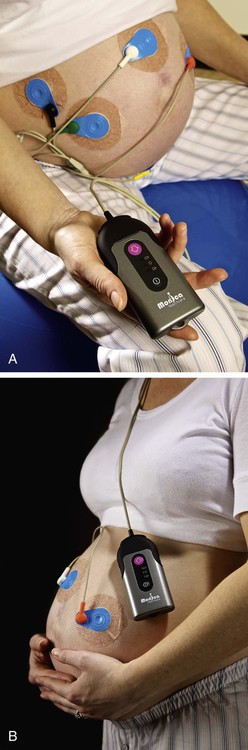
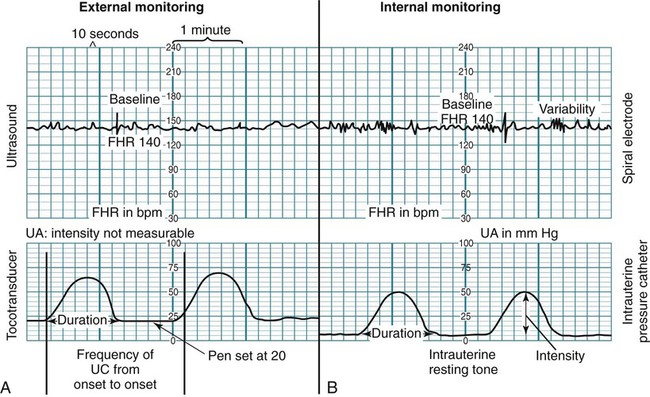
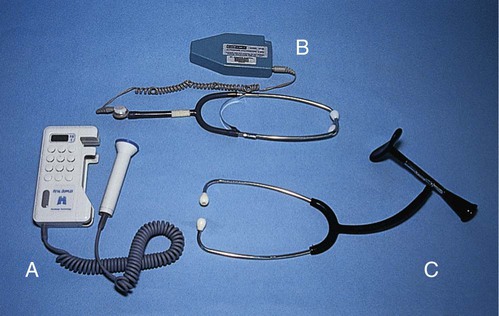
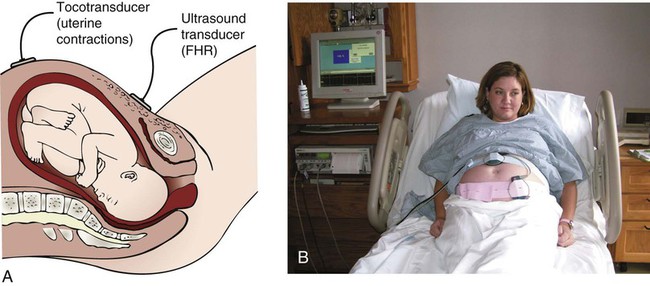
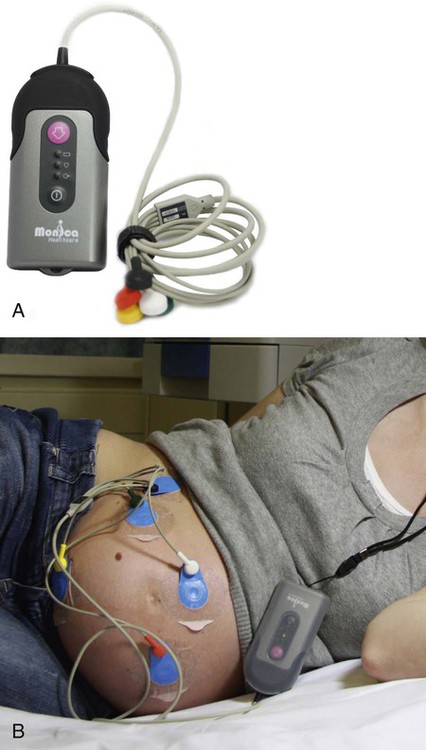
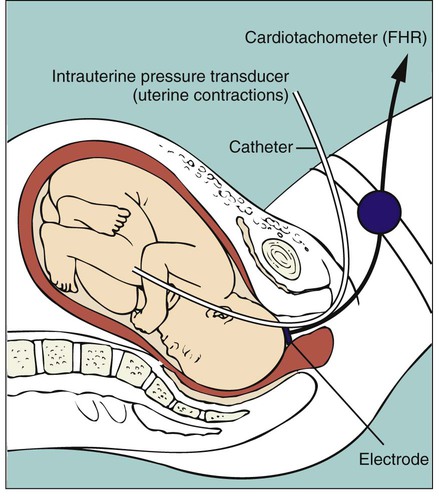
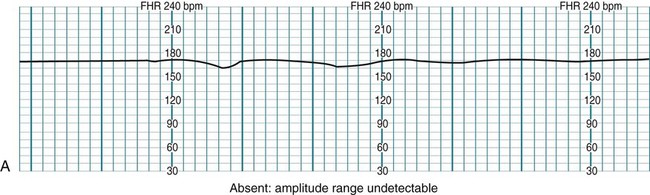
On completion of this chapter, the reader will be able to: • Identify typical signs of normal and abnormal fetal heart rate patterns. • Compare fetal heart rate monitoring performed by intermittent auscultation with external and internal electronic methods. • Explain the baseline fetal heart rate and evaluate periodic changes. • Describe nursing measures that can be used to maintain fetal heart rate patterns within normal limits. • Differentiate among the nursing interventions used for managing specific fetal heart rate patterns, including tachycardia and bradycardia, absent or minimal variability, and late and variable decelerations. • Review the documentation of the monitoring process necessary during labor. The ability to assess the fetus by auscultation of the fetal heart was initially described more than 300 years ago. With the advent of the fetoscope and stethoscope after the turn of the twentieth century, the listener could hear clearly enough to count the fetal heart rate (FHR). When electronic FHR monitoring made its debut for clinical use in the early 1970s, the anticipation was that its use would result in less intrapartum asphyxia and thus fewer cases of cerebral palsy. Consequently the use of electronic fetal monitoring rapidly expanded (Garite, 2012). However, the rate of cerebral palsy has not declined since that time and is not likely to decrease because more preterm infants are surviving (Gilbert, 2011). Prematurity is the leading cause of cerebral palsy. Intrapartum asphyxia accounts for 25% of cases or less of this disorder (Garite, 2012). Still electronic fetal monitoring (EFM) is a useful tool for visualizing FHR patterns on a monitor screen or printed tracing. It continues to be the primary mode of intrapartum fetal assessment in the United States and is the most commonly performed obstetric procedure in that country (ACOG, 2009; Miller, Miller, and Tucker, 2013). Pregnant women should be informed about the equipment and procedures used and the risks, benefits, and limitations of intermittent auscultation (IA) and EFM. This chapter discusses the basis for intrapartum fetal monitoring, the types of monitoring, and nursing assessment and management of abnormal fetal status. • Reduction of blood flow through the maternal vessels as a result of maternal hypertension (chronic hypertension, preeclampsia, or gestational hypertension), hypotension (caused by supine maternal position, hemorrhage, or epidural analgesia or anesthesia), or hypovolemia (caused by hemorrhage) • Reduction of the oxygen content in the maternal blood as a result of hemorrhage or severe anemia • Alterations in fetal circulation, occurring with compression of the umbilical cord (transient, during uterine contractions [UCs], or prolonged, resulting from cord prolapse), partial placental separation or complete abruption, or head compression (head compression causes increased intracranial pressure and vagal nerve stimulation with an accompanying decrease in the FHR) • Reduction in blood flow to the intervillous space in the placenta secondary to uterine hypertonus (generally caused by excessive exogenous oxytocin) or secondary to deterioration of the placental vasculature associated with maternal disorders such as hypertension or diabetes mellitus Fetal well-being during labor can be assessed by the response of the FHR to UCs. A group of fetal monitoring