Abnormal extension, extension of arm at elbow usually adduction and internal rotation of arm at shoulder | 2 | ||
| Lack of response | 1 | ||
| Untestable | U |
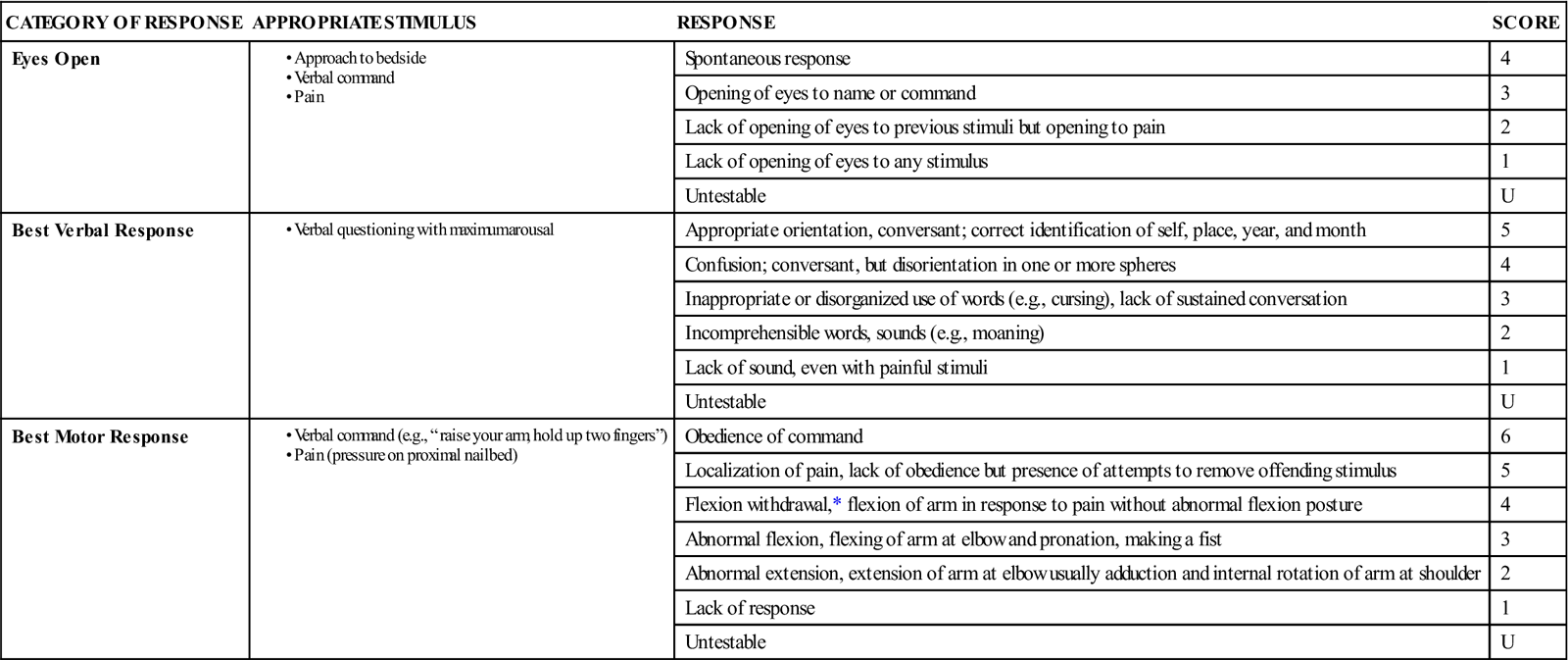
*Added to the original scale by many centers.
From Lewis, S.L., et al. (2007). Medical-surgical nursing: Assessment and management of clinical problems. (7th ed.). St. Louis: Mosby.
The stronger the stimulus needed to obtain a response, the lower the patient’s score. The number value assigned to each part of the scale is added to yield an objective score. The score for a patient who is not neurologically impaired is 15; the lowest possible score is 3. Generally, any score of 8 or less is commonly accepted as a definition of coma. The scale has a high degree of consistency even when used by staff of varied experience.
Four score coma scale
A recently developed scale for assessing coma is the FOUR (Full Outline of UnResponsiveness) Score coma scale (Wijdicks & Bamlet, 2005). It is used to assess patients with neurologic conditions that affect cognitive function such as stroke, craniotomy, and traumatic brain injury. It assesses eye response, motor response, brainstem reflexes, and respiration (Table 14-4). Each component is graded on a scale of 0 (worst response) to 4 (best response). The scores are not totaled; therefore there is not a sum score in this scale.
Table 14-4
| CATEGORY OF RESPONSE | RESPONSE | SCORE |
| Eyelids open or opened, tracking, or blinking to command | 4 | |
| Eyelids open but not tracking | 3 | |
| Eyelids closed, open to loud noise, not tracking | 2 | |
| Eyelids closed, open to pain, not tracking | 1 | |
| Eyelids remain closed with pain | 0 | |
| Pupil and corneal reflexes present | 4 | |
| One pupil wide and fixed | 3 | |
| Pupil or corneal reflexes absent | 2 | |
| Pupil and corneal reflexes absent | 1 | |
| Absent pupil, corneal, and cough reflex | 0 | |
| Thumbs up, fist or peace sign, to command | 4 | |
| Localizing to pain | 3 | |
| Flexion response to pain | 2 | |
| Extensor posturing | 1 | |
| No response to pain or generalized myoclonus status epilepticus | 0 | |
| Not intubated, regular breathing pattern | 4 | |
| Not intubated, Cheyne-Stokes breathing pattern | 3 | |
| Not intubated, irregular breathing pattern | 2 | |
| Breathes above ventilator rate | 1 | |
| Breathes at ventilator rate or apnea | 0 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



 g-N
g-N -zh
-zh ,
,  N-
N- r-
r- -z
-z m,
m,  -F
-F -z
-z –
– ,
,  -PR
-PR K-s
K-s –
– ,
,  -T
-T K-s
K-s –
– ,
,  W-r
W-r ,
,  -PL
-PL -p
-p –
– ,
,  s-F
s-F -j
-j –
– ,
,  K-s
K-s d,
d,  -R
-R -s
-s s,
s,  S-t
S-t k,
k,  k,
k,