| HLA-identical living donor | 88% | 73% |
| Other living donor | 74% | 56% |
| HLA-matched cadaver | 70% | 56% |
Case 2 | Polycystic Kidneys
Frequency in Survey:
main focus of a short case or additional feature in 14% of attempts at PACES Station 1, Abdominal.
Record
There are bilateral masses in the flanks which are bimanually ballotable. I can get above them and the percussion note is resonant over them.* I suspect, therefore, that they are renal masses and a likely diagnosis is polycystic kidneys (?uraemic facies; the blood pressure may be raised). The arteriovenous fistula/shunt on his arm indicates that the patient is being treated with haemodialysis (about 50% develop renal failure†).
Other causes of bilateral renal enlargement include:
1 Bilateral hydronephrosis
2 Amyloidosis (?underlying chronic disease, hepatosplenomegaly, etc; see Station 1, Abdominal, Case 4)
3 Tuberous sclerosis (?adenoma sebaceum; see Vol. 3, Station 5, Skin, Case 9)
4 Von Hippel–Lindau disease.
‡
Polycystic disease of the liver in adults may cause a nodular liver enlargement (liver function may be normal despite massive hepatomegaly). About 50% have renal involvement. Cystic liver is a major feature of autosomal recessive polycystic kidney disease (ARPKD, previously called infantile polycystic disease), but a minor feature of autosomal dominant polycystic kidney disease (ADPKD, previously called adult polycystic disease).
Other Features of ADPKD
Cysts may also occur in other organs – most important are saccular aneurysms (berry aneurysms) of the cerebral arteries
§ which, in combination with the hypertension, leads to serious risk of intracranial haemorrhage (cause of death in 10% of cases according to some authorities). There may be focal defects
Mitral valve prolapse (see Station 3, Cardiovascular, Case 10) may occur in 25% as a further manifestation of the systemic collagen defect. Patients often have palpitations and atypical chest pain. Other valvular abnormalities are also more common and echocardiography should be undertaken if a murmur is detected
It may present with flank pains, bleeding, urinary tract infection, nephrolithiasis, obstructive uropathy or obstruction of the surrounding structures
Renal cell carcinoma is not more common than in the general population, but it can be difficult to diagnose – CT and MRI may be useful
Presymptomatic screening by USS criteria and gene identification
† is deferred to 20 years of age as it is not conclusive before this. The exceptions to this are if there is a family history of aneurysm or if hypertension or other signs of renal disease are present
Case 3 | Chronic Liver Disease
Frequency in Survey:
main focus of a short case or additional feature in 12% of attempts at PACES Station 1, Abdominal.
Record
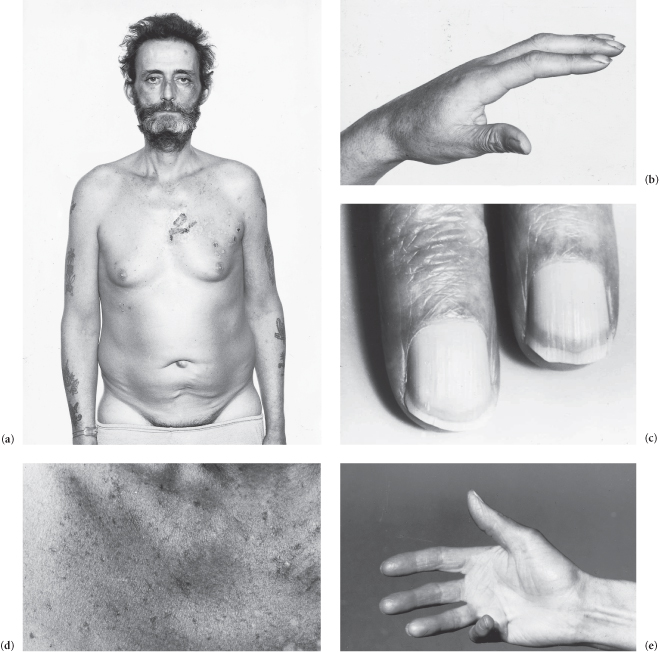
The patient is icteric, pigmented and (rarely) cyanosed (due to pulmonary venous shunts). He has clubbing, leuconychia, palmar erythema, Dupuytren’s contracture * and there are several spider naevi. He has a flapping tremor of the hands (suggesting some portosystemic encephalopathy). There are scratch marks on the forearms and back, and there is purpura. There is gynaecomastia, scanty body hair and his testes are small. There is 5 cm hepatomegaly and 3 cm splenomegaly. He has ascites and ankle oedema, and there are distended abdominal veins in which the flow is away from the umbilicus.
