Health care systems
Midge Noel Ray
Objectives
• Outline the role of the federal, state, and local governments in the provision of health care.
• Identify legislation that affects or regulates health care in the United States.
• Distinguish between the various health care organizations responsible for providing health care.
• Describe the organizational structures of the hospital as discussed within this chapter.
• State current mechanisms of health care financing.
• Describe specific information technologies and how they affect the health care systems.
Key words
Accreditation
Acute care
Advance directive
Alternative medicine
Ambulatory care
Ancillary services
Assisted living facility
Bed size (bed count)
Behavioral health
Benefit period
Beneficiaries
Capitation
Case management
Catchment area
Certification
Claim
Client
Clinical privileges
Coinsurance
Complementary and alternative medicine
Complementary medicine
Conditions of participation
Continuum of care
Contracted amount
Copayment
Critical access hospital
Deductible
Deemed status
Direct pay
Durable medical equipment
E-health
Electronic health record
Electronic medical record
Emergency department
Encounter
Episode of care
Evidence-based medicine
Ex officio
Fee-for-service
Fiscal intermediary
Gatekeeper
Governing body
Health
Health care services
Home health care
Horizontal integration
Hospice
Hospital
Hospital ambulatory care
Hospital formulary
Hospital inpatient
Hospital patient
Indigent
Indirect pay
Inpatient
Insurance
Integrated delivery system
Licensure
Life care centers
Long-term care
Managed care
Medicaid
Medically indigent
Medicare
Morbidity
Mortality
Nursing care
Nursing facility
Observation unit
Osteopathic medicine
Out-of-pocket costs
Outpatient
Outsourcing
Palliative care
Participating physicians
Patient
Patient assessment
Patient-centered care
Payer
Personal health record
Point of service
Practice Act
Preexisting condition
Preferred provider organization
Premium
Primary care
Proprietary
Prospective payment system
Provider
Rehabilitation
Reimbursement formula
Resident
Respite care
Retrospective payment system
Satellite clinic
Secondary care
Self-pay
Skilled nursing facility
Sliding-scale fee
Solo practice
Swing beds
Tertiary care
The Joint Commission
Third-party payer
Trauma center
Triage
TRICARE
Usual, customary, and reasonable charges
Utilization review
Vertical integration
Abbreviations
ACF—Administration for Children and Families
ACS—American Cancer Society/American College of Surgeons
AHA—American Hospital Association
AHIMA—American Health Information Management Association
AHRQ—Agency for Healthcare Research and Quality
AIDS—Acquired Immunodeficiency Syndrome
AMA—American Medical Association
ANA—American Nurses Association
ANSI—American National Standards Institute
AOA—American Osteopathic Association
AoA—Administration on Aging
BCBS—Blue Cross and Blue Shield
CAAHEP—Commission on Accreditation of Allied Health Education Programs
CAH—Critical Access Hospital
CAHIIM—Commission on Accreditation of Health Informatics and Information Management Education
CAM—Complementary and Alternative Medicine
CARF—Commission on Accreditation of Rehabilitation Facilities
CDC—Centers for Disease Control and Prevention
CDSS—Clinical Decision Support System
CEO—Chief Executive Officer
CFO—Chief Financial Officer
CHAMPUS—Civilian Health and Medical Program for the Uniformed Services
CHAP—Community Health Accreditation Program
CHC—Community Health Center
CIO—Chief Information Officer
CMS—Centers for Medicare and Medicaid Services
CNA—Certified Nursing Assistant
COBRA—Consolidated Omnibus Reconciliation Act
COCA—Commission on Osteopathic College Accreditation
COO—Chief Operating Officer
COP—(Medicare) Conditions of Participation
CRNA—Certified Registered Nurse Anesthetist
DHHS—Department of Health and Human Services
DME—Durable Medical Equipment
DO—Doctor of Osteopathy
DRG—Diagnosis Related Group
DSS—Decision Support Systems
ED—Emergency Department
EHR—Electronic Health Record
EMR—Electronic Medical Record
EMTALA—Emergency Medical Treatment and Active Labor Act
ESRD—End-Stage Renal Disease
FDA—Food and Drug Administration
FI—Fiscal Intermediary
FLEX—Federation Licensing Exam
GDP—Gross Domestic Product
HCFA—Health Care Financing Administration (now CMS)
HFAP—Healthcare Facilities Accreditation Program
HIPAA—Health Insurance Portability and Accountability Act
HCO—Health Care Organization
HIM—Health Information Management
HL7—Health Level Seven
HMO—Health Maintenance Organization
HRSA—Health Resources Services Administration
IDS—Integrated Delivery System
IPA—Independent Practice Association
IHS—Indian Health Service
IOM—Institute of Medicine
JC—The Joint Commission
JCAHO—Joint Commission on Accreditation of Healthcare Organizations (now The Joint Commission)
LPN—Licensed Practical Nurse
LTC—Long-Term Care
MCAT—Medical College Admission Test
MCO—Managed Care Organization
MD—Medical Doctor
MMA—Medicare Modernization Act
NBME—National Board of Medical Examiners
NCCAM—National Center for Complimentary and Alternative Medicine
NCQA—National Committee For Quality Assurance
NHII—National Health Information Infrastructure
NHIN—National Health Information Network
NIH—National Institutes of Health
NLN—National League for Nursing
NLNAC—National League for Nursing Accrediting Commission, Inc.
