Preterm and Postterm Newborns
Objectives
1. Define each key term listed.
2. Differentiate between the preterm and the low-birth-weight newborn.
3. List three causes of preterm birth.
5. Describe the symptoms of cold stress and methods of maintaining thermoregulation.
6. Contrast the techniques for feeding preterm and full-term newborns.
7. Discuss two ways to help facilitate maternal-infant bonding for a preterm newborn.
8. Describe the family reaction to preterm infants and nursing interventions.
Key Terms
apnea (ĂP-nē-ă, p. 309)
Ballard scoring system (p. 306)
bradycardia (brād-ĕ-KĂHR-dē-ă, p. 309)
bronchopulmonary dysplasia (brŏn-kō-PŬL-mŏ-năr-ē dĭs-PLĀ-zhă, p. 309)
cold stress (p. 310)
gestational age (p. 306)
hyperbilirubinemia (hī-pŭr-bĭl-ē-rū-bĭ-NĒ-mē-ă, p. 312)
hypocalcemia (hī-pō-kăl-SĒ-mē-ă, p. 310)
hypoglycemia (hī-pō-glī-SĒ-mē-ă, p. 310)
hypoxia (p. 309)
icterus (ĬK-tŭr-ŭs, p. 312)
kangaroo care (p. 314)
lanugo (lă-NŪ-gō, p. 318)
late preterm (p. 306)
necrotizing enterocolitis (NEC) (NĔK-rō-tīz-ĭng ĕn-ĕr-ō-kō-LĪ-tĭs, p. 311)
neutral thermal environment (p. 313)
postterm (p. 306)
preterm (p. 306)
previability (p. 306)
pulse oximetry (p. 309)
respiratory distress syndrome (RDS) (p. 307)
retinopathy of prematurity (ROP) (p. 311)
sepsis (SĔP-sĭs, p. 310)
surfactant (sŭr-FĂK-tănt, p. 307)
thermoregulation (p. 313)
total parenteral nutrition (TPN) (TŌT-ăl pă-RĔN-tŭr-ăl nū-TRĬ-shŭn, p. 316)
![]() http://evolve.elsevier.com/Leifer
http://evolve.elsevier.com/Leifer
The Preterm Newborn
The preterm (also known as premature) newborn is the most common admission to the intensive care nursery. With increased specialization and sophisticated monitoring techniques, many infants who in the past would have died are now surviving. The nurse’s role continues to be increasingly complex, with greater emphasis placed on subtle clinical observations and technology. In acquainting the student with the preterm infant, one goal of this chapter is to encourage an appreciation of the preterm infant’s struggle for survival and the intense responsibility placed on those entrusted with his or her care. The words preterm and premature are used synonymously, although the former is now considered more accurate. Any newborn whose life or quality of existence is threatened is considered to be in a high-risk category and requires close supervision by professionals in a special neonatal intensive care unit (NICU). Preterm newborns constitute a majority of these patients. Preterm birth is responsible for more deaths during the first year of life than any other single factor. Preterm infants also have a higher percentage of birth defects. Prematurity and low birth weight are often concomitant, and both factors are associated with increased neonatal morbidity and mortality. The less an infant weighs at birth, the greater the risks to life during delivery and immediately thereafter.