experts recommended that FHR tracings demonstrating certain reassuring characteristics be described as normal (category I) (Box 15-1). Table 15-1 describes normal uterine activity (UA) during labor. TABLE 15-1 NORMAL UTERINE ACTIVITY DURING LABOR Data from Macones GA, Hankins GD, Spong CY, et al: The 2008 National Institute of Child Health and Human Development Workshop Report on Electronic Fetal Monitoring: update on definitions, interpretation, and research guidelines, J Obstet Gynecol Neonatal Nurs 37(5):510–515, 2008; Miller LA, Miller DA, Tucker SM: Mosby’s pocket guide to fetal monitoring: a multidisciplinary approach, ed 7, St Louis, 2013, Mosby. The goals of intrapartum FHR monitoring are to identify and differentiate the normal (reassuring) patterns from the abnormal (nonreassuring) patterns, which can indicate fetal compromise. Although the 2008 National Institute of Child Health and Human Development workshop (Macones, Hankins, Spong, et al., 2008) and the ACOG (2009) both recommend use of the terms normal and abnormal to describe FHR tracings, the terms reassuring and nonreassuring are still frequently used clinically. Abnormal FHR patterns are those associated with fetal hypoxemia, which is a deficiency of oxygen in the arterial blood. If uncorrected, hypoxemia can deteriorate to severe fetal hypoxia, an inadequate supply of oxygen at the cellular level that can cause metabolic acidosis. The term asphyxia is used when fetal hypoxia results in metabolic acidosis (Garite, 2012). See Box 15-1 for examples of abnormal (category III) FHR tracings. The ideal method of fetal assessment during labor continues to be debated. Research findings support the use of both IA of the FHR and EFM (Gilbert, 2011). Although IA is a high-touch, low-technology method of assessing fetal status during labor that places fewer restrictions on maternal activity, more than 85% of laboring women in the United States are monitored electronically for at least part of their labor (ACOG, 2009; Miller, Miller, and Tucker, 2013). The continued use of EFM in place of IA is thought to be because of concerns about liability and the increased nurse-patient ratio required with IA. Because all surveillance methods, including EFM, have limitations, some believe that the evidence supports a return to the use of IA for low risk laboring women (ACOG, 2009; Miller, Miller, and Tucker, 2013). Intermittent auscultation involves listening to fetal heart sounds at periodic intervals to assess the FHR. IA of the fetal heart can be performed with a Pinard stethoscope (Fig. 15-1), Doppler ultrasound (Fig. 15-2, A), an ultrasound stethoscope (see Fig. 15-2, B), or a DeLee-Hillis fetoscope (see Fig. 15-2, C). Doppler ultrasound and ultrasound stethoscopes transmit ultra high–frequency sound waves, reflecting movement of the fetal heart, and convert these sounds into an electronic signal that can be counted. The fetoscope is applied to the listener’s forehead because bone conduction amplifies the fetal heart sounds for counting. Box 15-2 describes how to perform IA. IA is easy to use, inexpensive, and less invasive than EFM. It is often more comfortable for the woman and gives her more freedom of movement. Other care measures such as ambulation and the use of baths or showers are easier to carry out when IA is used. However, it may be difficult to perform transabdominally in women who are obese. A transvaginal fetal Doppler probe is now available. It provides closer proximity to the uterus, making it easier to auscultate the FHR when the woman is obese or early in gestation (Miller, Miller, and Tucker, 2013). Because IA is intermittent, significant