The Nurse’s Role in Women’s Health Care
Objectives
1. Define each key term listed.
2. Explain aspects of preventive health care for women.
3. Describe each menstrual disorder and its care.
4. Explain each gynecological infection in terms of cause, transmission, treatment, and care.
5. Describe the various methods of birth control, including side effects and contraindications of each.
6. Describe how to use natural family planning methods for contraception or infertility management.
7. Describe possible causes and treatment of infertility.
8. Explain the changes that occur during the perimenopausal period and after menopause.
9. Explain the medical and nursing care of women who are nearing or have completed menopause.
11. Describe the nursing care and treatment of a woman with leiomyoma.
Key Terms
amenorrhea (ă-mĕn-ŏ-RĒ-ă, p. 251)
climacteric (klī-MĂK-ŭr-ĭk, p. 272)
coitus interruptus (KŌ-ĭ-tŭs ĭn-tŭr-RŬP-tŭs, p. 266)
dysmenorrhea (dĭs-mĕn-ō-RĒ-ă, p. 251)
dyspareunia (dĭs-pă-RŪ-nē-ă, p. 252)
endometriosis (ĕn-dō-mē-trē-Ō-sĭs, p. 252)
leiomyomas (lī-ō-mī-Ō-măz, p. 276)
menopause (MĔN-ō-păwz, p. 272)
menorrhagia (mĕn-ō-RĀ-zhă, p. 251)
metrorrhagia (mĕ-trō-RĀ-zhă, p. 251)
mittelschmerz (MĬT-ĕl-shmārts, p. 251)
myomas (mī-Ō-măz, p. 269)
osteoporosis (ŏs-tē-ō-pă-RŌ-sĭs, p. 272)
retrograde ejaculation (p. 268)
spermicides (p. 262)
spinnbarkeit (SPĬN-băhr-kīt, p. 259)
stress incontinence (p. 276)
![]() http://evolve.elsevier.com/Leifer
http://evolve.elsevier.com/Leifer
Today women from all ethnic backgrounds choose to be active participants in their health care and therefore need information about their bodies, health promotion, self-care techniques, and choices concerning treatment options. Culturally competent communication is the key to empowering the woman to feel confident about her ability to care for herself and her family. In some cultures, women ask when they want to know; in other cultures, women wait to be told what to do. To be an effective teacher about health behaviors, the nurse must understand the cultural needs, past experiences, and individual goals of the patient. The nurse offers support, knowledge, and caring behaviors that help the woman cope with screening tests or problems.
Goals of Healthy People 2020
Some Healthy People 2020 (U.S. Department of Health and Human Services [USDHHS), 2010) goals and strategies related to women’s health include the following:
Achievement of these goals requires preventive care, screening, and increased accessibility to health care.
Preventive Health Care for Women
The goal of preventive health care, or health maintenance, is the prevention or early identification of disease. The value of preventive health care is that some disabling conditions can be prevented or their severity lessened by specific measures, such as altering the diet or detecting the disorder early and at a more treatable stage. Preventive care for women may include disorders with these characteristics:
• Exclusive to women, such as cervical cancer
• Dominant in women, such as breast cancer or osteoporosis
• Prevalent in the general population, such as hypertension or colorectal cancers
This chapter will focus on those disorders that are exclusive to or dominant in women. Much of preventive health care involves screening tests. These tests are not diagnostic but can identify whether additional testing is needed. Examples of screening tests that are common in women’s health care include mammography to identify breast cancer and Pap tests for cervical cancer.
Breast Care
Three approaches are needed for early detection of breast cancer:
The nurse’s role is to educate women about the benefit of all three examinations and techniques of self-examination. The reader should consult a medical-surgical text for additional information about the diagnosis and treatment of breast cancer.
Breast Self-Examination
Breast self-examination (BSE) should be performed by all women after age 20 years at about the same time each month. The best time for BSE is 1 week after the beginning of the menstrual period. If she is not menstruating, the woman may choose any day that is easy for her to remember, such as the first day of each month. Skill 11-1 describes how to teach a woman to perform BSE.
The chief value of BSE is that a woman learns how her own breasts feel. This is particularly valuable if she has fibrocystic breast changes, in which there are often many lumps that may change with hormonal fluctuations. The woman who knows her own breasts is more likely to notice when something is different about them.
