Barbara Lauritsen Christensen
Care of the patient with a visual or auditory disorder
Objectives
1. List the major sense organs and discuss their anatomical position.
2. List the parts of the eye and define the function of each part.
3. List the three divisions of the ear and discuss the function of each.
4. Describe the physiologic processes involved in normal vision and hearing.
5. Describe two changes in the sensory system that occur as a result of the normal aging process.
13. Describe the various surgeries of the eye, including the nursing interventions and prognosis.
14. Differentiate between conductive and sensorineural hearing loss.
15. Describe the appropriate care of the hearing aid.
16. List tips for communicating with hearing- and sight-impaired people.
17. Identify communication resources for people with visual and/or hearing impairment.
22. Provide patient instructions regarding care of the eye and ear in accordance with written protocol.
Key terms
astigmatism ( -ST
-ST G-m
G-m -t
-t sm, p. 611)
sm, p. 611)
audiometry ( w-d
w-d –
– M-
M- -tr
-tr , p. 632)
, p. 632)
conjunctivitis (k n-j
n-j nk-t
nk-t -V
-V -t
-t s, p. 614)
s, p. 614)
cryotherapy (kr –
– -TH
-TH R-
R- -p
-p , p. 620)
, p. 620)
diabetic retinopathy (d –
– -B
-B T-
T- k r
k r -t
-t n-N
n-N P-
P- -th
-th , p. 618)
, p. 618)
enucleation ( -n
-n -kl
-kl –
– -sh
-sh n, p. 629)
n, p. 629)
exophthalmos ( k-s
k-s f-TH
f-TH L-m
L-m s, p. 607)
s, p. 607)
hyperopia (h -p
-p r-
r- -p
-p –
– , p. 611)
, p. 611)
keratitis (k r-
r- -T
-T -t
-t s, p. 615)
s, p. 615)
keratoplasty (k r-
r- -t
-t -PL
-PL S-t
S-t , p. 629)
, p. 629)
labyrinthitis (l b-
b- -r
-r nth-
nth- -t
-t s, p. 639)
s, p. 639)
mastoiditis (m s-t
s-t y-D
y-D -t
-t s, p. 636)
s, p. 636)
mydriatic (m d-r
d-r –
– T-
T- k, p. 608)
k, p. 608)
myringotomy (m r-
r- n-G
n-G T-
T- -m
-m , p. 645)
, p. 645)
radial keratotomy (R -d
-d –
– l k
l k -r
-r -T
-T T-
T- -m
-m , p. 612)
, p. 612)
retinal detachment (R -t
-t -n
-n l d
l d -T
-T CH-m
CH-m nt, p. 622)
nt, p. 622)
Sjögren syndrome (SH R-gr
R-gr nz S
nz S N-dr
N-dr m, p. 615)
m, p. 615)
Snellen’s test (SN L-
L- nz t
nz t st, p. 608)
st, p. 608)
stapedectomy (st -p
-p -D
-D K-t
K-t -m
-m , p. 644)
, p. 644)
strabismus (str -B
-B Z-m
Z-m s, p. 611)
s, p. 611)
tympanoplasty (t m-p
m-p -n
-n -PL
-PL S-t
S-t , p. 644)
, p. 644)
Anatomy and physiology of the sensory system
The sensory system constantly gathers information through millions of receptors scattered throughout the body and delivers it to the brain for interpretation. This process enables humans to survive safely by enabling them to make appropriate responses to external stimuli. The five major senses are taste, touch, smell, sight, and hearing. The sense of balance (equilibrium) is linked with hearing, since the sensors are located within the ear.