NP—Nurse Practitioner
OIG—Office of Inspector General
OSHA—Occupational Safety and Health Administration
PA—Physician Assistant
PHR—Personal Health Record
PHS—Public Health Service
POS—Point of Service
PPO—Preferred Provider Organization
PPS—Prospective Payment System
QIO—Quality Improvement Organization
RN—Registered Nurse
SCHIP—State Children’s Health Insurance Program
SNF—Skilled Nursing Facility
SSA—Social Security Administration
TEFRA—Tax Equity and Fiscal Responsibility Act
VA—Veterans Administration
VISN—Veterens Integrated Service Networks
WEDI—Workgroup on Electronic Data Interchange
Student Study Guide activities for this chapter are available on the Evolve Learning Resources site for this textbook. Please visit http://evolve.elsevier.com/Abdelhak.
When you see the Evolve logo,  go to the Evolve site and complete the corresponding activity, referenced by the page number in the text where the logo appears.
go to the Evolve site and complete the corresponding activity, referenced by the page number in the text where the logo appears.
Health information management (HIM) is a vital component of the health care delivery system. Therefore, it is crucial for health information professionals to understand the structure of that system. This chapter introduces the reader to the health care system, including what the system is like and how it functions, and identifies its components. Topics include the history, influencing factors, payers, regulatory agencies, structure, operation, and workforce of health care systems in the United States.
Evolution of health care systems in the united states
From its inception hundreds of years ago to the present, the health care system has been continually evolving. In the United States, virtually every person is in some way a patient or a consumer of health care at some point. Most people are born either in a hospital or outside the hospital with the assistance of a health care professional. Other people come in contact with the health care system in a variety of ways, including physical examination, immunizations, employee physicals, school vision and hearing screens, emergency care, and public health service announcements.
Before proceeding, see Box 1-1 for key definitions.
Health care in the 19th century
The 19th century saw the development and organization of professional education and health-related associations. The first school in the United States dedicated to training physicians was founded in 1765 in Philadelphia. Before this time, the only training an American physician received was by way of apprenticeship with an older physician. As the population in the United States grew and moved westward, the demand for more hospitals and physicians increased. To meet the growing need for more physicians, a large number of new medical schools were opened, most of which were profit oriented. By the end of the 19th century, there were no fewer than 400 medical schools in the United States, most of questionable quality.3
In 1847, a group of physicians formed the American Medical Association (AMA) for the primary purpose of establishing and supporting a code of ethics for physicians in their duties to their patients and the profession. The AMA initially examined the poor quality of medical education and the questionable ethics of practicing physicians. Today, membership in the AMA is open to any physician in good standing and includes local, city, and state medical societies. The AMA is dedicated to promoting the science and art of medicine, improving public health, making health care policy, and servicing the professional needs of its members.4
The American Hospital Association (AHA) was founded in 1898 for the purpose of promoting public welfare by providing better health care in the hospitals. The AHA offers education for health care leadership and provides health care information on trends and issues. AHA maintains data on hospital profiles and represents hospital interests in legal, legislative, and regulatory matters, all of which are directed at improving the nation’s health care system.5
In the late 19th century, states became involved in health care when mental health reformers pushed for an innovation, that “insanity” be managed as a medical or mental disorder. State governments established mental institutions for the confinement of the mentally ill rather than housing them in the poorhouses and prisons. However, because of inadequate funding, mental institutions soon became overcrowded, and living conditions were deplorable.
In the mid-1800s, there was evidence of the earliest forms of managed care. Plantation owners in Hawaii, mining companies in Pennsylvania and Minnesota, and lumber companies in Washington, Wisconsin, and Michigan tried to attract and keep immigrant workers by offering medical care for their workers. The companies contracted with local physicians and hospitals for a set number of beds. Some of the companies even built medical clinics and hospitals. Physicians who agreed to contract with these companies were ostracized from the local medical societies and were even threatened with revocation of their medical licenses.6
Twentieth-century reforms
In the early 1900s, most hospitals were viewed as boardinghouses for the poor and sick; physicians did not take histories and perform physical examinations on admission, and seldom did they document assessments or diagnoses. The private sector, however, showed little interest in serving the population as a whole; the assumption was that local government would pay for health care for the poor.7
Between the 1870s and 1920s, the number of U.S. hospitals increased from fewer than 200 to more than 6000. Private benevolence was responsible for establishing hundreds of new hospitals that were not interested in serving the poor. By 1910, there were as many hospitals per 1000 population as there are today, and, as is still true today, part of the population was not being served.