The diagnosis is likely to be cirrhosis of the liver with portal hypertension.
Possible Causes
1 Alcohol
2 Viral hepatitis:
(a) hepatitis B (?health or clinical laboratory worker, IV drug abuser, risky sexual practices)
(b) hepatitis C
† (the major cause of posttransfusion hepatitis; also transmitted between IV drug users)
(c) hepatitis D (unusual; the D virus requires the presence of hepatitis B virus (HBV) for its replication and expression)
3 Autoimmune chronic active hepatitis (pubertal or menopausal female, steroid responsive; associated with diabetes, inflammatory bowel disease, thyroiditis and pulmonary infiltrates; ?smooth muscle antibodies)
4 Primary biliary cirrhosis (middle-aged female, scratch marks, xanthelasma; ?antimitochondrial antibody; see Station 1, Abdominal, Case 17)
5 Haemochromatosis (male, slate-grey pigmentation; see Station 1, Abdominal, Case 16)
6 Non-alcoholic fatty liver disease (NAFLD), (?obesity, diabetes mellitus, hypertension, hyperlipidaemia)
*
7 Cryptogenic
Other Causes
Cardiac failure (?JVP ↑, v waves, S3 or a valvular lesion, tender pulsatile liver if tricuspid incompetence)
Constrictive pericarditis
† (JVP raised, abrupt
x and
y descent, loud early
S3 (‘pericardial knock’ – a valuable sign but only present in <40% of cases) though heart sounds often normal, slight ‘paradoxical pulse’,
no signs in lung fields, chest X-ray may show calcified pericardium; rare but important cause of ascites as response to treatment may be dramatic)
Budd–Chiari syndrome (in the acute phase ascites develops rapidly with pain, there are no cutaneous signs of chronic liver disease and the liver is smoothly enlarged and tender; if the inferior vena cava is involved there is no hepatojugular reflux)
Biliary cholestasis (bile obstruction with or without infection), which leads to secondary biliary cirrhosis
Toxins and drugs (methotrexate, methyldopa, isoniazid, carbon tetrachloride, amiodarone, aspirin, phenytoin, propylthiouracil, sulphonamides)
Wilson’s disease (?Kayser–Fleischer rings, tremor, rigidity, dysarthria)
α1-Antitrypsin deficiency (?lower zone emphysema)
Other metabolic causes (galactosaemia, tyrosinaemia, type IV glycogenolysis)
Case 4 | Hepatosplenomegaly
Frequency in Survey:
main focus of a short case or additional feature in 12% of attempts at PACES Station 1, Abdominal.
Record
There is hepatosplenomegaly, the spleen is enlarged … cm below the left costal margin. The liver is palpable at … cm below the right costal margin; it is non-tender, firm and smooth (now look for clinical anaemia, lymphadenopathy and signs of chronic liver disease).
Likely causes to be considered are:
No Other Signs or Clinical Anaemia Only
1 Myeloproliferative disorders (see Station 1, Abdominal, Case 6)
2 Lymphoproliferative disorders (see Station 1, Abdominal, Case 6)
3 Cirrhosis of the liver with portal hypertension
* (less likely if there are no other signs of chronic liver disease)
Hepatosplenomegaly Plus Palpable Lymph Nodes†
1 Chronic lymphatic leukaemia
2 Lymphoma
Other conditions to be considered include infectious mononucleosis (?throat), infective hepatitis (?icterus), sarcoidosis and secondary syphilis.