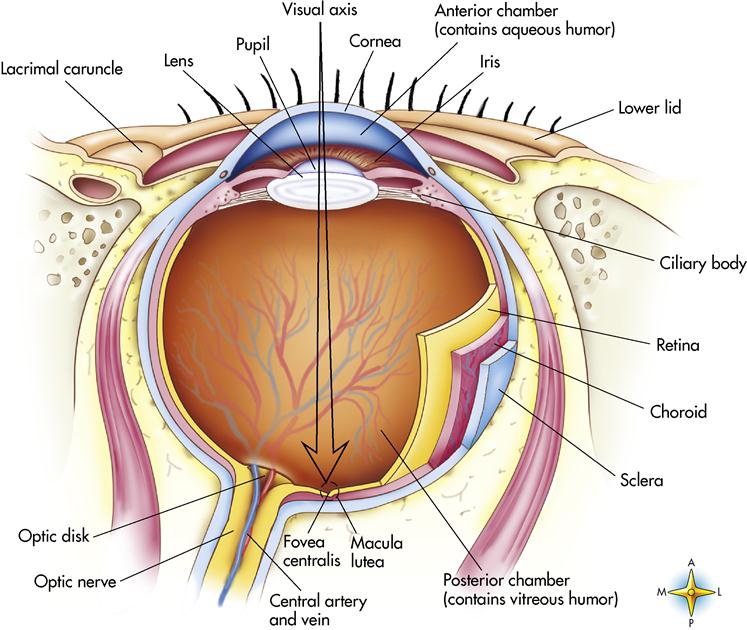
Anatomy of the eye
The eye, which is only 1 inch (2.5 cm) in diameter, is a marvelous spherical structure that contains 70% of the sensory structures of the body. The optic tracts contain more than 1 million nerve fibers that carry messages from the eye to the brain, where they are interpreted. Only a small portion of the eye is visible externally; the remainder is enclosed in the skeletal bones of the face and cushioned in layers of fat. The bones surrounding the eyeball include the frontal, zygomatic, ethmoid, sphenoid, and lacrimal bones.
Accessory structures of the eye
The accessory structures of the eye—eyebrows, eyelashes, eyelids, and lacrimal apparatus—function mainly as protective devices. In addition, six extrinsic eye muscles control gross eye movement and enable the eye to focus on any object in the visual field. The eye muscles are attached to the sclera (or white part of the eye) and move the eye laterally, medially, superiorly, and inferiorly.
The lacrimal apparatus (Figure 13-1) manufactures and drains tears to keep the eyeball moist and sweep away debris that might enter the eye. Tears are composed of a watery secretion that contains salt, mucus, and a bactericidal enzyme called lysozyme. The lacrimal glands are located superior and lateral to each eye. Blinking causes tears to flow medially to the lacrimal ducts, which empty into the nasolacrimal ducts and drain into the nasal cavity.
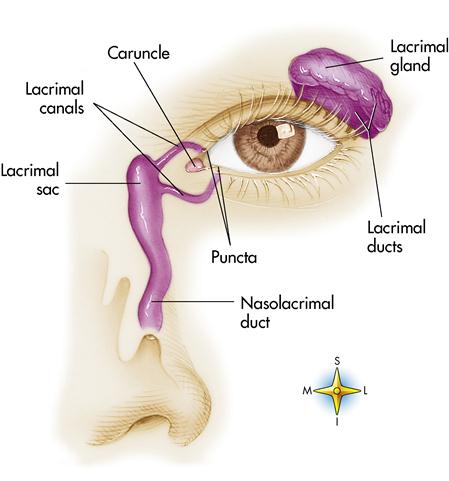
The conjunctiva is a thin mucous membrane that lines the inner aspect of the eyelids and the anterior surface of the eyeball to the edge of the cornea. Sometimes the blood vessels of the conjunctiva become dilated because of irritation or congestion, and the individual is said to have “bloodshot” eyes. The lower conjunctival sac is where eyedrops and eye ointment medication are usually administered.
Structure of the eyeball
The eyeball is composed of three layers, or tunics (Figure 13-2). The outermost layer of the eyeball is the fibrous tunic; it is composed of the sclera and the cornea. The sclera, or white of the eye, is a thick, white, opaque, connective tissue. The sclera gives shape to the eyeball and, because of its toughness, protects the inner eye structures. Posteriorly it is pierced by the optic nerve.