In 1910, Abraham Flexner conducted a study on the quality of medical education in the United States. The famous Flexner Report identified serious problems and inconsistencies that existed in medical education. As a result, many of the profit-oriented schools were closed, and those that remained open underwent significant curriculum revision. In addition, the AMA initiated an accreditation process that ranked schools according to their performance. The Flexner Report established a model for medical education that is still used in many medical schools today.
In 1913, the American College of Surgeons (ACS) was founded. One of its purposes was to develop a system of hospital standardization that would improve patient care and recognize hospitals that had the highest ideals. To establish the standards, the ACS began collecting data from health records. At this time, the ACS realized that health record documentation was inadequate. In 1917, the ACS founded the Hospital Standardization Program, which laid the groundwork for establishing standards of care. The first ACS report revealed that of the 692 hospitals surveyed, only 89 met minimum standards, and some of the most prestigious hospitals did not meet approval. After issuing this report, the ACS adopted the Minimum Standards, which identified the essential standards for proper care and treatment of hospital patients. The Minimum Standards included specifications that established an organized medical staff and required that certain diagnostic and therapeutic facilities be available and that a health record be written for every patient. The standards specified, among other things, that the record be complete, accurate, and accessible.7 In fact, the standards for health care in use today continue to encompass the documentation requirements identified in 1919 (Box 1-2).
Although hospital admissions increased dramatically from 1935 to the end of World War II in 1945, the unemployed, disabled, elderly, and others who could not pay were excluded. The economy was growing, and technological advances continued in the medical field. The need for more hospitals and high-quality health care accessible to all Americans increased. In 1946, Senators Lister Hill and Harold H. Burton sponsored the Hospital Survey and Construction Act. This legislation, known as the Hill-Burton Act, provided funding for the construction of hospitals and other health care facilities on the basis of state need. For the next 25 years, as a result of this program, hospital construction and expansion flourished.
In the early 1950s, the ACS Hospital Standardization Program was overburdened by the huge increase in the numbers of hospitals, nonsurgical specialties, and the perception that medical care was becoming more sophisticated. As a result, The Joint Commission on Accreditation of Hospitals (JCAH) was founded in 1952 and adopted the Hospital Standardization Program from the ACS.7
In the 1950s, Americans began to want more technology, accessible to all people at an affordable cost. As advances were made in the medical field, the demand for health care services and the cost to provide those services grew. The attitude became “more is better.” In addition, medical advances extended life expectancy, resulting in an increase in the elderly population. With the growing elderly population came a growth in the incidence of chronic diseases. As hospital care became more expensive, those who were uninsured or underinsured—primarily the poor and the elderly—could not access the health care system. Up to this point, the federal and state governments did little to control hospital costs. However, in 1965, Congress amended the Social Security Act of 1935, Public Law 89-97, establishing both Title XVIII, Health Insurance for the Aged (now called Medicare), and Title XIX, which extended the Kerr-Mills Medical Assistance Program (now called Medicaid). Medicare is a federally funded program that provides health insurance for elderly people and certain other groups, and Medicaid supports the states in paying for health care for the indigent.8 An indigent is one who is without the means for subsistence—poor or impoverished. At this time, the federal government became a significant player in the health care delivery system because it not only funded and operated the Medicare program but also assisted the states with the Medicaid program. These programs are discussed further in the section on financing health care later in this chapter. In response to the federal government’s establishing and regulating the Medicare and Medicaid programs, states began writing more and, in some cases, their first regulatory codes.

In the 1960s, there was a proliferation of various health care facilities, including long-term care, psychiatric and substance abuse facilities, and programs for the developmentally disabled. The JCAH not only redefined the standards to be the optimal achievable, as opposed to minimum standards, but also began developing standards for the various types of health care facilities.7 In 1987, the JCAH reflected its broader scope by changing its name to The Joint Commission on Accreditation of Healthcare Organizations (JCAHO) (Box 1-3). It has been known as the Joint Commission since early 2007.