Professional Breast Examination
BSE is a supplement to, rather than a substitute for, regular professional examinations. Although the woman who does regular BSE knows what is usual for her own breasts, professionals have the training and experience to identify suspicious breast masses. It is part of every annual gynecological examination and is done more frequently for women who have a high risk for breast cancer. It is recommended at yearly intervals for all women over age 20 years. The professional examination is similar to that for BSE.
Mammography
Mammography uses very-low-dose x-rays to visualize the breast tissue. It can detect breast tumors very early—long before the woman or a professional can feel them. The breast is compressed firmly between two plates, which is briefly uncomfortable. Scheduling the mammogram after a menstrual period reduces the discomfort because the breasts are less tender at that time. The American Cancer Society (2007) currently recommends a mammogram every 1 to 2 years for all women age 40 years or over. Women at higher risk for breast cancer may begin mammography earlier.
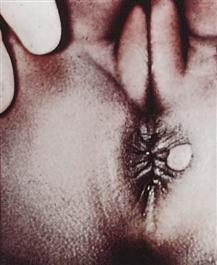
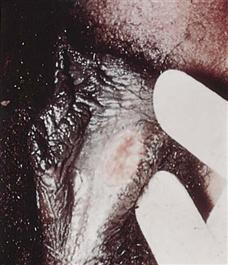
Vulvar Self-Examination
Women over 18 years of age (or younger, if sexually active) should perform a monthly examination of the external genitalia to identify lesions or masses that may indicate infection or malignancy. The woman should use a hand mirror in a good light to systematically inspect and palpate her vulva and mons pubis for any new growths of any type, any painful or inflamed areas, ulcers, sores, or changes in skin color. She should report any abnormalities to her health care provider.
Pelvic Examination
The pelvic examination should be scheduled between menstrual periods, and the woman should not douche or have sexual intercourse for at least 48 hours before the examination to avoid altering the Pap test. The purpose of the pelvic examination is to identify conditions such as tumors, abnormal discharge, infections, or unusual pain.
The health care provider first checks the external genitalia to identify signs or problems similar to those noted in vulvar self-examination. Next, a speculum is inserted to visualize the woman’s cervix and vagina for inflammation, discharge, or lesions. The speculum is warmed and lubricated with warm water only. A Pap test is obtained to screen for changes in the vaginal and cervical tissues that may be precancerous. The current American Cancer Society recommendations (2009) for the Pap test are as follows:
After the Pap test is obtained, the health care provider will perform an internal, or bimanual, examination to evaluate the internal organs. The index and middle fingers of one hand are inserted into the vagina and the other hand is placed on the abdomen to permit palpation of the cervix, uterus, and ovaries between the fingers. After the internal examination, a single lubricated finger is inserted into the rectum to identify hemorrhoids or other lesions. A test for fecal occult blood may be done at this time (see a medical-surgical text for details).
Menstrual Disorders
Menstrual cycle disorders can cause many women distress. The nursing role in each depends on the disorder’s cause and treatment. Common nursing roles involve explaining any recommended treatments (e.g., medications) and caring for the woman before and after procedures. The nurse also provides emotional support to the patient.
Amenorrhea
Amenorrhea is the absence of menstruation. It is normal before menarche, during pregnancy, and after menopause. Amenorrhea that is not normal may fall into one of two categories:
Treatment of amenorrhea begins with a thorough history, physical examination, and laboratory examinations to identify the cause. Pregnancy testing is done for any sexually active woman.
The specific treatment depends on the cause that is identified. For example, women who are very thin or have a low percentage of body fat may have amenorrhea because fat is necessary for estrogen production. This group of women may include athletes but may also include patients who have eating disorders such as anorexia or bulimia. Therapy for their eating disorder may result in the resumption of normal periods. Other treatments are aimed at correcting the cause, which may be an endocrine imbalance.