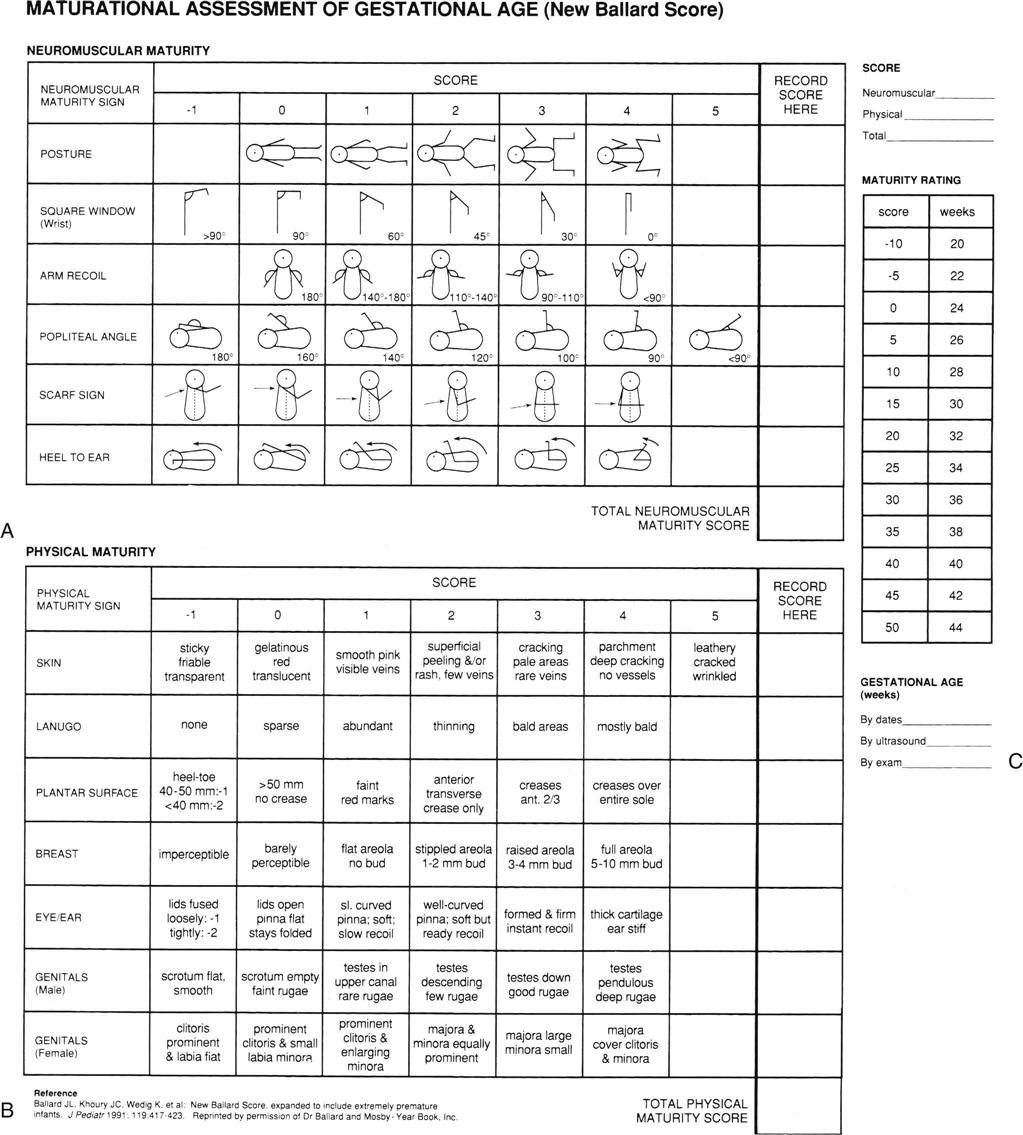
In the past a newborn was classified solely by birth weight. The emphasis is now on gestational age and level of maturation. Figure 13-1 shows two term infants of the same gestational age. One newborn would be classified as small-for-gestational-age (SGA), which may be the result of intrauterine growth restriction (IUGR) because of its weight and size. Term infants over 4000 g (8.8 lb) may be classified as large-for-gestational-age (LGA). Current data also indicate that intrauterine growth rates are not the same for all infants and that individual factors must be considered. Gestational age refers to the actual time, from conception to birth, that the fetus remains in the uterus. For the preterm infant this is less than 38 weeks, for the term infant it is 38 to 42 weeks, and for the postterm infant it is beyond 42 weeks. A late preterm infant, also known as a near-term infant, is born between 24 and 36 weeks and is also considered a high-risk newborn regardless of birth weight. One standardized method used to estimate gestational age is the Ballard scoring system, which is based on the infant’s external characteristics and neurological development (Figures 13-2 and 13-3).

