Nursing Care of the Newborn
Objectives
2. Discuss the nursing responsibilities concerning the care of the newborn infant.
3. Describe a neutral thermal environment.
4. Demonstrate three ways to hold a newborn.
5. Demonstrate the proper way to suction the newborn with a bulb syringe.
6. Describe newborn bathing and cord care to parents.
7. Interpret instructions for parents about newborn stools and voiding patterns.
8. Discuss care of the circumcised and uncircumcised penis.
9. Describe pain assessment and control in the newborn.
10. Explain the discharge care plan.
11. Discuss five aspects of newborn care that the mother should understand before discharge.
Key Terms
circumcision (sĭr-kŭm-SĬZH-ŭn, p. 197)
cord care (p. 186)
en face (p. 191)
kangaroo care (p. 188)
neutral thermal environment (p. 187)
ophthalmia neonatorum (p. 188)
retraction (rē-TRĂK-shŭn, p. 198)
 http://evolve.elsevier.com/Leifer/maternity
http://evolve.elsevier.com/Leifer/maternity
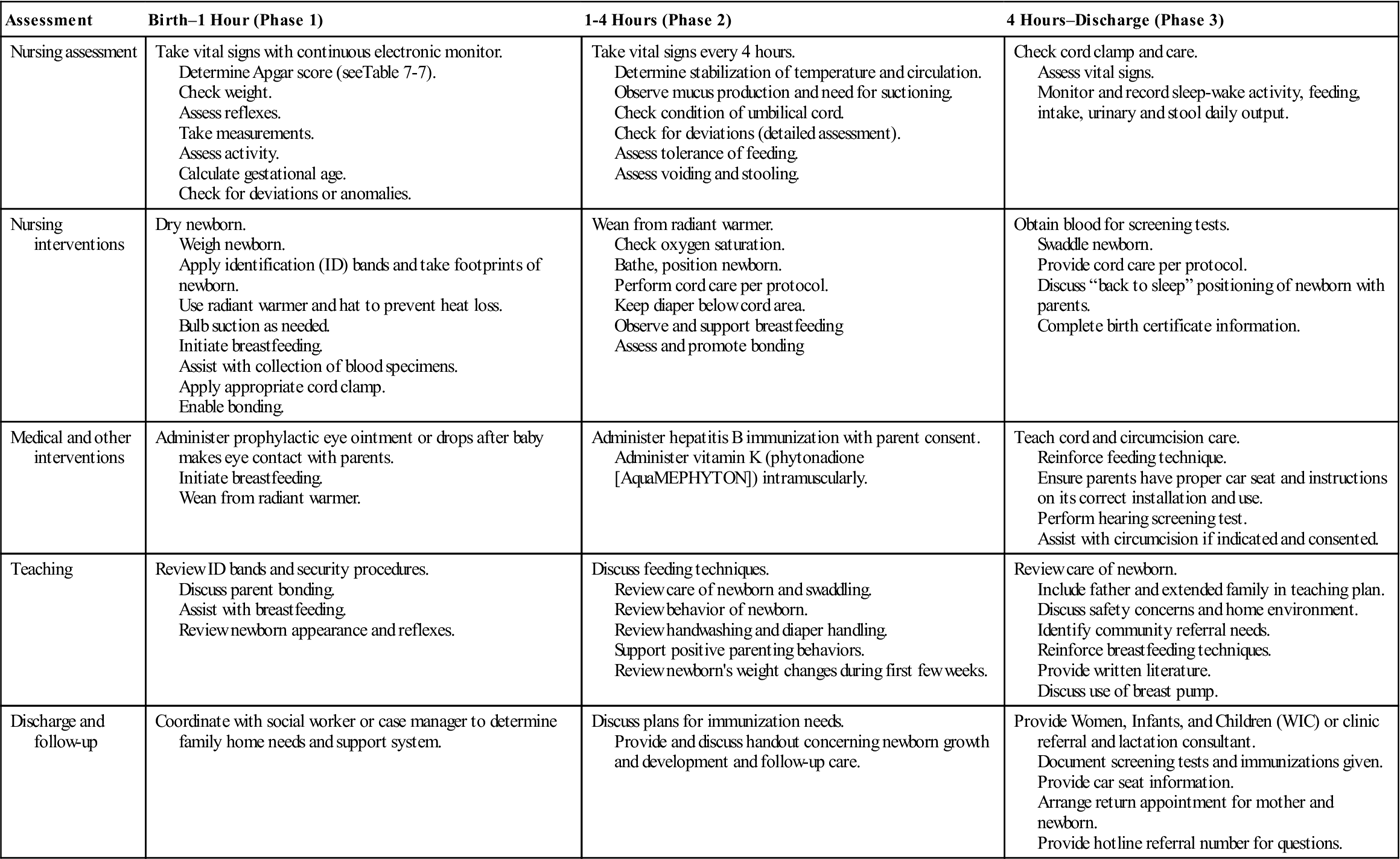
Three Phases of Newborn Care
The nursing care of the newborn is directed toward promoting the physical well-being of the baby and supporting the family unit. The immediate care of the newborn takes place in the delivery room and is discussed in Chapter 7. Because numerous physiologic adaptations begin right after birth, immediate nursing care is very important. The first goal is to help the newborn make the transition to extrauterine life. The second goal is to assess and provide nursing care that supports the newborn’s health status. The third goal is to teach the parents and family members how to care for and bond with the new baby.
Three phases of newborn care are discussed that span from the immediate neonatal period until the infant has stabilized in the transition to extrauterine life. The three phases of transition are:
Phase 1: Birth to 1 hour—first period of reactivity; takes place in delivery room (see Chapter 7)
Phase 2: One to 4 hours—may take place in the labor, delivery, recovery, and postpartum (LDRP) room, nursery, or parents’ room; when the initial detailed health assessment is completed (see Chapter 9)
This chapter briefly reviews phases 1 and 2 and focuses on phase 3.
A clinical pathway indicates specific care given over a specified period that is related to a planned outcome. It includes nursing assessments, interventions, medical interventions, teaching, and discharge and follow-up care (Clinical Pathway 10-1).
Phase 1 Care: Nursing Interventions
Clamping the Umbilical Cord and Cord Care
The umbilical cord is initially white and gelatinous in appearance. It contains two umbilical arteries and one vein in the center of the umbilical cord. Deviations in the number of vessels in the cord could indicate a congenital anomaly and must be reported to the health care provider. The cord begins drying within 1 to 2 hours after birth. Bleeding from the cord or a foul odor should be reported immediately.
After the newborn is stabilized in phase 1 care, a disposable umbilical clamp is applied and the cord is cut to a shorter length. Before discharge, the parents are shown how to care for the umbilical cord stump at home. The cord clamp may be removed before
discharge if the cord is dry and crisp, or it may be left on at discharge and discarded when the cord falls off, which usually occurs within 10 days. Parents are taught cord care, which may include dipping a cotton swab in isopropyl alcohol, triple dye, saline, or a solution prescribed by the health care provider and using it to clean around the base of the cord where it joins the skin. The cord stump is allowed to dry (Skill 10-1).
Studies have shown that newborns who have cord care involving the application of topical human breast milk, or dry care, take less time for cord separation and have fewer infection risks (Vural & Kisa, 2006). Cleansing is done at every diaper change until the cord stump falls off. The nurse shows the parents how to fold the diaper below the level of the umbilicus so that it will not become wet with urine. A cord that is moist or red or has a discharge or a foul odor should be reported immediately to the health care provider.
Identification and Security
Matching identification (ID) bands are placed on the newborn’s wrist and ankle and the mother’s wrist in the delivery room. In some hospitals, the partner also receives a wrist band with matching numbers. For security reasons, many hospitals have either an umbilical clamp or ID wrist band with an electronic sensor attached that will sound an alarm if the newborn is taken out of the unit (Figure 10-1). The ID band is checked by the nurse and mother at any time the newborn is separated or returned to the mother and before discharge. The nurse and mother verify the ID bands together.
Birth Certificates
Birth certificates are completed before the infant is discharged or within 48 hours of birth. Birth certificates include vital data concerning the mother and infant that can be used for research and statistical purposes. Valid information can aid in improving public health strategies and formulating public health action plans. Ninety-nine percent of all births were registered on official birth certificates in 1998 (Northam & Knapp, 2006).
Birth certificate information is sent to the Bureau of Vital Statistics via computer. The data recorded on the birth certificate should be reviewed by the health care provider to increase the validity and reliability of information recorded. Birth certificates are required throughout the life of the child for admission to school, employment, travel, and so forth.
Thermoregulation
Maintenance of temperature—or thermoregulation—immediately after birth is discussed in Chapters 7 and 9. The technique of assessing temperature is reviewed in Chapter 9. Maintenance of a neutral thermal environment after birth aids the infant in achieving thermoregulation. A neutral thermal environment is maintenance of an environmental temperature at which oxygen consumption is minimal but adequate to maintain body temperature (Kenner & Lott, 2007). Strategies to conserve heat and to prevent cold stress in the newborn are important nursing responsibilities. Cold stress is discussed in Chapter 9.
The American Academy of Pediatrics (1997) defines normal rectal or axillary temperatures to be between 36.5° C and 37.5° C (97.7° F and 99.5° F). Hypothermia is classified as mild if the temperature is 36° C to 36.4° C (96.8° F to 97.5° F), moderate at 32.0° C to 35.9° C (89.6° F to 96.6° F), and severe if less than 32.6° C (90.7° F). Newborns are at greater risk for hypothermia than adults are because they have a higher body surface area to body mass ratio, higher metabolic rate with limited metabolic stores, and immature thermoregulation mechanism.
Although hypothermia can be a sign of a central nervous system (CNS) infection or metabolic anomaly, about 20% of all normal newborns are seen with hypothermia, and about 50% of newborns have one or more episodes of hypothermia in the first 72 hours of life (Li, Sun, & Neubauer, 2004). Hypothermia can cause increased cell metabolism, increased oxygen consumption, hypoglycemia, and other complications in the newborn and should be actively prevented. Strategies to conserve heat and to prevent cold stress are important nursing responsibilities.
In phase 1 care, the newborn is placed in a radiant warmer with a temperature probe on the abdomen until body temperature is stabilized. In phases 2 and 3 care, when the newborn is in the nursery or the mother’s room, the baby’s axillary temperature is recorded every 4 hours (see Skill 9-1). The newborn is wrapped warmly and placed in a bassinet. A hat is placed on the newborn’s head to conserve heat because the head has a large surface area, and the newborn is dressed in a shirt and diaper only. When the newborn’s temperature is stabilized, a bath may be given to remove excess blood and vernix. The bath does not need to remove all vernix because it provides some antimicrobial protection. Until the completion of the initial bath, the nurse should wear gloves and a cover gown when handling the newborn (see Appendices A and B). The room temperature should be maintained at 24° C to 25° C (75.2° F to 77° F). The newborn is weighed and measured on admission to the newborn nursery.
Skin-to-skin contact, with the newborn placed on the mother’s naked chest, has been shown to be an effective temperature stabilizer (Galligan, 2006). The infant is covered with a blanket and may wear a hat. Skin-to-skin (kangaroo care) is effective to warm a hypothermic infant when the mother’s temperature is normal, her skin is dry, and she is relatively comfortable (Figure 10-2).
Administering an Intramuscular Injection
The newborn should receive vitamin K (phytonadione [AquaMEPHYTON] 0.5 to 1 mg) (see Skill 7-8). It is given intramuscularly in the midanterior thigh (the vastus lateralis muscle) where the muscle development is adequate. Because newborns cannot synthesize vitamin K in the intestines without the presence of bacterial flora, they are deficient in clotting factors, and vitamin K must be administered as a prophylaxis to assist in clotting.
Prophylactic Eye Care
The newborn can acquire an eye infection, such as gonorrhea or chlamydia, when passing through an infected birth canal. Prophylaxis against gonococcal ophthalmia neonatorum, an infection that can cause blindness, is required for all newborns. Erythromycin (Ilotycin) ophthalmic ointment is commonly used for prophylactic eye care because it produces less eye irritation than other eye medications and also destroys the Chlamydia organism. Ideally, a single-unit dose (new tube) of ointment is used. The ointment is placed so that it reaches all areas of the conjunctival sac (see Skill 7-9). It is recommended that eye prophylaxis be administered approximately 1 hour after birth to allow time for newborn-parent interaction without the newborn’s vision being disturbed.
Phase 2 Care: Routine Nursing Interventions
Weighing and Measuring
Weight
The infant is weighed in the birthing room or when admitted to the nursery (Skill 10-2). Disposable paper is put on the scale, and the scale is balanced to zero according to its model. The unclothed infant is then placed on the scale. The nurse’s hand should not touch the infant but should be kept just above him or her to prevent falls. The weight must be converted to grams for gestational age assessment. The normal term newborn weighs approximately 3405 g (7 lbs, 8 oz). The normal newborn may lose up to 10% of its birthweight in the first week (physiologic weight loss) and regains the birthweight by the tenth day. After the first week, the newborn typically gains 200 g (7 oz) per week (gestational age is discussed in Chapter 15).
Measurements
Three typical measurements are length, head circumference, and chest circumference. A disposable tape measure is used. The tape should not be pulled out from under the infant to avoid giving a paper cut. Measurements must also be noted in centimeters for gestational age assessment.
Length
There are several ways to measure length. Some facilities have a tape measure applied to the clear wall of a bassinet. The nurse places the infant’s head at one end, extends the leg, and notes where the heel ends. Another method is to bring the infant to the bassinet or warmer with the scale paper. The paper is marked at the top of the head, the body and leg are extended, and the paper is marked where the foot is located. Length is measured between the marks. Still another method involves placing the zero end of the tape at the infant’s head, extending the body and leg, and stretching the tape to the heel. The average length of the full-term newborn is 48 to 53 cm (19 to 21 inches).
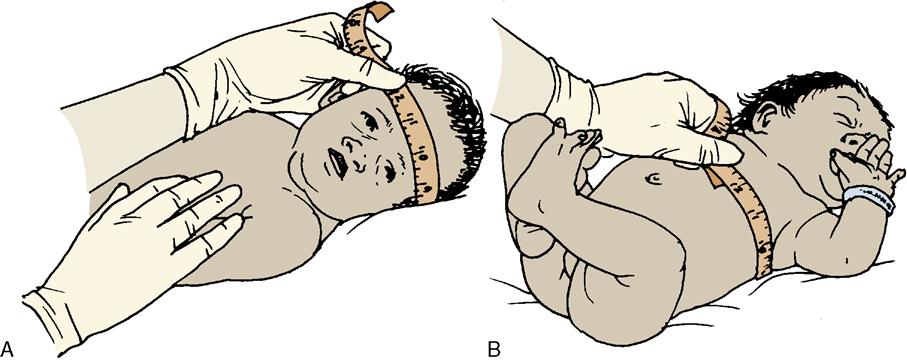
Head Circumference
The fullest part of the infant’s head is measured just above the eyebrows (see Skill 10-2). Molding of the head may affect the
accuracy of the initial measurement. The average head circumference of the full-term newborn is 33 to 35.5 cm (13 to 14 inches).
Chest Circumference
Chest circumference is measured at the nipple line. The average chest circumference of the full-term newborn is 30.5 to 33 cm (12 to 13 inches) (see Skill 10-2).
Protection from Infection
Newborns are susceptible to infection, and prevention of infection constitutes a major part of nursing care and parent teaching. Cracks in the skin, particularly on the newborn’s hands, feet, and umbilical cord, are especially vulnerable to infection. All newborns are also at risk for health–care-acquired infections. Many facilities require all personnel who have direct contact with newborns to perform a 3-minute scrub (hands to elbow) procedure at the beginning of each shift. The hands must always be cleaned, with either soap and water or an alcohol-based hand sanitizer, before and after contact with a newborn or any soiled surface. Alcohol-based hand sanitizers should be available for use by personnel, parents, and visitors. Avoiding cross-contamination is an important objective in newborn care.
Signs of newborn infection include poor feeding, lethargy, and periods of apnea. More obvious signs of infection are drainage, redness, and possible odor from the umbilical cord stump, eyes, or circumcision site.
Hepatitis B Vaccination
The American Academy of Pediatrics and the Centers for Disease Control and Prevention (AAP, 2009) recommend that all newborns receive their first vaccination against hepatitis B within 12 hours after birth, regardless of the mother’s hepatitis B surface antigen (HBsAg) status. It is important that newborns receive their second vaccination at approximately 1 month of age and their third one at 6 months of age.
Assessing and Managing Pain in the Newborn
The nurse is responsible for understanding physiologic and behavioral responses to pain in infants and for providing appropriate relief measures. Untreated pain in the preterm or term newborn or in early infancy can have long-term effects because pain pathways and structures required for long-term memory are well developed by 24 weeks’ gestation.
Several pain assessment tools are available:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



 Skill 10-1
Skill 10-1




 Did You Know?
Did You Know? Skill 10-2
Skill 10-2