Toward the turn of the century, there were not only concerns regarding the cost of health care and quality but also increased awareness of patient safety. In 1999, the Institute of Medicine (IOM) published To Err Is Human, which reported that between 44,000 and 98,000 deaths per year are attributable to medical errors at a cost of approximately $17 billion to $29 billion.3 Medical errors include adverse drug events, mismatched blood types, and surgery on wrong patient or limb. With this report has come increasing attention to patient safety and bringing more information to the point of care with the use of technology.9 In 2004, the World Health Organization began supporting dialogue among health leaders, consumers, and health ministers to discuss patient safety.
Health care in the 21st century
The health care system in the United States has evolved into a complex system composed of multiple types of facilities, providers, payers, and regulators and consumers who are demanding more and better health care. There is a proliferation of sophisticated technology for both medical practice and information management. The technology available in financial, administrative, and clinical information systems affects the quality, cost, and efficiency of health care systems. The technological advances in medicine support prevention, early diagnosis, shorter hospital stays, patient safety, and increased outpatient services and home health care.
In 2007, U.S. health care spending was 6.1% of the federal budget, and health care costs are approximately 16.2% of the U.S. gross domestic product (GDP).10 The total national health care expenditures in the United States in 2007 were $2.2 trillion,11 yet millions of people were uninsured or could not access the system. Those without insurance either cannot afford it or cannot find an insurance company that is willing to sell them a policy at any price. Insurance companies often cancel contracts with patients who have expensive (catastrophic costs) health care needs, as is the case with chronic conditions such as cancer, kidney disease, and heart disease. Those who cannot access the health care system may live in areas where little or no health care is available or lack transportation.
Advances in technology and scientific developments have supported a healthier lifestyle and a longer life expectancy. For women, life expectancy increased from 49.1 years in 1900 to 80.1 years in 2003, and for men, from 49.1 years to 74.8 years.11 With the longer life expectancy has come tremendous growth in the need for home health and long-term care (LTC).
Health care continues to be costly and not accessible to all citizens, yet consumers continued to demand more and better care. As a result, there has been tremendous pressure to reform the manner in which health care is delivered to contain the cost and still provide high-quality care to all.12 The sources of the pressure are numerous. They include the federal government, which is concerned with the cost of health care and its accessibility; the consumers, who have become more educated and are demanding more and better quality; the providers, who want to maintain their market share, cut their costs, and realize a profit; and the taxpayers, who are underinsured or uninsured or who feel overburdened with taxation that finances health care. The changes that are occurring are evidenced by the shift from inpatient care to outpatient care, increased legislation on patient rights, and the increase in alternative health care systems. The result is a health care system that is evolving into a more patient- or consumer-centric culture. Patient-centered care allows patients to have more control over their care and access to their health care information. Evidence of patient-centric care includes the following:
• Supporting patients in setting up their own personal health records (PHRs) by making provider records accessible to patients through Web portals and other methods.13
• Protecting the patient’s privacy and security of health information by legislation.
• Increasing communication between patient and provider by e-mail or voicemail.
AHIMA has defined a PHR as:
The personal health record (PHR) is an electronic, lifelong resource of health information needed by individuals to make health decisions. Individuals own and manage the information in the PHR, which comes from healthcare providers and the individual. The PHR is maintained in a secure and private environment, with the individual determining rights of access. The PHR does not replace the legal record of any provider.13
With such problems as the escalating cost of health care, the number of uninsured, and the existence of underserved rural areas where medical care is not available, there has been great debate on health care reform and there continues to be a great impetus to reform the manner in which health care is delivered in the United States. The debates/discussions resulted in numerous plans proposed by professional organizations, members of Congress, state governments, and the federal government. The various plans for reform addressed issues such as universal coverage, meaning health care for every citizen, health care costs, and the quality and safety of the health care provided.