Abnormal Uterine Bleeding
Abnormal uterine bleeding is (1) too frequent, (2) too long in duration, or (3) excessive in amount. Metrorrhagia is uterine bleeding that is usually normal in amount but occurs at irregular intervals. Menorrhagia refers to menstrual bleeding that is excessive in amount. The average woman loses about 35 mL of blood during normal menstruation. Blood loss greater than 80 mL/month is considered excessive and often results in anemia. Common causes for any type of abnormal bleeding include the following:
• Pregnancy complications, such as an unidentified pregnancy that is ending in spontaneous abortion
• Lesions of the vagina, cervix, or uterus (benign or malignant)
• Breakthrough bleeding (BTB) that may occur in the woman taking oral contraceptives
• Endocrine disorders such as hypothyroidism
Treatment of abnormal uterine bleeding depends on the identified cause. Pregnancy complications and benign or malignant lesions are treated appropriately. BTB may be relieved by a change in the oral contraceptive used. Abnormal hormone secretion is treated with the appropriate medications. Surgical dilation and evacuation (D&E [formerly known as dilation and curettage, or D&C]) may serve to remove intrauterine growths or aid in diagnosis. Hysterectomy may be done for some disorders if the woman does not want other children. A newer technique, laser ablation, can permanently remove the abnormally bleeding uterine lining without a hysterectomy. Menorrhagia can be treated with mefenamic acid (a nonsteroidal antiinflammatory drug, or NSAID) or tranexamic acid (an antifibrinolytic) if hormone therapy is contraindicated.
Menstrual Cycle Pain
Mittelschmerz
Mittelschmerz (“middle pain”) is pain that many women experience around ovulation, near the middle of their menstrual cycle. Mild analgesics are usually sufficient to relieve this discomfort. The nurse can teach the woman that this discomfort, although annoying, is harmless.
Dysmenorrhea
Dysmenorrhea, painful menses or “cramps,” affects many women. It occurs soon after the onset of menses and is spasmodic in nature. Discomfort is in the lower abdomen and may radiate to the lower back or down the legs. Some women also have diarrhea, nausea, and vomiting. It is most common in young women who have not been pregnant (nulliparas).
There are two types of dysmenorrhea: primary, in which there is no evidence of pelvic abnormality, and secondary, in which a pathological condition is identifiable. Primary dysmenorrhea is a leading cause of short-term recurrent school absenteeism in adolescent girls in the United States. Characteristics include the following:
• Onset is shortly after menarche with heavy menstrual flow.
• Pain starts no more than a few hours before menstruation starts and lasts no more than 72 hours.
• Pelvic examination results are normal.
Vasopressins and prostaglandins from the endometrium (uterine lining) play an important role in dysmenorrhea. Some women produce excessive amounts of prostaglandins from the endometrium, and these substances are potent stimulants of painful uterine contractions. Three treatments may provide relief:
Low-fat and vegetarian diets reduce serum estrogen levels and can relieve menstrual pain in some women. Vitamins B and E, and the high level of omega-3 fatty acids in vegetarian diets influence prostaglandin metabolism and may have effects similar to antiinflammatory agents (French, 2005).
Endometriosis
Endometriosis is the presence of tissue that resembles endometrium outside the uterus. This tissue responds to hormonal stimulation just as the uterine lining does. The lesions may cause pain, pressure, and inflammation to adjacent organs as they build up and slough during menstrual cycles.
Endometriosis causes pain in many women that is either sharp or dull. It is more constant than the spasmodic pain of dysmenorrhea. Dyspareunia (painful sexual intercourse) may be present. Endometriosis appears to cause infertility in some women.
Treatment of endometriosis may be either medical or surgical. Medications such as danazol and agonists of gonadotropin-releasing hormone (GnRH) may be given via nasal spray to reduce the buildup of tissue by inducing an artificial menopause. The woman may have hot flashes and vaginal dryness, similar to symptoms occurring at natural menopause. She is also at increased risk for other problems that occur after menopause, such as osteoporosis and serum lipid changes. Surgical treatment includes the following:
Premenstrual Dysphoric Disorder
Formerly called premenstrual syndrome (PMS), premenstrual dysphoric disorder (PMDD) is associated with abnormal serotonin response to normal changes in the estrogen levels during the menstrual cycle. The following symptom criteria (which are used to diagnose PMDD) occur between ovulation and the onset of menstruation, begin to improve between the menstruation and ovulation phase, and are not present in the week after the menstrual period. Five or more of the following symptoms usually occur regularly:
• Anxiety, tension, feeling “on edge”
• Increased sensitivity to rejection
• Decreased interest in usual activities
• Lethargy
• Change in appetite—food cravings
• Physical symptoms such as breast tenderness, bloating, weight gain, headaches
Treatment includes prescribing calcium, magnesium, and vitamin B6 (helps convert tryptophan to serotonin) and a diet rich in complex carbohydrates and fiber (to lengthen effects of the carbohydrate meal). Stress management and exercise are also advised. Medical management includes oral contraceptives (low-estrogen, progestin-dominant), diuretics during the luteal phase of the menstrual cycle (between ovulation and onset of menstruation), and NSAIDs to prevent headaches.