Signs of Chronic Liver Disease
1 Cirrhosis of the liver with portal hypertension (see Station 1, Abdominal, Case 3)
2 Chronic autoimmune liver disease (can occur before cirrhosis develops)
Other Causes of Hepatosplenomegaly
Acute viral hepatitis A, B or C or E
‡ (?icterus, tattoo marks, needle marks, foreign travel)
Brucellosis (‘Examine this farmer’s abdomen’)
Weil’s disease (?icterus, sewerage worker or fell into canal)
Toxoplasmosis (glandular fever-like illness)
Cytomegalovirus infection (glandular fever-like illness)
Pernicious anaemia and other megaloblastic anaemias (NB: SACD; see Station 3, CNS, Case 37. NB: associated organ-specific autoimmune disease; see Vol. 3, Station 5, Skin, Case 8)
Storage disorders (e.g. Gaucher’s – spleen is often huge; glycogen storage disease)
Amyloidosis (?underlying chronic disease)
§Other causes of portal hypertension (e.g. Budd–Chiari syndrome = hepatic vein thrombosis; see Station 1, Abdominal, Cases 3 and 7)
Infantile polycystic disease (in some variants of this, children have relatively mild renal involvement but hepatosplenomegaly and portal hypertension; they rarely survive to adulthood)
Common Causes on a Worldwide Basis
Malaria
Kala-azar
Schistosomiasis
Tuberculosis
Case 5 | Hepatomegaly (Without Splenomegaly)
Frequency in Survey:
main focus of a short case or additional feature in 10% of attempts at PACES Station 1, Abdominal.
Record
The liver is palpable at … cm below the right costal margin (?icterus, ascites, signs of cirrhosis (do not miss gynaecomastia), pigmentation, lymph nodes).
Common Causes
Cirrhosis – usually alcoholic (?spider naevi, gynaecomastia, etc; see Station 1, Abdominal, Case 3)
Secondary carcinoma (?hard and knobbly, cachexia, evidence of primary)
Congestive cardiac failure (?JVP ↑, ankle oedema, S3 or cardiac murmur; tender pulsatile liver with giant v waves in the JVP in tricuspid incompetence)
Other Causes of Hepatomegaly
Infections such as glandular fever, Weil’s disease and acute viral hepatitis (e.g. A,B,E) (remember hepatitis serology heads list of investigations in icterus of uncertain cause)
Primary tumours, both malignant (hepatoma may complicate cirrhosis) and benign (liver cell adenoma is associated with oral contraceptive use)
Lymphoproliferative disorders (?lymph nodes)
Primary biliary cirrhosis (?middle-aged female, scratch marks, xanthelasma, etc; see Station 1, Abdominal, Case 17)
Haemochromatosis (?male, slate-grey pigmentation, etc; see Station 1, Abdominal, Case 16)
Hepatic steatosis (alcohol, NAFLD; see Station 1, Abdominal, Case 3)
Sarcoidosis (?erythema nodosum or history of, lupus pernio, chest signs)
Amyloidosis (?rheumatoid arthritis or other underlying chronic disease; see Footnote, Station 1, Abdominal, Case 4)
Hydatid cyst (?Welsh connection – NB: patient’s name)
Amoebic abscess (?tropical connection – name, appearance)
Budd–Chiari syndrome (?icterus, ascites, tender hepatomegaly)
Riedel’s lobe (5th liver lobe – anatomical variant)
Emphysema (apparent hepatomegaly)
Hard and Knobbly Hepatomegaly – Possible Causes
Malignancy – primary or secondary
Polycystic liver disease (?kidneys; see Station 1, Abdominal, Case 2)
Macronodular cirrhosis (following hepatitis B with widespread necrosis)
Hydatid cysts (may be eosinophilia; rupture may be associated with anaphylaxis)
Syphilitic gummas (late benign syphilis; there is usually hepatosplenomegaly and anaemia; rapid response to penicillin)
Case 6 | Splenomegaly (Without Hepatomegaly)
Frequency in Survey:
main focus of a short case or additional feature in 9% of attempts at PACES Station 1, Abdominal.