events may occur during a time when the FHR is not being auscultated. In addition, IA does not provide a permanent documented visual record of the FHR and cannot be used to assess visual patterns of the FHR variability or periodic changes (Miller, Miller, and Tucker, 2013). By using IA the nurse can assess the baseline FHR, rhythm, and increases and decreases from baseline. The American College of Nurse-Midwives (ACNM) reviewed references from the United States, Great Britain, and Canada regarding the recommended frequency of IA in low risk women and found consistent recommendations for every 15 minutes in the active phase of the first stage of labor and every 5 minutes in the second stage of labor (Miller, Miller, and Tucker, 2013). The ACOG (2009) agrees that these time frames are acceptable for IA in low risk women. The Association of Women’s Health, Obstetric and Neonatal Nurses recommends different IA frequencies: every hour in the latent phase of first-stage labor, every 30 minutes in the active phase of first-stage labor, and every 15 minutes in the second stage of labor (AWHONN, 2009). However, the optimal frequency for IA in low risk women during labor has not been determined (Nageotte and Gilstrap, 2009). When using IA, UA is assessed by palpation. The examiner should keep his or her fingertips placed over the fundus before, during, and after contractions. The contraction intensity is usually described as mild, moderate, or strong. The contraction duration is measured in seconds, from the beginning to the end of the contraction. The frequency of contractions is measured in minutes, from the beginning of one contraction to the beginning of the next. The examiner should keep his or her hand on the fundus after the contraction is over to evaluate uterine resting tone or relaxation between contractions. Resting tone between contractions is usually described as soft or relaxed (AWHONN, 2009). The purpose of EFM is the ongoing assessment of fetal oxygenation. FHR tracings are analyzed for characteristic patterns that suggest fetal hypoxic events and metabolic acidosis during labor. When hypoxia or metabolic acidosis is suspected in labor, interventions to resolve the problem can be implemented in a timely manner before permanent damage or death occurs (Garite, 2012). The two modes of EFM are the external mode, which uses external transducers placed on the maternal abdomen to assess FHR and UA; and the internal mode, which uses a spiral electrode applied to the fetal presenting part to assess the FHR and an intrauterine pressure catheter (IUPC) to assess UA and uterine resting tone. The differences between the external and internal modes of EFM are summarized in Table 15-2. TABLE 15-2 EXTERNAL AND INTERNAL MODES OF MONITORING Separate transducers are used to monitor the FHR and UCs (Fig. 15-3). The ultrasound transducer works by reflecting high-frequency sound waves off a moving interface, in this case the fetal heart and valves. It is sometimes difficult to reproduce a continuous and precise record of the FHR because of artifact introduced by fetal and maternal movement. Maternal obesity, occiput posterior position of the fetus, and anterior attachment of the placenta can cause weak or absent signals (AWHONN, 2009). The FHR is printed on specially formatted monitor paper. The standard paper speed used in the United States is 3 cm/min. Once the area of maximal intensity of the FHR has been located, conductive gel is applied to the surface of the ultrasound transducer, and the transducer is then positioned over this area and held securely in place using an elastic belt (see Critical Thinking Case Study). The tocotransducer (tocodynamometer) measures UA transabdominally. The device is placed over the fundus above the umbilicus and held securely in place with an elastic belt (see Fig. 15-3, B). UCs or fetal movements depress a pressure-sensitive surface on the side next to the abdomen. The tocotransducer can measure and record the frequency and approximate duration of UCs but not their intensity. This method is especially valuable for measuring UA during the first stage of labor in women with intact membranes or for antepartum testing. If the woman is obese, the tocotransducer may be unable to detect the exact frequency and duration of UA. In 2011 an external monitor became available for use in the United States. The Monica AN24 uses abdominally obtained electronic impulses to monitor both FHR and UA (Fig. 15-4, A and B). The monitor uses five electrodes placed on the woman’s abdomen to directly monitor the electrocardiogram from the maternal and fetal hearts and the electromyogram from the uterine muscle. This information is transmitted wirelessly, via Bluetooth technology, to an interface device that allows the FHR and UA data to print or display on a standard fetal monitor (Miller, Miller, and Tucker, 2013). The Monica AN24 eliminates much of the problem caused by signal loss resulting from maternal or fetal movement or maternal obesity that often occurs with traditional external monitors. The monitor also more accurately measures the frequency, occurrence of peak, and duration of UCs than does the traditional tocotransducer, although it does not provide actual intensity measurement in millimeters of mercury (mm Hg) as an IUPC does. Other advantages of the Monica AN24 are that it eliminates the need for abdominal belts and frequent readjustment of the tocotransducer and ultrasound transducer and provides some patient mobility. The woman may move up to 50 feet away from the interface device without signal loss (Fig. 15-5, A and B). In the United States the Monica AN24 is only approved for use in pregnancies that have reached 36 completed weeks or more of gestation (Miller, Miller, and Tucker, 2013). The Monica AN24 monitor may not be readily available for use in all labor and birth settings. The technique of continuous internal FHR or UA monitoring provides a more accurate appraisal of fetal well-being during labor than external monitoring because it is not interrupted by fetal or maternal movement or affected by maternal size (Fig. 15-6). For this type of monitoring the membranes must be ruptured, the cervix sufficiently dilated (at least 2 to 3 cm), and the presenting part low enough to allow placement of the spiral electrode or IUPC or both. Internal and external modes of monitoring may be combined (i.e., internal FHR with external UA or external FHR with internal UA) without difficulty. Because it can measure the intensity of individual UCs precisely, the IUPC can be used to evaluate the adequacy of UA for achieving progress in labor. Montevideo units (MVUs) are calculated by subtracting the baseline uterine pressure from the peak contraction pressure for each contraction that occurs in a 10-minute window and then adding together the pressures generated by each contraction that occurs during that period of time. Spontaneous labor usually begins when MVUs are between 80 and 120. Uterine activity during the first stage of normal labor rarely exceeds 250 MVUs (see Table 15-1) (Cunningham, Leveno, Bloom, et al., 2010; Miller, Miller, and Tucker, 2013). The FHR and UA are displayed on the monitor paper or computer screen, with the FHR in the upper section and UA in the lower section. Fig. 15-7 contrasts the internal and external modes of electronic monitoring. Note that each small square on the monitor paper or screen represents 10 seconds; each larger box of six squares equals 1 minute (when paper is moving through the monitor at the rate of 3 cm/min). Characteristic FHR patterns are associated with fetal and maternal physiologic processes and have been identified for many years. However, because EFM was introduced into clinical practice before consensus was reached regarding standardized terminology, variations in the description and interpretation of common FHR patterns were often great. In 1997 the National Institute of Child Health and Human Development (NICHD) published a proposed nomenclature system for EFM interpretation with standardized definitions for FHR monitoring. However, the NICHD recommendations were not widely incorporated into clinical practice until they were endorsed by the ACOG in 2005. Shortly thereafter use of the NICHD standard terminology was also endorsed by the AWHONN and the ACNM (Miller, Miller, and Tucker, 2013). All three organizations cited concerns regarding patient safety and the need for improved communication among caregivers as reasons for using standard EFM definitions in clinical practice. In April 2008 the NICHD, the ACOG, and the Society for Maternal-Fetal Medicine partnered to sponsor another workshop to revisit the FHR definitions recommended by the NICHD in 1997. The 1997 FHR definitions were reaffirmed at this workshop. In addition, new definitions related to UA and a three-tier system of FHR pattern interpretation and categorization were recommended (see Box 15-1) (Macones, Hankins, Spong, et al., 2008). The baseline FHR is the average rate during a 10-minute segment that excludes periodic or episodic changes, periods of marked variability, and segments of the baseline that differ by more than 25 beats/min. There must be at least 2 minutes of interpretable baseline data in a 10-minute segment of tracing to determine the baseline FHR (Macones, Hankins, Spong, et al., 2008). After 10 minutes of tracing is observed, the approximate mean rate is rounded to the closest 5 beats/min interval (AWHONN, 2009). For example, if the FHR rate varies between 130 and 140 beats/min over a 10-minute period, the baseline is recorded as 135 beats/min. The normal range at term is 110 to 160 beats/min. In the preterm fetus the baseline rate is slightly higher. Variability of the FHR can be described as irregular waves or fluctuations in the baseline FHR of two cycles per minute or greater (Macones, Hankins, Spong, et al., 2008). It is a characteristic of the baseline FHR and does not include accelerations or decelerations of the FHR. Variability is quantified in beats per minute and is measured from the peak to the trough of a single cycle. Four possible categories of variability have been identified: absent, minimal, moderate, and marked (Fig. 15-8). In the past variability was described as either long term or short term (beat to beat). However, the NICHD definitions do not distinguish between long- and short-term variability because in actual practice they are visually determined as a unit (NICHD, 1997).
Fetal Assessment During Labor
Basis for Monitoring
Fetal Response
Uterine Activity
CHARACTERISTIC
DESCRIPTION
Frequency
Contraction frequency overall generally ranges from two to five per 10 minutes during labor, with lower frequencies seen in first stage of labor and higher frequencies (up to five contractions in 10 minutes) seen during second stage of labor.
Duration
Contraction duration remains fairly stable throughout first and second stages, ranging from 45-80 seconds, not generally exceeding 90 seconds.
Strength
Uterine contractions generally range from peaking at 40-70 mm Hg in first stage of labor to over 80 mm Hg in second stage. Contractions palpated as “mild” would likely peak at less than 50 mm Hg if measured internally, whereas contractions palpated as “moderate” or greater would likely peak at 50 mm Hg or greater if measured internally.
Resting tone
Average resting tone during labor is 10 mm Hg; if using palpation, should palpate as “soft” (i.e., easily indented, no palpable resistance).
Relaxation time
Relaxation time is commonly 60 seconds or more in first stage and 45 seconds or more in second stage.
Montevideo units (MVUs)
MVUs usually range from 100-250 in first stage; may rise to 300-400 in the second stage. Contraction intensities of 40 mm Hg or more and MVUs of 80-120 are generally sufficient to initiate spontaneous labor. MVUs are used only with internal monitoring of contractions.
Fetal Compromise
Monitoring Techniques
Intermittent Auscultation

Electronic Fetal Monitoring
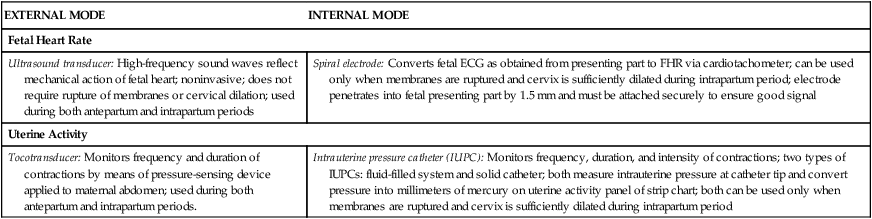
EXTERNAL MODE
INTERNAL MODE
Fetal Heart Rate
Ultrasound transducer: High-frequency sound waves reflect mechanical action of fetal heart; noninvasive; does not require rupture of membranes or cervical dilation; used during both antepartum and intrapartum periods
Spiral electrode: Converts fetal ECG as obtained from presenting part to FHR via cardiotachometer; can be used only when membranes are ruptured and cervix is sufficiently dilated during intrapartum period; electrode penetrates into fetal presenting part by 1.5 mm and must be attached securely to ensure good signal
Uterine Activity
Tocotransducer: Monitors frequency and duration of contractions by means of pressure-sensing device applied to maternal abdomen; used during both antepartum and intrapartum periods.
Intrauterine pressure catheter (IUPC): Monitors frequency, duration, and intensity of contractions; two types of IUPCs: fluid-filled system and solid catheter; both measure intrauterine pressure at catheter tip and convert pressure into millimeters of mercury on uterine activity panel of strip chart; both can be used only when membranes are ruptured and cervix is sufficiently dilated during intrapartum period
External Monitoring
Internal Monitoring
Display
Fetal Heart Rate Patterns
Baseline Fetal Heart Rate
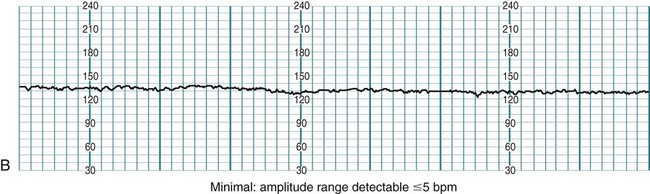
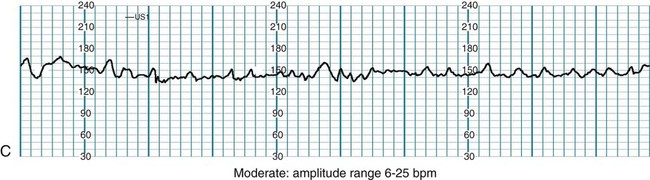
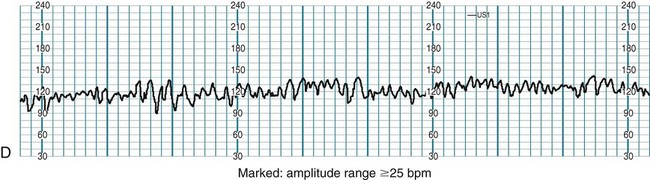
Variability
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Fetal Assessment During Labor
Get Clinical Tree app for offline access