Serotonin reuptake inhibitors such as fluoxetine (Sarafem) may also be prescribed for negative behavior. Medroxyprogesterone (Depo-Provera) may be indicated to inhibit ovulation and thus control estrogen levels. Patient education concerning maintenance of a monthly calendar of symptoms, stress management, and dietary guidance are important nursing responsibilities. Although eating chocolate has been shown to elevate depressed moods, excessive consumption should be avoided.
The Normal Vagina
At birth the infant’s vaginal epithelium is controlled by estrogen from the mother and is rich in glycogen, with a low pH of 3.7 to 6.3. When the maternal estrogen effect decreases, the vaginal epithelium atrophies and contains little glycogen. The pH rises to 7. Estrogen influence returns at puberty, and glycogen increases. The interaction of glycogen and estrogen in the vaginal epithelium results in the growth of lactobacilli, which have bacteriostatic action. The pH falls to 3.5 to 4.5. The types of bacteria found in the vagina vary with the pH of the vagina. Factors that change the normal flora of the vagina and predispose to vaginal infection include the following:
• Antibiotics: Encourage yeast overgrowth
• Sexual intercourse: Raises pH to 7 or higher for 8 hours after coitus
• Uncontrolled diabetes mellitus: Increases glucose that promotes organism growth
The normally acidic pH for the vagina is the first line of defense against vaginal infections. Normal vaginal secretions are made up of creamy white epithelial cells and mucus from the cervix, Skene’s glands, and Bartholin’s glands. The secretions prevent dryness and infection. Immediately after menstruation the mucus is thin, but as ovulation approaches, the estrogen level increases; at ovulation, the mucus is clear and slippery and can be stretched without breaking (spinnbarkeit) (see Figure 11-2). After ovulation the mucus is cloudy and sticky. At menopause, lowered estrogen causes vaginal dryness and the pH may change, predisposing the woman to vaginal discomfort and infections. Other factors can alter the pH of the vagina temporarily and include the following:
Gynecological Infections
Vaginal infections are the most common reason for women to seek health care. Nurses play a key role in educating women concerning vaginal health and the prevention of sexually transmitted infections. Identifying high-risk behavior and providing nonjudgmental, sensitive counseling and education should be part of every physical checkup. Safe sex practices, the reduction of the number of partners, and avoiding the exchange of body fluids are part of primary prevention of STIs. Community-based education in schools and churches is also important in primary prevention.
There are three classes of gynecological infections:
Toxic Shock Syndrome
Toxic shock syndrome (TSS) is a rare and potentially fatal disorder. It is caused by strains of Staphylococcus aureus that produce toxins that can cause shock, coagulation defects, and tissue damage if they enter the bloodstream. TSS is associated with the trapping of bacteria within the reproductive tract for a prolonged time. Factors that increase the risk of TSS include the use of high-absorbency tampons and the use of a diaphragm or cervical cap for contraception. Signs and symptoms of TSS include the following:
• Generalized rash that resembles sunburn
• Skin peeling from the palms and soles 1 to 2 weeks after the illness
The incidence of TSS has decreased, but nurses continue to play a role in prevention. The nurse’s role is primarily one of education. The following teaching points should be included:
• Wash hands before and after inserting a tampon.
• Change tampons at least every 4 hours.
• Do not use superabsorbent tampons.
Diaphragm or cervical cap use:
• Wash hands before and after inserting the diaphragm or cervical cap.
• Do not use a diaphragm or cervical cap during the menstrual period.
• Remove the diaphragm or cervical cap at the time recommended by the health care provider.
Sexually Transmitted Infections
STIs are those that can be spread by sexual contact, although several of these have other modes of transmission as well. It is important that all sexual contacts, even those who are asymptomatic, be completely treated to eradicate the infection. Table 11-1 gives specific information about STIs that the nurse may encounter. Certain STIs must be reported to the health department.