Level of maturation refers to how well developed the infant is at birth and the ability of the organs to function outside the uterus. The physician can determine much about the maturity of the newborn by careful physical examination, observation of behavior, and family history. An infant who is born at 34 weeks of gestation, weighs 1588 g (3.5 lb) at birth, has not been damaged by multifactorial birth defects, and has had a good placenta may be healthier than a full-term, “small-for-date” infant whose placenta was insufficient for any of a number of reasons. Such an infant is also probably in better condition than the heavy but immature infant of a diabetic mother. Each infant has different and distinct needs.
Causes
The predisposing causes of preterm birth are numerous; in many instances the cause is unknown. Prematurity may be caused by multiple births, illness of the mother (e.g., malnutrition, heart disease, diabetes mellitus, or infectious conditions), or the hazards of pregnancy itself, such as gestational hypertension, placental abnormalities that may result in premature rupture of the membranes, placenta previa (in which the placenta lies over the cervix instead of higher in the uterus), and premature separation of the placenta. Studies also indicate the relationships between prematurity and poverty, smoking, alcohol consumption, and abuse of cocaine and other drugs.
Adequate prenatal care to prevent preterm birth is extremely important. Some preterm infants are born into families with numerous other problems. The parents may not be prepared to handle the additional financial and emotional strain imposed by a preterm infant. After delivery, early parental interaction with the infant is recognized as essential to the bonding (attachment) process. The presence of parents in special care nurseries is commonplace. Multidisciplinary care (including parent aides and other types of home support and assistance) is vital, particularly because current studies indicate a correlation between high-risk births and child abuse and neglect.
Physical Characteristics
Preterm birth deprives the newborn of the complete benefits of intrauterine life. The infant the nurse sees in the incubator may resemble a fetus of 7 months of gestation. The skin is transparent and loose. Superficial veins may be seen beneath the abdomen and scalp. There is a lack of subcutaneous fat, and fine hair (lanugo) covers the forehead, shoulders, and arms. The cheeselike vernix caseosa is abundant. The extremities appear short. The soles of the feet have few creases, and the abdomen protrudes. The nails are short. The genitalia are small. In girls the labia majora may be open (see Figure 13-3).
Related Problems
Inadequate Respiratory Function
Important structural changes occur in the fetal lungs during the second half of the pregnancy. The alveoli, or air sacs, enlarge, which brings them closer to the capillaries in the lungs. The failure of this phenomenon to occur leads to many deaths attributed to previability (pre, “before,” vita, “life,” and able “capable of”). In addition, the muscles that move the chest are not fully developed; the abdomen is distended, creating pressure on the diaphragm; the stimulation of the respiratory center in the brain is immature; and the gag and cough reflexes are weak because of immature nerve supply. Oxygen may be required and can be administered via nasal catheter, incubator, or oxygen hood (Figure 13-4). The oxygen must be warmed and humidified to prevent drying of the mucous membranes. Mechanical ventilation may be required. Oxygen saturation levels should be monitored. The infant is usually admitted to the NICU.
Respiratory Distress Syndrome.
Respiratory distress syndrome (RDS), also called hyaline membrane disease, is also known as respiratory distress syndrome type 1 (RDS type 2 is discussed in Chapter 14). RDS type 1 is a result of lung immaturity, which leads to decreased gas exchange. An estimated 30% of all neonatal deaths result from RDS or its complications (Kliegman et al., 2007). In this disease, there is a deficient synthesis or release of surfactant, a chemical in the lungs. Surfactant is high in lecithin, a fatty protein necessary for the absorption of oxygen by the lungs. Testing for the lecithin/sphingomyelin (L/S) ratio provides information about the amount of surfactant in amniotic fluid.
Manifestations.