As a result, in 2010 President Obama signed into law the Patient Protection and Affordable Health Care Act of 2010 and the Health Care and Education Reconciliation Act of 2010. The Health Reform Bill, as it is collectively called, provides public or private health insurance coverage for more than 30 million uninsured Americans. The provisions of the Health Reform Bill will be phased in over many years and will impact employers, providers, insurers, group health plans and taxpayers. The law is quite comprehensive (over 3000 pages) and affects numerous entities in numerous ways. For example, the law mandates that large employers provide employee health care coverage or pay a penalty and smaller businesses may earn tax credits if they offer coverage. People who currently do not have health care coverage will have several options for obtaining health care insurance. The law expands Medicaid so that more, lower income people will be eligible for benefits and then there is a penalty for individuals who do not get health care insurance by 2014. Among many other mandates, the bill also allots additional resources to fight health care fraud and abuse. The full text of the two laws are published in the Federal Register.14
Healthy people
The U.S. Department of Health and Human Services (DHHS) establishes science-based objectives every 10 years that promote health and prevention of disease. One of the DHHS reports is Healthy People 2000, which used data systems to identify national opportunities for health improvement. Some of the national data systems used to formulate the goals that would lead to a better quality of life include data on adult use of tobacco, a continuing survey of individual food intake, a national crime survey, and birth and infant death data. Healthy Communities 2000: Model Standards, Guidelines for Community Attainment of Year 2000 Objectives was developed to provide assistance to state and local governments in reaching their goals.15 This report was updated as Healthy People 2010, which identified specific national objectives for disease prevention and health promotion. Although the Healthy People 2010 objectives are disease- and indicator-specific, the primary goals are to increase the quality and years of healthy life and to eliminate health disparities.16
As of this writing, Healthy People 2020 is in development and has two phases. The first phase was the publication of the mission, vision, and goals for promoting health and preventing disease in the United States. The second phase is the publication of the specific objectives and guidance for achieving the objects. Currently, the proposed objectives for Healthy People 2020 are under development.17
Regulatory agencies and organizations
External forces that regulate the health care industry include, but are not limited to, the DHHS, The Joint Commission, the American Osteopathic Association, the Community Health Accreditation Program (CHAP) of the National League for Nursing, the Commission on Accreditation of Rehabilitation Facilities (CARF), and the state departments of public health. The regulatory activities of health care facilities are primarily directed at quality, utilization, and cost of care, whereas the regulatory activities that affect educational programs and the health care workforce are directed at quality and supply of manpower.
Federal government as regulator
The federal government has been involved in the regulation of the health care systems since the early part of the century, primarily in the consumer’s interest. In 1906, the Pure Food and Drug Act was passed because of the unsanitary conditions that prevailed in the food production industry, and in 1938 the Food, Drug, and Cosmetic Act was passed to regulate the food, drug, and cosmetic industry. This act mandated that manufacturers prove safety, specify composition and method of manufacture, and provide labeling and package inserts. Interestingly, it was not until 1962 that manufacturers were required to prove efficacy (i.e., how effective a product is).
Department of health and human services
The principal agency of the federal government that is primarily responsible for the numerous regulatory programs that affect the health industry is the DHHS, formerly the Department of Health, Education, and Welfare (HEW). HEW, created in 1953, underwent numerous reorganizations that led to the creation of the DHHS in 1980. The organization of the DHHS is complex and includes numerous administrations, divisions, offices, centers, and agencies; the highest ranking official is the secretary of the DHHS, who advises the president of the United States on issues regarding health, welfare, income security plans, and programs and projects of the DHHS. The DHHS has regional offices that work with the states and communities in carrying out various programs.
Organization of dhhs
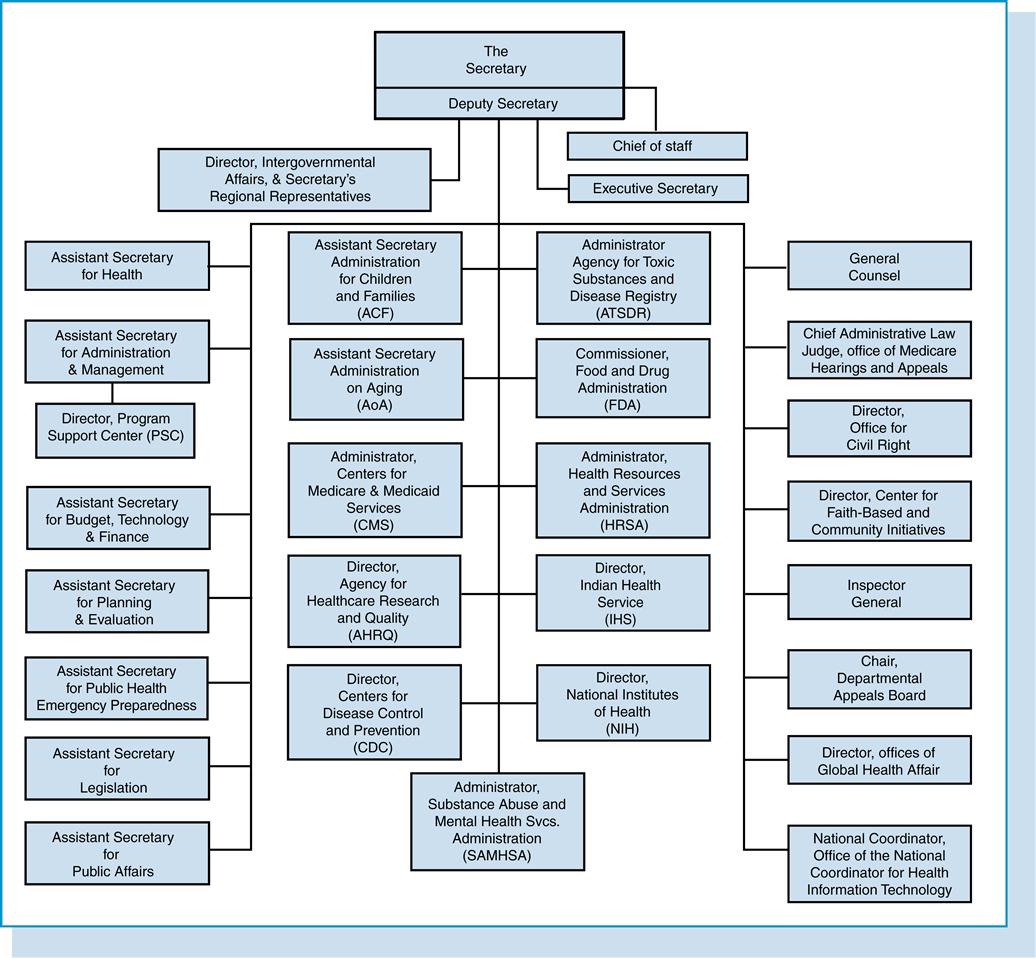
The organizational structure of the DHHS encompasses various agencies, centers, and offices, some of which are discussed in the following section and identified in the DHHS organizational chart illustrated in Figure 1-1.