The cornea is the central anterior portion of the sclera. It is transparent and covers the iris, which is the colored portion of the eye. The cornea allows light rays to enter the inner portion of the eye. The cornea is the first part of the eye that refracts (bends) light rays. It is dense, uniform in thickness, and nonvascular, and it projects like a dome beyond the sclera. The cornea is one of the most highly developed, sensitive tissues in the body and is innervated by the trigeminal nerve (cranial nerve V). The avascular cornea obtains oxygen primarily through absorption from the tear film layer that bathes the epithelium. A small amount of oxygen is obtained from the aqueous humor (watery fluid in front of the lens in the anterior chamber of the eye) through the endothelial layers. The degree of corneal curvature varies in different individuals and in the same person at different ages. The curvature is more pronounced in youth than in advanced age.
At the junction of the sclera and cornea is a special structure called the canal of Schlemm. This tiny venous sinus at the angle of the anterior chamber of the eye drains the aqueous humor and funnels it into the bloodstream. This aids in controlling intraocular pressure (IOP; the pressure within the eyeball).
The middle layer of the eyeball is the vascular tunic. It contains the choroid, the ciliary body, and the iris. The posterior portion of the vascular tunic is the choroid, which is a thin, dark brown membrane that lines most of the internal area of the sclera. It is highly vascular and supplies nutrients to the retina. The anterior portion of the vascular tunic forms the ciliary body, which is an intrinsic muscular ring that holds the lens in place and changes its shape for near or distant vision. The ciliary body also attaches to the iris, a pigmented intrinsic muscular ring that resembles a doughnut. Located slightly nasal to the center of the iris is a circular opening called the pupil. The iris lies between the cornea and the lens and regulates the amount of light entering the eye through the pupil, much like a camera shutter. Two sets of smooth muscle control the iris, which in turn controls the pupil. In bright light the circular muscle fibers of the iris contract and the pupil contracts; in dim light the radial muscles contract and the pupil dilates. Papillary constriction is a reflex that protects the retina from intense light or that permits more acute near vision.
The innermost tunic of the eye is the retina, a 10-layer, delicate, nervous-tissue membrane that receives images of external objects and transmits impulses through the optic nerve to the brain. It lies on the posterior portion of the eyeball. The retina contains specialized sensory cells called rods and cones (photoreceptors). The rods and cones are scattered throughout the retina except where the optic nerve exits the eye; this area is called the optic disk or blind spot. Rods are receptors for night vision and are also responsible for peripheral vision. Cones are responsible for day vision. The three kinds of cones are each sensitive to a different color: red, green, or blue. Color pigments that are sensitive to light enable the rods and cones to function. Rods detect only the presence of light, whereas cones detect different wave lengths of color.
The center of the retina is the fovea centralis, a pinpoint depression composed only of densely packed cones. The fovea centralis contains the greatest concentration of cones of any area in the retina. This area of the retina provides the sharpest visual acuity and most acute color vision. Surrounding the fovea is the macula, an area of less than 1 mm2 that has a high concentration of cones and is relatively free of blood vessels. Vitamin A is responsible for the production of these color pigments. The absence of these three types of cones causes color blindness, which is an inherited condition found primarily in males.
Chambers of the eye
The eye is divided into the anterior and posterior chambers by the crystalline lens, a transparent, colorless structure that is biconvex, enclosed in a capsule, and held in place just behind the pupil by the suspensory ligament. The crystalline lens focuses light rays so that they form a perfect image on the retina. Anterior to the crystalline lens is the anterior chamber, which is filled with aqueous humor, a clear, watery fluid similar to blood plasma. The ciliary bodies of the choroid constantly secrete, drain, and replace aqueous humor to maintain normal IOP. Aqueous humor also helps maintain the eyeball’s shape, keeps the retina attached to the choroid, and refracts light.
The posterior chamber is filled with vitreous humor, a transparent, jellylike substance that gives shape to the eyeball, keeps the retina attached to the choroid, and refracts light. It differs from the aqueous humor in that it is not continuously replaced.