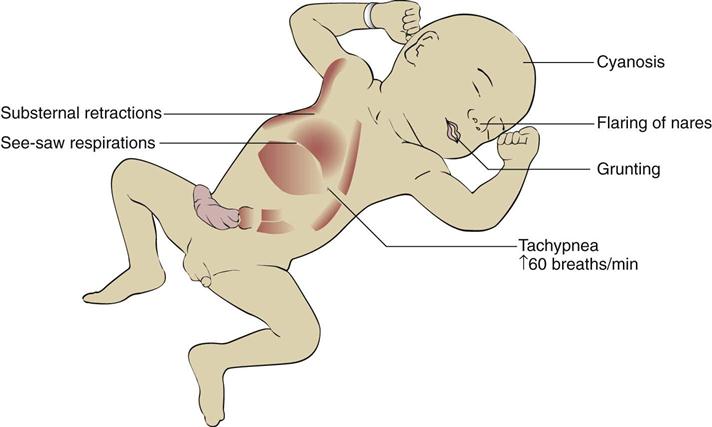
In general, the symptoms of respiratory distress are apparent after delivery, but they may not be manifested for several hours (Figure 13-5). Respirations increase to 60 breaths/min or more. Rapid respirations (tachypnea) are accompanied by gruntlike sounds, nasal flaring, cyanosis, and intercostal and sternal retractions. Edema, lassitude, and apnea occur as the condition becomes more severe. Mechanical ventilation may be necessary. The treatment of these infants is ideally carried out in the NICU.
Treatment.
Surfactant begins to appear in the fetal alveoli at approximately 24 weeks of gestation and is at a level to enable the infant to breathe adequately at birth by 34 weeks of gestation. If insufficient amounts of surfactant are detected through amniocentesis, it is possible to increase its production by giving the mother injections of corticosteroids such as betamethasone. Administration 1 or 2 days before delivery may reduce the chances of RDS. In preterm newborns, surfactant can be administered via endotracheal (ET) tube at birth or when symptoms of RDS occur, with improvement of lung function seen within 72 hours. Surfactant production is altered during episodes of cold stress or hypoxia and when there is poor tissue perfusion, and such conditions are often present in the preterm infant.
Vital signs are monitored closely, arterial blood gases are analyzed, and the infant is placed in a warm incubator with gentle and minimal handling to conserve energy. Intravenous fluids are prescribed, and the nurse observes for signs of overhydration or dehydration. Oxygen therapy may be given via hood (see Figure 13-4) or ventilator in concentrations necessary to maintain adequate tissue perfusion. Oxygen toxicity is a high risk for infants receiving prolonged treatment with high concentrations of oxygen. Bronchopulmonary dysplasia is the toxic response of the lung to oxygen therapy. Atelectasis, edema, and thickening of the membranes of the lung interfere with ventilation. This often results in prolonged dependence on supplemental oxygen and ventilators and has long-term complications.
Apnea.
Apnea is defined as the cessation of breathing for 20 seconds or longer. It is not uncommon in the preterm newborn and is believed to be related to immaturity of the nervous system. An apneic episode may be accompanied by bradycardia (heart rate of fewer than 100 beats/min) and cyanosis. Apnea monitors alert nurses to this complication. Gentle rubbing of the infant’s feet, ankles, and back may stimulate breathing after this occurrence. When these measures fail, suctioning of the nose and mouth and raising of the infant’s head to a semi-Fowler’s position usually facilitates breathing. If breathing does not begin, an Ambu bag is used.
Neonatal Hypoxia.
Neonatal hypoxia is inadequate oxygenation at the cellular level in a newborn infant. A deficiency of oxygen in the arterial blood is known as hypoxemia. The degree of hypoxemia present can be detected by a noninvasive pulse oximetry reading. Pulse oximetry is defined as the measure of oxygen on the hemoglobin in the circulating blood divided by the oxygen capacity of the hemoglobin. A pulse oximeter saturation level of 92% or above is normal (see Skill 13-1 on p. 312). There must be at least 5 g/dL of desaturated hemoglobin (unoxygenated blood) in order to produce clinical cyanosis. Therefore the severely anemic infant may have severe hypoxia yet not manifest clinical cyanosis. If the hemoglobin present is an abnormal fetal hemoglobin, hypoxia can be present even when the pulse oximeter shows a normal reading because fetal hemoglobin does not readily release oxygen to the tissues and end organs (Rohan & Golombek, 2009).