Record
The spleen is palpable at … cm.
or
There is a mass in the left hypochondrium. On palpation I cannot get above the mass, it has a notch, and on inspiration moves diagonally across the abdomen. The percussion note is dull over the left lower lateral chest wall and over the mass.
I think this is the spleen enlarged at … cm. Likely causes* to be considered are:
Very Large Spleen†
1 Chronic myeloid leukaemia (Philadelphia (Ph) chromosome positive in 90%
‡)
2 Myelofibrosis
and in other parts of the world
3 Chronic malaria
4 Kala-azar
Spleen Enlarged 4–8 cm (2–4 Finger Breadths)
1 Myeloproliferative disorders
§ (e.g. CML and myelofibrosis)
2 Lymphoproliferative disorders
* (e.g. lymphoma and chronic lymphatic leukaemia)
3 Cirrhosis of the liver with portal hypertension (spider naevi, icterus, etc; see Station 1, Abdominal, Case 3)
Spleen Just Tipped or Enlarged 2–4 cm (1–2 Finger Breadths)
1 Myeloproliferative disorders
†
2 Lymphoproliferative disorders
* (?palpable lymph nodes)
3 Cirrhosis of the liver and other causes of portal hypertension (e.g. congenital hepatic fibrosis, portal vein thrombosis)
4 Infections such as:
(a) glandular fever (?throat, lymph nodes)
(b) infectious hepatitis (?icterus)
(c) subacute bacterial endocarditis (?heart murmur, splinter haemorrhages, etc.)
Other Causes of Splenomegaly
Polycythaemia rubra vera (?plethoric, middle-aged man)
Brucellosis (‘Examine this farmer’s abdomen’)
Sarcoidosis (?erythema nodosum or history of; lupus pernio; chest signs)
Haemolytic anaemia (?icterus)
Pernicious anaemia and other megaloblastic anaemias (?pallor; NB: SACD; see Station 3, CNS, Case 37; NB: associated organ-specific autoimmune diseases, especially autoimmune thyroid disease, diabetes, Addison’s, vitiligo, hypoparathyroidism; see Vol. 3, Station 5, Skin, Case 8)
Idiopathic thrombocytopenic purpura (?young female, purpura)
Paroxysmal nocturnal haemoglobinuria (rare 3rd–4th decade, caused by an acquired defect in the cell membrane)
Felty’s syndrome (?hands, nodules)
Amyloidosis (?underlying chronic disease, other organ involvement; see Station 1, Abdominal, Case 4)
SLE (?typical rash)
Lipid storage disease (spleen may be enormous, e.g. Gaucher’s)
Myelomatosis
Chronic iron deficiency anaemia
Thyrotoxicosis
Other infections (subacute septicaemia, typhoid, disseminated TB, trypanosomiasis, echinococcosis)
Other causes of congestive splenomegaly
* (hepatic vein thrombosis, portal vein obstruction, schistosomiasis, congestive heart failure)
Case 7 | Ascites
Frequency in Survey:
main focus of a short case or additional feature in 6% of attempts at PACES Station 1, Abdominal.
Survey Note:
occurred in the examination: (i) as part of cirrhosis; (ii) on its own without a clearly defined underlying cause, in which case it was the main focus and possible causes were often discussed; and (iii) in association with an obvious mass or the irregular liver of malignancy.
Record
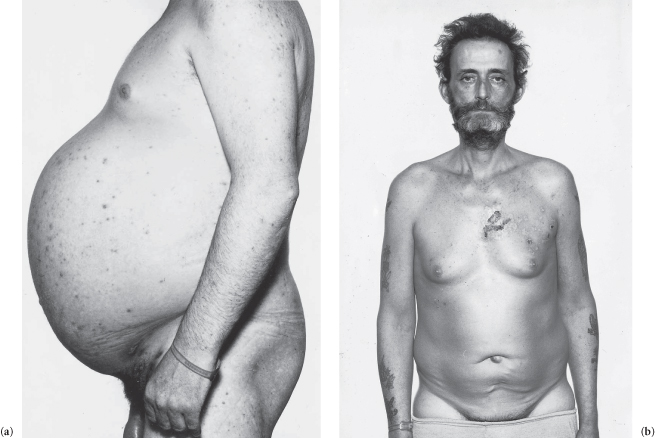
There is generalized swelling of the abdomen and the umbilicus is everted. * The flanks are stony dull to percussion but the centre is resonant (floating, gas-filled bowel). The dullness is shifting and a fluid thrill can be demonstrated (only in tense, large ascites).
This is ascites.
Usual Causes
1 Cirrhosis with portal hypertension (?hepatomegaly, icterus, spider naevi, leuconychia, etc; see Station 1, Abdominal, Case 3); treatment consists of salt restriction, diuretic therapy (spironolactone or amiloride); paracentesis is increasingly used as initial treatment
2 Intraabdominal malignancy (especially ovarian and gastrointestinal – ?hard knobbly liver, mass, cachexia, nodes, e.g. Troisier’s sign also called Virchow’s node)
3 Congestive cardiac failue (?JVP ↑, ankle and sacral oedema, hepatomegaly (pulsatile if tricuspid incompetence), large heart, tachycardia, S3 or signs of the cardiac lesion)
Other Causes
Nephrotic syndrome (?young, underlying diabetes (fundi), evidence of chronic disease underlying amyloid, evidence of collagen disease, etc; see Station 1, Abdominal, Case 20)
Other causes of hypoalbuminaemia (e.g. malabsorption)
Tuberculous peritonitis
† (?ethnic origin, chest signs)
Constrictive pericarditis (JVP raised, abrupt x and y descent, loud early S3 (‘pericardial knock’), though heart sounds often normal, slight ‘paradoxical’ pulse, no signs in lung fields; chest X-ray may show calcified pericardium; rare but important as response to treatment may be dramatic)
Budd–Chiari syndrome (ascites develops rapidly with pain, icterus but no signs of chronic liver disease, smoothly enlarged tender liver; causes include tumour infiltration, oral contraceptives, polycythaemia rubra vera, ulcerative colitis and severe dehydration)
Myxoedema (?facies, ankle jerks, etc; very rare)
Meigs’ syndrome (ovarian fibroma; important as easily correctable by surgery)
Pancreatic ascites (complication of acute pancreatitis)
Chylous ascites (due to lymphatic obstruction; milky fluid)
Case 8 | Abdominal Mass
Frequency in Survey:
main focus of a short case or additional feature in 3% of attempts at PACES Station 1, Abdominal.
Survey Note:
discussion usually concerned differentiation from/of enlarged organs (spleen, kidney, liver) or differential diagnosis.
Record 1
In this young (?somewhat pale-looking) adult patient there is a freely mobile 5 × 4 cm (measure) firm tender mass in the right iliac fossa. None of the abdominal organs is enlarged, and there are no fistulae.
The diagnosis could be Crohn’s disease (Station 1, Abdominal, Case 9).
Other Causes of a Mass in the Right Iliac Fossa
1 Ileocaecal tuberculosis (?ethnic origin, chest signs)
2 Carcinoma of the caecum (?older person, non-tender and hard mass, lymph nodes; investigate with colonoscopy)
3 Amoebic abscess (?travelled abroad)
4 Lymphoma (?hepatosplenomegaly, lymph nodes elsewhere; investigate with CT scan)
5 Appendicular abscess (investigate with USS)
6 Neoplasm of the ovary (investigate with USS/CT scan)
7 Ileal carcinoid (rare)
8 Transplanted kidney
9 Faecal matter in caecum (especially in constipation)
Record 2
A mobile tender 6 × 5 cm mass is palpable in the left iliac fossa in this elderly patient. None of the other organs is palpable.
It is probably a diverticular abscess (usually tender; investigate with USS/CT scan).
Other Causes of a Mass in the Left Iliac Fossa
1 Carcinoma of the colon (?non-tender, hepatomegaly; investigate with colonoscopy)
2 Neoplasm of the left ovary (investigate with USS/CT scan)
3 A faecal mass (no other signs)
4 Amoebic abscess
Record 3
In this thin and pale patient there is a round, hard 8 × 6 cm non-tender mass with ill-defined edges in the epigastrium. It does not move with respiration. Neither the liver nor the spleen is enlarged (check neck for lymph nodes).
The probable diagnosis is a neoplasm such as:
1 Carcinoma of the stomach (?Troisier’s sign also called Virchow’s node; investigate with upper GI endoscopy)
2 Carcinoma of the pancreas (?icterus; NB: Courvoisier’s sign; investigate with CT scan)
3 Lymphoma (?generalized lymphadenopathy, spleen; investigate with CT scan).
Record 4
In this elderly patient there is a pulsatile (pulsating anteriorly as well as transversely), 6 × 4 cm firm mass* palpable 2 cm above the umbilicus and reaching the epigastrium. Both femoral pulses are palpable just before the radials (no evidence of dissection) and there are no bruits heard either over the mass or over the femorals. (Look for evidence of peripheral vascular insufficiency in the feet.)
This patient has an aneurysm of his abdominal aorta (the most common cause is arteriosclerosis†).
If you find a mass in either upper quadrant you should define:
Its size
Its shape
Its consistency
Whether you can get above it
Whether it is bimanually ballotable
Whether it moves with respiration
Whether it is tender.
In either upper quadrant it has to be differentiated from a renal mass (see Station 1, Abdominal, Case 2); if in the left hypochondrium, it has to be differentiated from a spleen (see Station 1, Abdominal, Case 6) and in the right hypochondrium from a liver (see Station 1, Abdominal, Case 5). Other causes of an upper quadrant mass include:
Carcinoma of the colon
Retroperitoneal sarcoma
Lymphoma (?generalized lymphadenopathy, spleen)
Diverticular abscess (?tender).
Case 9 | Crohn’s Disease
Frequency in Survey:
main focus of a short case or additional feature in 3% of attempts at PACES Station 1, Abdominal.
Survey Note:
there were several different presentations: as a right iliac fossa mass, as multiple scars and sinuses on the abdomen, as perianal Crohn’s disease (only one case) and as Crohn’s disease of the lips. In one-third of cases the clue was given that the patient had diarrhoea.
Record 1
The multiple laparotomy scars suggest a chronic, relapsing, abdominal condition which has led to crises requiring surgical intervention on several occasions. In view of the associated fistula formation, Crohn’s disease is likely.
Record 2
The chronically swollen lips (granulomatous infiltration) and history of chronic diarrhoea are suggestive of Crohn’s disease (examine inside the mouth for ulcers which vary in size).
Record 3
There is a (characteristic) dusky blue discoloration of the perianal skin. There are oedematous skin tags (which look soft but are very firm), there is fissuring, ulceration and fistula formation.
The diagnosis is perianal Crohn’s disease (may antedate disease elsewhere in the bowel).
Record 4
Right iliac fossa mass (see Station 1, Abdominal, Case 8).
Other Physical Signs in Crohn’s Disease