Physiology of vision
Light must travel through the cornea, the aqueous humor, the pupil, the crystalline lens, and the vitreous humor and finally reaches the rods and cones of the retina. The image is transported via the optic nerve to the visual center of the cerebral cortex in the brain.
Four basic processes are necessary to form an image:
Anatomy and physiology of the ear
The external ear (pinna, or auricle) reveals only a portion of the complex organ of hearing. Within the ear are many structures that enable hearing and interpretation of sound and assist in maintaining equilibrium (balance). Anatomically, from the external structures to the internal structures, the ear has three distinct divisions: the external ear, the middle ear, and the inner ear (Figure 13-3). The external ear and the middle ear deal exclusively with sound waves, whereas the inner ear deals with sound waves and equilibrium.
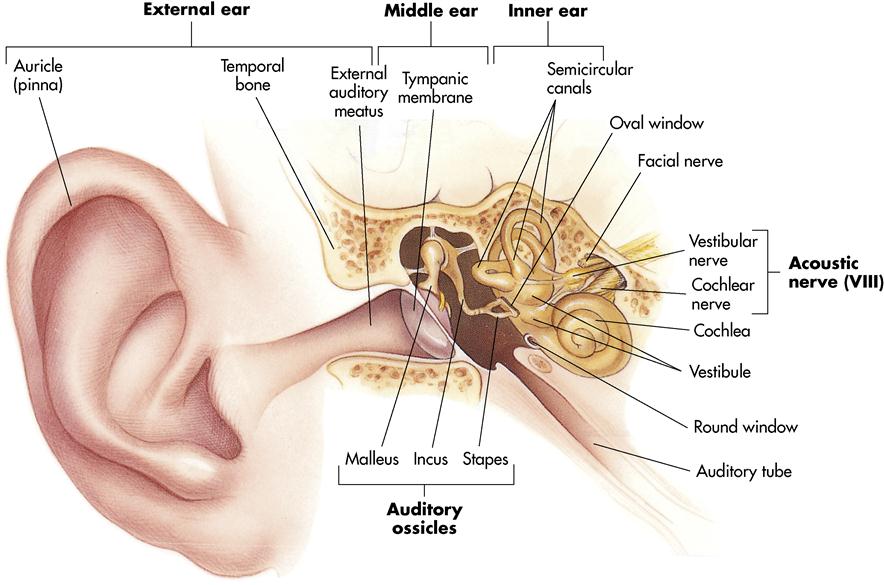
External ear
The external ear is composed of the auricle (pinna) and the external auditory canal. The canal is shaped like a small, curved tube (about 1 inch [2.5 cm] in length). It extends into the temporal bone, ending at the tympanic membrane—a thin, semitransparent membrane. The tympanic membrane separates the external ear from the middle ear and transmits sound vibrations to the internal ear by means of the auditory ossicles. The external ear is designed to collect sound waves and channel them to the middle ear. The upper part of the pinna is composed of elastic cartilage, whereas the lower part, the lobe, is mainly fleshy tissue. The whole structure is attached to the head by ligaments and muscles.
The walls of the external auditory canal are composed of cartilage-lined bone. The external auditory canal contains cilia (tiny hairs) and specialized sebaceous (oil) glands called ceruminous glands. They secrete cerumen (earwax), which protects the lining from infection. The cilia, in combination with the cerumen, also prevent foreign objects from entering the ear.
Middle ear
The middle ear, or tympanic cavity, is a small, air-filled chamber located within the temporal bone. The eustachian tube, or auditory canal, is lined with a mucous membrane that joins the nasopharynx and the middle-ear cavity. During swallowing or yawning, the tube allows air to enter the middle ear, which equalizes the air pressure on either side of the tympanic membrane. Because the pharynx, the eustachian tube, and the middle ear are all covered with a continuous mucous membrane, infection can travel easily from the throat to the middle ear. This is often seen in young children. The posterior wall of the middle ear opens into the mastoid process, an area filled with air spaces, which also aids in equalizing air pressure. Infection of the middle ear, if untreated, can spread to the mastoid process.
Extending along the middle-ear chamber are three small bones (ossicles) that carry sound waves from the external ear to the inner ear. These ossicles are named according to their shape: the malleus (hammer), the incus (anvil), and the stapes (stirrup). The internal surface of the tympanic membrane is connected to the first of these three bones, the malleus. The malleus transfers sound waves to the incus, which in turn transfers them to the stapes. The stapes pushes against the oval window, a small membrane that marks the beginning of the inner ear. When sound waves cause the tympanic membrane to vibrate, that vibration is transmitted and amplified by the ear ossicles as it passes through the middle ear. Movement of the stapes against the oval window causes movement of fluid in the inner ear.
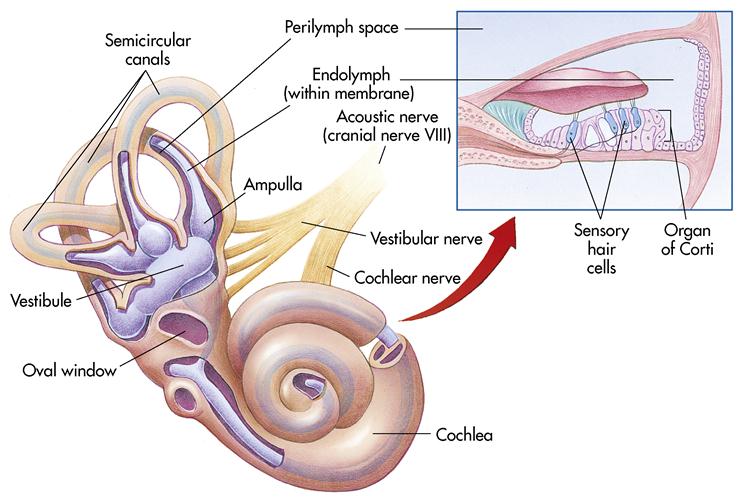
Inner ear
A very important portion of the ear, the inner ear, or labyrinth, is a series of canals (Figure 13-4). Structurally, it contains the bony labyrinth, which is filled with a fluid called perilymph. The bony labyrinth has three subdivisions called the semicircular canal (associated with the sense of balance), the vestibule, and the cochlea. The membranous labyrinth is a series of sacs and tubes that contain a thicker fluid called endolymph. Endolymph and perilymph conduct sound waves through the inner-ear system.
The cochlea resembles a snail’s shell and contains the organ of Corti, the organ of hearing. It contains many hearing receptors, or hair cells. These cells respond to sound waves by stimulating the cochlear nerve (a branch of the eighth cranial nerve—the vestibulocochlear, or acoustic, nerve), which transmits the message to the brain. These hair cells may become damaged from noise pollution (i.e., high-intensity sounds such as those produced by jet engines, factory equipment, and rock bands). Once these cells are damaged or destroyed, hearing becomes permanently impaired.
Deeper in the inner ear, past the cochlea, is the vestibule, or the oval central portion of the bony labyrinth. The vestibule contains receptors that respond to gravity. They provide information on which way is up and which way is down, enabling an individual to remain in an upright position. Extending upward from the vestibule are three semicircular canals responsible for maintaining balance and equilibrium. They contain sensory hair cells and endolymph. The motion of the endolymph stimulates the hair cells, which stimulate the receptors; then the message is sent to the brain for interpretation (see Figure 13-4).
Other special senses
Taste and smell
The tongue of the average adult contains approximately 10,000 taste buds; some are also located on the inner aspect of the cheeks. Certain locations on the taste buds are receptors for four taste sensations, as follow:
1. Sweet: Respond to sugar and other sweet substances; located on the tip of the tongue
2. Sour: Respond to acid content of foods; located on the sides of the tongue
3. Salty: Respond to metal ions within foods; located on the tip of the tongue
The receptors for the sense of smell (olfactory receptors) are located in the roof, or the upper part of the nasal cavity. On inhalation, an odor comes in contact with the olfactory receptors and the message is sent to the brain. Certain odors are remembered for a long time and stimulate certain memories (e.g., pine scent reminds people of Christmas; talcum powder reminds people of infants). The body is not able to regenerate olfactory cells; once they are damaged, the sense of smell is impaired.
Touch
The receptors for touch (tactile receptors) are located throughout the integumentary system. They respond to touch, pressure, and vibration.
Position and movement
Proprioception (sense of position) maintains the proper position of the body. Proprioceptors include any sensory nerve ending—such as those located in muscles, tendons, and joints—that responds to stimuli originating from within the body regarding movement and spatial position. They work in conjunction with the semicircular canals and the vestibule of the inner ear to maintain proper coordination. They orchestrate the body’s movements in running, walking, dancing, and many other activities. Once they receive information from the environment, they send it to the cerebellum for interpretation. Proprioceptors enable one to sense the position of the different parts of the body and be aware of the movement of each.
Normal aging of the sensory system
As the individual ages, the crystalline lens of the eye hardens and becomes too large for the eye muscles, thus causing a loss of accommodation. This often results in a need for bifocals or trifocals. The crystalline lens loses some of its transparency and becomes more opaque, and glare begins to become a problem. The lens proteins are vulnerable to biochemical changes and exposure to ultraviolet (UV) light, resulting in cataract development. Hypertension and atherosclerosis lead to retinal vascular changes. Age-related macular degeneration (ARMD) contributes to impaired vision. The pupils become smaller and decrease the amount of light that reaches the retina, resulting in a need for brighter lighting for reading (Lewis et al., 2007).
Impaired hearing can result from age-related changes in the auditory system. A condition called presbycusis, a hearing deficit secondary to aging, can occur from numerous sources such as noise, vascular or systemic diseases, poor nutrition, ototoxic drugs, and pollution. These exposures occurring over the life span can damage the delicate hair cells of the organ of Corti, cause calcification of the ossicles of the middle ear, and interfere with sound conduction. Tinnitus (ringing in the ear) may also occur secondary to the aging process.
Visual and hearing losses in the older adult can result in physical and psychosocial problems. Early detection of these helps maintain a more productive lifestyle (Lewis et al., 2007). The remaining senses undergo slight changes that decrease their reaction or threshold time, which results in slower response or diminished sensation (see Life Span Considerations box).
Nursing considerations for care of the patient with an eye disorder
In caring for the patient with an eye disorder, review the following items:
• Nystagmus (involuntary, rhythmic movements of the eyes)
• Current medication for the eye disorder
• Side effects of any medications
• Use of glasses or contact lenses
• Adequacy of current eyewear prescription
• Personal habits related to care of eyewear
After gathering the information and reporting it to the physician, assist with the eye examination. The results of the initial examination are compared with normal findings (Table 13-1).
Table 13-1
Normal Findings of the Adult Eye
| AREA EXAMINED | FINDINGS |
| Eyelid | Blink reflex to light or touch intact. Lid margins just above the corneal borders. |
| Eyeball | Eyeball does not protrude beyond the supraorbital ridge of the frontal bone. The eyeball is usually moist; moisture may be diminished in the older adult. |
| Conjunctiva | |
| Sclera | Generally white; may have yellow-tan dots in a dark-skinned individual. |
| Cornea | Transparent, smooth, convex. In the older adult, a gray ring around the cornea (arcus senilis) may be present as a result of lipid deposits. |
| Iris | Round, intact, bilateral coloration. In the older adult, color may be paler and shape less regular. |
| Pupil | Equal, round, reactive to light and accommodation. Response to light is equal bilaterally. In the older adult, constriction response may be slower. |
| Internal eye (including retina, vessels, and optic disk) | Retina is intact. Vessel structure is intact and bilaterally similar in pattern. Optic disk has well-defined border. |
| Visual acuity | |
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| |
 T-
T- -r
-r kt,
kt,  w-K
w-K -m
-m ,
,  –
– T-
T- ks,
ks,  –
– -p
-p –
– ,
,  -n
-n -t
-t s,
s,  R-t
R-t -g
-g ,
,