Table 11-1
Sexually Transmitted Infections
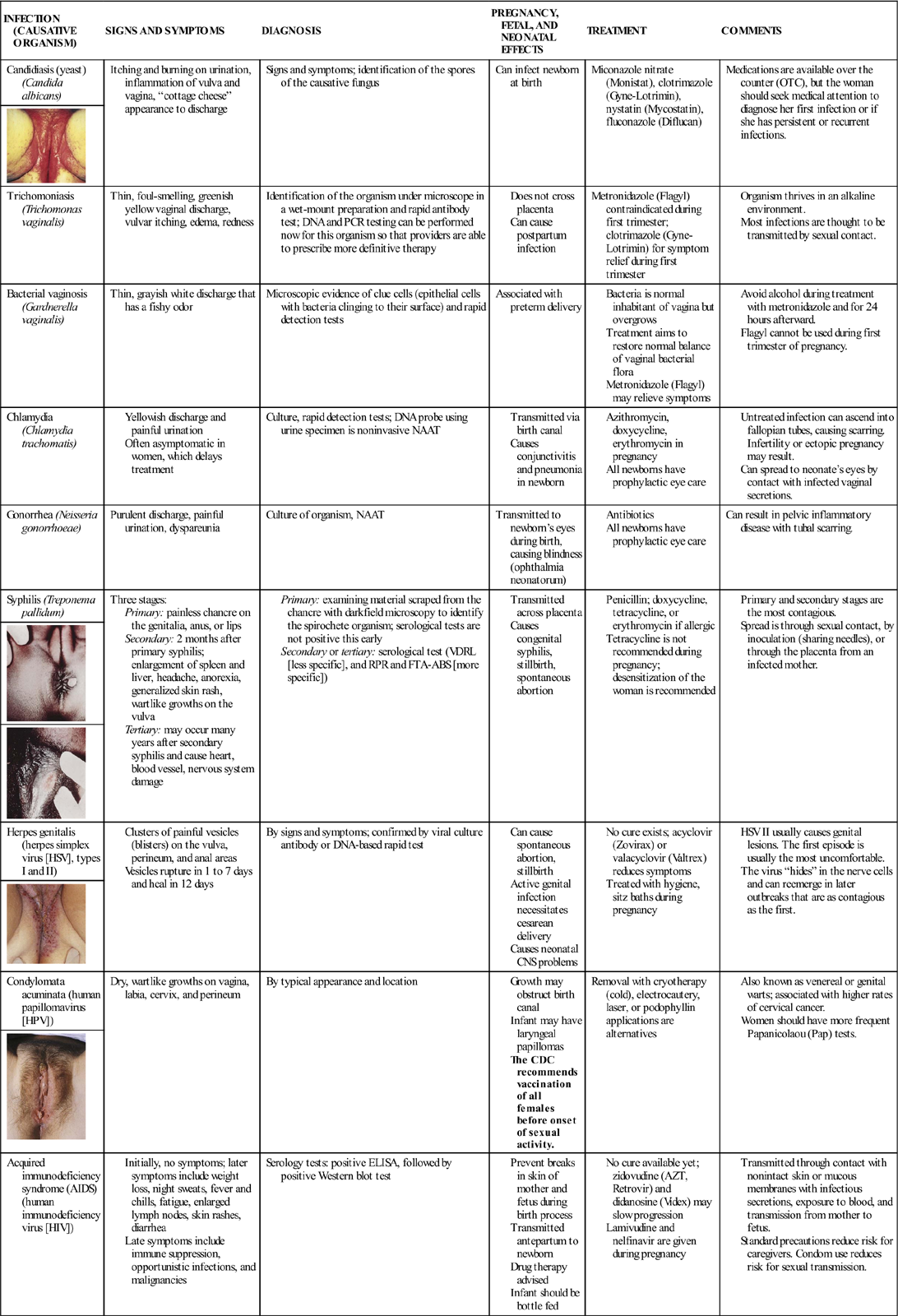
Nursing care related to STIs primarily focuses on patient education to prevent spread of these infections, including the following:
• Teaching signs and symptoms that should be reported to the health care provider
• Teaching measures to prevent spread of infection, such as use of a condom
• Explaining treatment measures
The incidence of STIs has increased over the past few decades. Teaching STI prevention to women across the life span is important because some viral STIs remain in the body for life and can have long-term complications. The most common viral STI is human papillomavirus (HPV), with more than 100 variations. HPV types 16 and 18 are associated with serious cervical cancer, and women who are immunocompromised are at the greatest risk. The use of condoms may not protect the woman if the male’s lesion is on the scrotum or inguinal folds. It may take 3 to 6 months after infection to develop visible warts. Treatment includes cryotherapy, laser vaporization, electrodiathermy, and electrofulguration with a loop electrode excision procedure. Topical agents are used, such as podofilox (Condylox), imiquimod (Aldara), and bichloroacetic acid (BCA). Lidocaine cream may be used 20 minutes before painful treatments. 5-Fluorouracil (5-FU) is no longer used for this condition because of serious side effects.