Office of inspector general
The responsibility of conducting and monitoring audits, inspections, and investigations regarding programs or projects sponsored by the DHHS is delegated to the Office of Inspector General (OIG). For example, this office investigates cases of alleged fraud and abuse that occur in Medicare and Medicaid programs and recommends corrective action in such cases.
Administration for children and families
The Administration for Children and Families is committed to the development of children, youth, and families and to supporting activities that improve and enrich these groups. This agency administers and funds state grants regarding such issues as adoption, runaway and homeless youth, prevention and treatment of child abuse, and child welfare services.
Administration on aging
The Administration on Aging (AoA) was created in response to the Amendment to the Older American Act of 1965. It supports a range of programs that offer services and opportunities for older Americans. The AoA is an advocate for older persons; it works to increase awareness of the contribution that older Americans make and alerts the public regarding the needs of older people.
Agency for healthcare research and quality
The Agency for Healthcare Research and Quality (AHRQ) was established by the Omnibus Budget Reconciliation Act of 1989, which placed greater emphasis on health services research. The primary focus is to produce and disseminate scientific and policy-relevant information that improves the quality, reduces the cost, and enhances the effectiveness of health care.
Agency for toxic substances and disease registry
The Agency for Toxic Substances and Disease Registry is committed to protecting both workers and the public from exposure to and the adverse effects of hazardous substances. The agency, among other functions, collects, analyzes, and disseminates information regarding mortality rates, disease, and hazardous substances; establishes registries for long-term follow-up; and develops programs for public response to health emergencies.
Centers for disease control and prevention
The Centers for Disease Control and Prevention (CDC) is concerned with communicable diseases, environmental health, and foreign quarantine activities. The CDC also works with state and local agencies regarding these matters and provides consultation, education, and training. For example, the CDC has established recommendations (standards) called “Universal Precautions” that are guidelines for health care workers to minimize the spread of infectious substances.
Food and drug administration
The Food and Drug Administration (FDA) is responsible for the safety of foods, drugs, medical devices, cosmetics, and radiation-emitting equipment. Responsibilities include proper labeling, product information, safety, and efficacy.
Substance abuse and mental health services administration
The Substance Abuse and Mental Health Services Administration is concerned with the effective prevention and treatment of addictive and mental disorders. The administration emphasizes state-of-the-art practice that is based on science, high quality, and access to health care for these disorders.
Health resources and services administration
The Health Resources and Services Administration (HRSA) is primarily involved in the distribution of major grant funding to state governments and the private sector.
National institutes of health
The National Institutes of Health (NIH) is a major medical research center composed of numerous institutes and centers (e.g., National Institute on Aging, National Center for Nursing Research, National Cancer Institute). It is a major source of funding for health-related research (e.g., aging, cancer, women’s health issues, obesity, nutrition).
Surgeon general
The surgeon general reports to the assistant secretary for health and is appointed by the president of the United States to serve a 4-year term. The primary role of the surgeon general is to provide leadership and management for the Public Health Service (PHS) Commissioned Corps and to serve as advisor on public health and scientific issues, including current and long-term health issues, emergency preparedness and response, protection and enhancement of the health of the nation, and provision of leadership on health initiatives such as prevention of spread of infectious diseases and tobacco cessation.18
Indian health service
The Indian Health Service (IHS) is responsible for providing health care through a network of hospitals, health centers, health stations, and school health centers and through contracts with private providers to eligible Native Americans.
Centers for medicare and medicaid services
The Centers for Medicare and Medicaid Services (CMS), formerly Health Care Financing Administration (HCFA), is responsible for the Medicare program and the federal government’s role in the Medicaid programs, with special emphasis on quality and utilization control. Through its programs, CMS is involved in the health care of the elderly, disabled, and poor.
The CMS establishes rules and regulations that govern the Medicare program. To be eligible for Medicare and Medicaid reimbursement, providers must demonstrate compliance with the Conditions of Participation (COP), which were originally published in Regulation Number 5, Federal Health Insurance for the Aged. Revisions to the COP are published in the Federal Register. Compliance with the COP is regulated by the states. The review of HCOs to determine compliance with the COP is the responsibility of the states. However, Title XVIII, the Medicare Act, specifies that the facilities accredited by The Joint Commission and American Osteopathic Association (AOA) be deemed in compliance with the Medicare Conditions of Participation for Hospitals7; those accredited are said to have deemed status, which means that the accredited facility meets the requirements for Medicare Conditions of Participation.
Meeting the requirements of the COP is referred to as being certified. However, the term certification is also used to refer to the process by which government and nongovernment organizations evaluate educational programs, health care facilities, and individuals as having met predetermined standards. To ensure high-quality care, the CMS established a national network of Quality Improvement Organizations (QIOs) for each U.S. state and territory and for the District of Columbia. The QIOs work with health care providers and consumers to promote a high quality of care and to investigate complaints about care. The QIOs, discussed in further detail in Chapter 12, also work to protect the Medicare trust fund and ensure that payments are made for only medically necessary services.

Social security administration
Before 1995, the Social Security Administration (SSA) was located within the organizational structure of the DHHS. However, in 1995 it became an independent agency. The Social Security Administration manages the social security program for elderly, disabled, and blind people and for survivors (dependents). The social security program is financed by contributions from employees, employers, and self-employed people, which are placed in a fund. When earnings stop or are reduced because of retirement, death, or disability, the fund pays monthly cash amounts to supplement the loss of income.
Occupational safety and health administration
In 1970, Congress passed the Occupational Safety and Health Act, which mandated that employers provide a safe and healthy work environment. The Occupational Safety and Health Administration (OSHA) is responsible for developing standards and regulations and conducting inspections and investigations to determine compliance, and it proposes corrective actions for noncompliance in matters related to occupational safety and health. Other agencies involved in establishing standards for occupational safety and health include government agencies, such as the CDC, and professional organizations, such as the ACS. The guidelines, recommendations, and standards are directed at protecting employees from occupational health hazards, such as minimizing the risk of contracting disease from asbestos in old buildings, contracting acquired immunodeficiency syndrome (AIDS) in health care facilities, and developing repetitive motion injuries such as carpal tunnel syndrome.
The role of states
State governments have regulatory involvement in the health care systems through state-owned and state-operated facilities, the funding of medical education and teaching hospitals, the certification of health care facilities according to the Medicare COP, maintenance of public health departments, and licensing of health care facilities and health occupations. Hospital ownership, medical education, certification, and licensing of health occupations are discussed in other sections; therefore, only the states’ roles in public health departments and in licensing health care facilities are addressed in this section.
State health departments
The organization of state health departments varies from state to state but is a joint venture between the state and the local communities. The health care provided is usually directed toward maternal and child health care, communicable diseases, and chronic diseases. The maternal and childcare services usually provide obstetric care, family planning, well-baby checkups, vaccinations, and other services. Health care for communicable diseases involves teaching the patient and community about transmission and prevention of certain diseases, diagnosing and treating communicable diseases such as measles and gonorrhea, and tracking the source of the communicable disease. Some of the chronic diseases that the public health department might manage are mental illness, substance abuse, hypertension, and diabetes. HIM professionals need to be knowledgeable about the organization of the state health department in the state where they reside or practice; information is usually available through the county health department.
State and local health departments have important roles in collecting information through vital statistics and communicable disease reporting, in ensuring safe drinking water and environment, and in bioterrorism.

Public health is a general term that refers to a wide array of activities directed at promoting the health of populations. Activities include efforts directed at prevention and early detection of disease and promotion of health in the general and in special populations. Many of the programs and activities are conducted by the states and funded by state and federal monies. The programs and activities include, among other activities, immunizations, behavior modification through education, health screenings and periodic examinations, and therapeutic interventions. For example, to reduce tobacco use, numerous state and federal initiatives are directed at educating the public about the risk of tobacco use, advice about how to quit, funding for counseling and advising patients on smoking cessation, and a hotline for consumers desiring to quit.
Licensure of health care facilities
Licensure gives legal approval for a facility to operate or for a person to practice within his or her profession (Table 1-1). Virtually every state requires that hospitals, nursing homes, and pharmacies be licensed to operate, although the requirements and standards for licensure may differ from state to state. State licensure is mandatory. Federal facilities such as those of the Department of Veterans Affairs do not require state licensure.
Table 1-1
REGULATION OF HEALTH CARE PROVIDERS
| State Government | National Nongovernmental | |
| Health care professionals | Licensure | Registration/certification |
| Health care facilities | Licensure | Accreditation |
Although licensure requirements vary, health care facilities must meet certain basic criteria that are determined by state regulatory agencies. The standards address such concerns as adequacy of staffing, personnel employed to provide services, physical aspects of the facility (equipment, buildings), and services provided, including health records. Survey for licensure is typically performed annually, and the standards are usually considered to be minimally acceptable for operation. Some states also accept Joint Commission Accreditation as proof of meeting licensure requirements.
Legislation
Following is a brief discussion of selected legislation that has had a major impact on health care delivery in the United States.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) of 1985 was written out of a concern for the management of indigent patients. COBRA established the Emergency Medical Treatment and Labor Act (EMTALA), which is known as the “Patient Antidumping Law.” EMTALA established criteria for Medicare-certified facilities and physicians responsible for the transfer and discharge of patients. The law requires that every patient, regardless of ability to pay, who arrives at an emergency department with an emergency medical condition, including active labor, be provided a medical screening examination and stabilizing medical care. If the facility is unable to provide stabilizing treatment or if the patient requests, a transfer to an appropriate facility should be made.19
In 1989, the Omnibus Budget Reconciliation Act was passed, which emphasizes the production and dissemination of scientific and policy-relevant information that improves the quality, reduces the cost, and enhances the effectiveness of health care. This act promoted the development of outcome measures (criteria) for health care quality.
The Patient Self Determination Act of 1990 was a result of the Supreme Court’s ruling in Cruzan v. Missouri (1990) that upheld patient wishes, although the decision meant inevitable death for the patient. The act is intended to increase the public’s awareness of the respective state laws governing patient options for health care, patient rights, and advance directives. An advance directive is a legal, written document that specifies patient preferences regarding future health care or specifies another person to make medical decisions in the event the patient has an incurable or irreversible condition and is unable to communicate his or her wishes; the patient must be competent at the time the document is prepared and signed. The advance directive guides the health care team in making decisions about life-sustaining treatment and organ donation and usually designates a person to assume authority for the patient. The statute requires providers to develop written policies and procedures on self-determination and to document in each health record regardless of whether an advance directive has been signed.12 The HIM or risk management department is responsible for ensuring that the proper documentation is in each health record. (See Chapter 14, Privacy and Health Law, for further information.)
Today, some medical conditions can be extremely costly to treat, and that cost represents a major expense to the business community, insurance companies, managed-care organizations (MCOs), and other health care payers. The result has been the dropping of coverage of high-cost patients or even dropping of the businesses that employ them by these major payers. The individual is then unable to secure health insurance and incurs health care costs that are financially devastating. As a result, in 1996 Congress passed the Health Insurance Portability and Accountability Act (HIPAA), which is a comprehensive law dealing with a variety of health care issues mainly directed at improving access, affordability, and adequacy of health insurance.20
One of the main provisions of HIPAA is to provide for the portability of group health insurance when a person changes employers. Before the enactment of HIPAA, employees often had to wait for coverage themselves or for one of their dependents because of preexisting conditions such as asthma or high blood pressure. This potential loss of health insurance coverage kept individuals from changing jobs and advancing in their careers. HIPAA allowed for continuous coverage when a person changed from one group insurance plan to another. The act also established tax breaks for purchasers of long-term care insurance and self-employed purchasers of health insurance and created a fraud and abuse program for health plans.20
HIPAA includes many other provisions that affects the operation of HCOs. Some that have had the greatest affect on HIM can be found in the administrative simplification section. The Privacy and Security Rules are included in this section. The Privacy Rule applies to protected health information in any format created or used by health care providers, health care plans, and health care clearinghouses. The HIPAA security rule is concerned with the protection of the electronic health information. The advent of HIPAA has brought about expanded roles and responsibilities for HIM professionals—that is, protecting privacy and maintaining the security of electronic health care transactions and records. The federal regulations standardize the privacy and security practices in the health care industry throughout the United Stated. Before HIPAA, laws differed among states. Privacy is discussed in further detail in Chapters 14 and 15 and security in Chapter 7.

Accreditation
The process by which a private nongovernmental organization or agency performs an external review and grants recognition to a program of study or institution that meets certain predetermined standards is called accreditation. The review process and the standards are devised and regulated by professional organizations such as The Joint Commission and the AOA. Although the process is voluntary, there are financial and legal incentives for HCOs to attain accreditation. Advantages of accreditation are numerous and include the following:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