Sepsis.
Sepsis is a generalized infection of the bloodstream. Preterm newborns are at risk for developing this complication because of the immaturity of many body systems. The liver of the preterm infant is immature and forms antibodies poorly. Body enzymes are inefficient. There is little or no immunity received from the mother, and stores of nutrients, vitamins, and iron are insufficient. There may be no local signs of infection, which also hinders diagnosis. Some signs of sepsis include a low temperature, lethargy or irritability, poor feeding, and respiratory distress. Maternal infection and complications during labor can also predispose the preterm infant to sepsis.
Treatment involves administration of intravenous antimicrobials, maintenance of warmth and nutrition, and close monitoring of vital signs, including blood pressure. Keeping nursing care as organized as possible will help conserve energy. An incubator separates the infant from other infants in the unit and facilitates close observation. Maintenance of strict Standard Precautions is essential (see Appendix A).
Poor Control of Body Temperature
Keeping the preterm infant warm is a nursing challenge. Heat loss in the preterm infant results from the following factors:
• The preterm infant has a lack of brown fat, which is the body’s insulation.
• The heat-regulating center of the brain is immature.
• The sweat glands are not functioning to capacity.
• Metabolism is high, and the preterm infant is prone to low blood glucose levels (hypoglycemia).
These and other factors make the preterm newborn vulnerable to cold stress, which increases the need for oxygen and glucose. Early detection can prevent complications.
Nursing Care.
The infant’s skin temperature will fall before the core temperature falls. Therefore a skin probe is used to monitor the temperature of preterm infants. The skin probe is placed in the right upper quadrant of the abdomen. Care should be taken to ensure that the probe is not directly over a bony prominence, in the line of cool oxygen input, or under a diaper.
The infant is placed under a radiant warmer or in an incubator to maintain a warm environment. The temperature of the incubator is adjusted so that the infant’s body temperature is at an optimal level (36.2° to 37° C [97.1° to 98.6° F]).
Hypoglycemia and Hypocalcemia
Hypoglycemia (hypo, “less than,” and glycemia, “sugar in the blood”) is common among preterm infants. They have not remained in the uterus long enough to acquire sufficient stores of glycogen and fat. This condition is aggravated by the need for increased glycogen in the brain, the heart, and other tissues as a result of asphyxia, sepsis, RDS, unstable body temperature, and similar conditions. Any condition that increases energy requirements places more stress on these already deficient stores. Plasma glucose levels lower than 40 mg/dL indicate hypoglycemia in a term infant, and in a preterm infant, lower than 30 mg/dL.
The brain needs a steady supply of glucose, and hypoglycemia must be anticipated and treated promptly. Any condition that increases metabolism increases glucose needs. Preterm infants may be too weak to suck and swallow formula and often require gavage or parenteral feedings to supply their 120- to 150-kcal/kg/day needs.
Hypocalcemia (hypo, “below,” and calcemia, “calcium in the blood”) is also seen in preterm and sick newborns. Calcium is transported across the placenta throughout pregnancy, but in greater amounts during the third trimester. Early birth can result in infants with lower serum calcium levels.
In early hypocalcemia the parathyroid fails to respond to the preterm infant’s low calcium levels. Infants stressed by hypoxia or birth trauma or who are receiving sodium bicarbonate are at high risk for this problem. Infants born to mothers who are diabetic or who have had low vitamin D intake are also at risk for developing early hypocalcemia.
Late hypocalcemia usually occurs about age 1 week in newborn or preterm infants who are fed cow’s milk. Cow’s milk increases serum phosphate levels, which cause calcium levels to fall.
Hypocalcemia is treated by administering intravenous calcium gluconate. During intravenous therapy the nurse should monitor the infant for bradycardia. Adding calcium lactate powder to the formula also lowers phosphate levels. (Calcium lactate tablets are insoluble in milk and must not be used.) When calcium lactate powder is slowly discontinued from the formula, the nurse should again monitor the infant for signs of neonatal tetany.