Herpes simplex virus II (HSV II) is another example of a viral STI that is recurrent and incurable. HSV infection during pregnancy can have serious consequences for the newborn.
Hepatitis B can be sexually transmitted if sexual practices include anal-oral sexual contact, digital rectal sexual intercourse, or multiple sex partners. Symptoms are nonspecific and include malaise, anorexia, nausea, and fatigue. Liver failure can develop. Hepatitis B vaccine can prevent the disease, and immunoglobulin can be given if known exposure has occurred.
Chlamydia trachomatis is the most common bacterial STI in the United States (Centers for Disease Control and Prevention [CDC], 2008). Treatment tends to be delayed because infection is often asymptomatic.
Gonorrhea (GC) is the second most common reportable infectious disease in the United States and a major cause of pelvic inflammatory disease (PID). The occurrence of gonorrhea in 2007 declined except for an increase of 1.8% in the black population. Casual sex in the 15- to 19-year age-group and sex associated with drug use are the highest-risk practices for GC infection (CDC, 2008). Several nucleic acid amplification tests are now available to detect chlamydia, GC, and trichomonas with a simple noninvasive urine sample, with results available in a few hours. Fluoroquinolones are no longer recommended for treatment of GC infections (CDC, 2008).
The rate of syphilis reached an all time low in 2000. However, over the past 7 years the rate has been increasing. Between 2006 and 2007, a 15.2% increase in the diagnosis of syphilis has been noted (CDC, 2008). Untreated syphilis is a risk factor in the spread of human immunodeficiency virus (HIV) infection and also leads to central nervous system (CNS), musculoskeletal, and heart complications. Most newborns of mothers infected with syphilis will have congenital syphilis or die. An external chancre is a characteristic first sign and resolves within 6 weeks without treatment; however, the disease spreads internally. A rash also occurs and resolves, and then the latent period of syphilis occurs and progresses to tertiary syphilis. Aortic aneurysms, dementia, and death can occur.
The number of women infected with HIV worldwide is staggering. Patient education plays a key role in prevention, quality of life, and compassionate and knowledgeable referral. Early diagnosis, access to care, medications, and safe sex practices are improving outcomes and decreasing occurrence. Universal HIV screening at pregnancy is a goal of the National Academy of Sciences Institute of Medicine, because many women do not realize they are infected in the early stages. Education for prevention is essential. Nurses may be less likely to consider the older age-group at risk and may miss opportunities for early detection and education for prevention. Sexual contact and intravenous (IV) drug use are the most common risk behaviors for HIV infection.
Prevention of disease is the key role of the nurse. The nurse must develop strategies, use initiatives, and contact adolescents in the community setting, schools, and churches. Teaching all age-groups healthy behaviors such as abstinence, safe sex practices, and discussion of STI prevention is essential. Improving access to care and early detection is also important. The CDC offers various free programs that are available over the Internet and can be used by nurses and teachers in the community to teach STI prevention.
Pelvic Inflammatory Disease
Pelvic inflammatory disease (PID) is an infection of the upper reproductive tract. Asymptomatic STIs are a common cause of PID. The cervix, uterine cavity, fallopian tubes, and pelvic cavity are often involved. Infertility may be the result.
The woman’s symptoms vary according to the area affected. Fever, pelvic pain, abnormal vaginal discharge, nausea and anorexia, and irregular vaginal bleeding are common. When examined, the abdomen and pelvic organs are often very tender. Laboratory tests identify common general signs of infection, such as elevated leukocytes and an elevated sedimentation rate. Cultures of the cervical canal are done to identify the infecting organism. Urinalysis is usually done to identify infection of the urinary tract.
Treatment may be administered on an inpatient or outpatient basis depending on the severity of the infection. Antibiotics are begun promptly to treat the infection. A change in antibiotic(s) is made if culture and sensitivity testing indicates that another one would be more effective.
Douching results in changes in the vaginal flora and predisposes the woman to the development of PID, bacterial vaginosis, and ectopic pregnancies. However, many women practice regular douching in the belief that it is cleansing. The nurse can play an important role in educating the woman to prevent PID. A diagnosis of PID is reportable to the local health department in many states.
Family Planning
Contraception
Contraception (birth control) may be part of the nurse’s responsibility in family-planning clinics, in physician or nurse-midwife practices, or on the postpartum or gynecology units of an acute care hospital. In addition, family members and friends may turn to the nurse as a resource person who can answer their questions about contraception. The nurse can play a part in helping couples choose and correctly use contraceptive methods that enable them to have children who are both wanted and well timed. The nurse’s role in family planning includes the following:
• Answering general questions about contraceptive methods
• Teaching the correct use of the method or methods of contraception that the patient chooses
A couple’s choice of contraception often changes as needs change. Factors that influence the choice of a contraceptive include the following:
• Age
• Health status, including risk for STI
• Religion
• Culture
• Impact of an unplanned pregnancy on the woman or family
• Convenience and degree of spontaneity that is important to the couple
• Expense
• Degree of comfort the partners have with touching their bodies
Contraception does not always prevent pregnancy. An important consideration for patients is how likely the method is to fail. A contraceptive technique may fail because the method is ineffective or the user is using the method inappropriately. The following two Healthy People 2020 (USDHHS, 2010) goals are relevant to the provision of family planning services:
Natural Family Planning
Natural family planning, also called fertility awareness, involves learning to identify the signs and symptoms associated with ovulation. The couple either abstains from intercourse or uses a barrier method during the period that is presumed to be fertile. The ovum is viable up to 24 hours after ovulation, and sperm are viable for 48 to 72 hours in the fallopian tube, although most die within 24 hours.
Natural family planning methods are acceptable to most religions. They require no administration of systemic hormones or insertion of devices. They are not only reversible but also can actually be used to increase the odds of achieving pregnancy when the couple desires a child.
Natural family planning requires extensive assessment and charting of all the changes in the menstrual cycle. The woman must be highly motivated to track the many factors that identify ovulation. Both partners must be willing to abstain from intercourse for much of the woman’s cycle if the method is used to prevent pregnancy. They must also be willing to accept the relatively high failure rate of 20%. Most women use a combination of the following four methods for predicting when they are fertile to increase the predictive value over that of each method on its own.
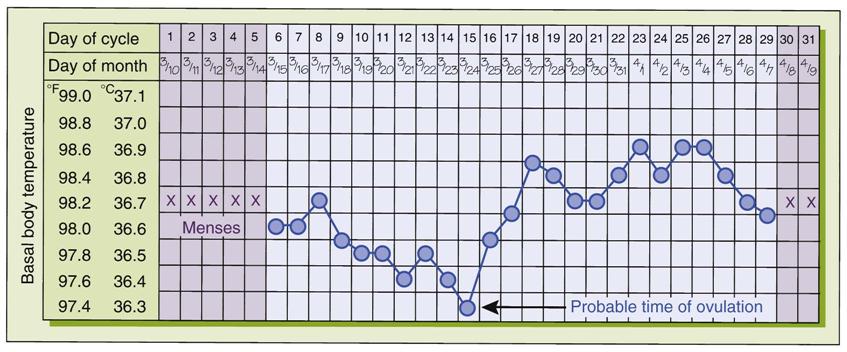
Basal Body Temperature
The basal body temperature (BBT) is taken upon awakening and before any activity (Figure 11-1). This technique is based on the fact that the basal temperature rises very slightly at ovulation (about 0.2° C [0.4° F]) and remains higher in the last half of the cycle. Unfortunately, BBT is better at identifying that ovulation has already occurred rather than predicting when it is about to occur. The most important time point to identify in attempting conception or contraception is the day before ovulation, rather than the day of ovulation (Fehring et al., 2008).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree