Janice Cuzzell and M. Linda Workman
Care of Patients with Skin Problems
Learning Outcomes
Safe and Effective Care Environment
Health Promotion and Maintenance
Psychosocial Integrity
Physiological Integrity
13 Compare wound healing by first, second, and third intention.
14 Evaluate wounds for size, depth, presence of infection, and indications of healing.
17 Identify the key features of psoriasis.
18 Coordinate nursing interventions for care of the patient with psoriasis in the community.
19 Identify key features of melanoma and other skin cancers.

http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Audio Glossary
Concept Map Creator
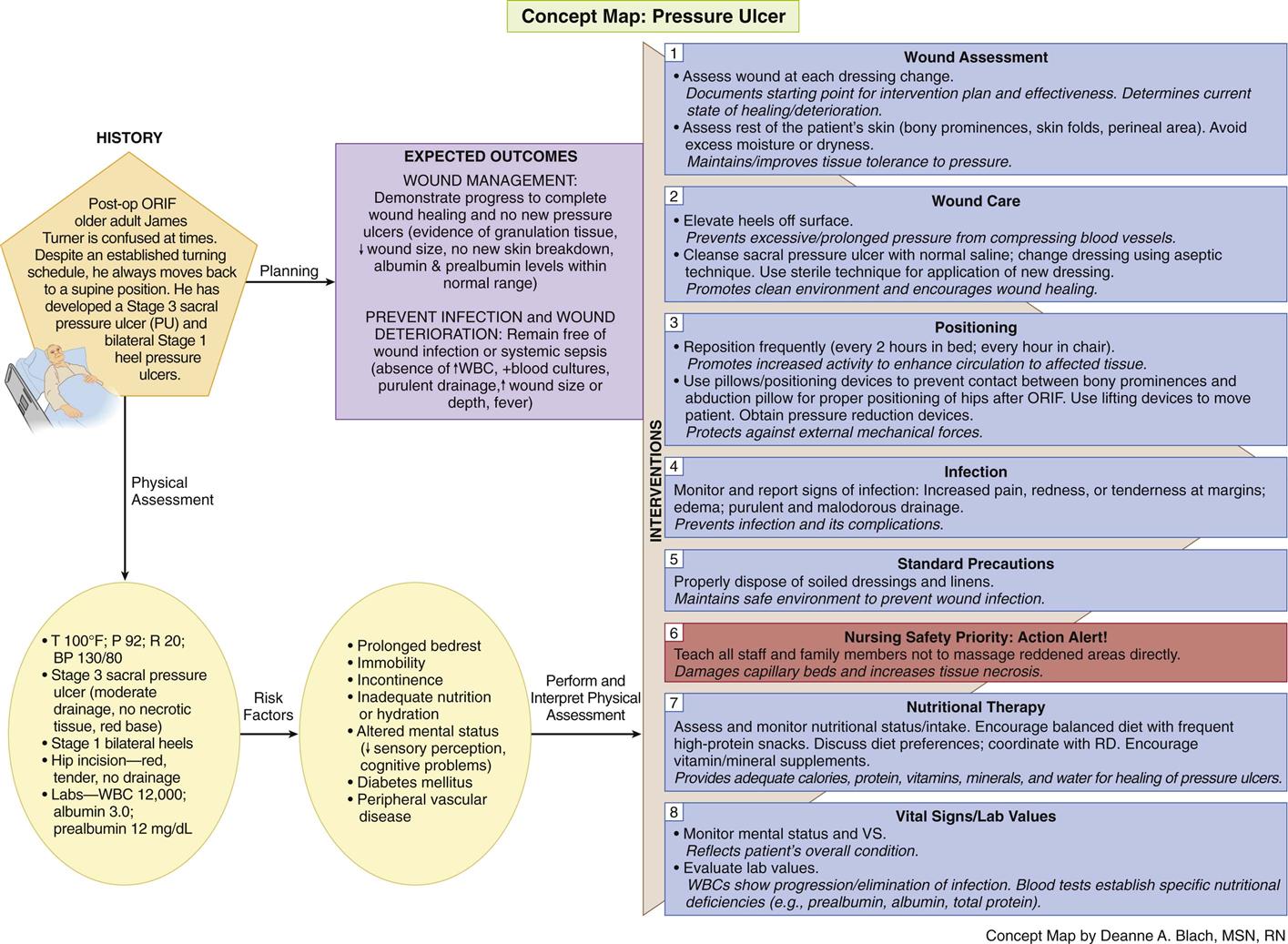
Concept Map: Pressure Ulcer
Key Points
Review Questions for the NCLEX® Examination
As discussed in Chapter 26, the skin plays an important role in protection. Like the wall surrounding a castle, it provides a strong barrier, in this case to invasion by harmful microorganisms.
Skin problems are common, especially among older adults. Changes in structural integrity reduce the skin’s protective function to some degree, and the cause of the problem is often difficult to determine. In addition to its primary functions, the skin also reflects underlying medical conditions. Thus problems may truly arise in the skin, or they may be a symptom of a systemic disease or injury.
Drugs and other interventions for any health problem can trigger a skin response or reaction. Skin problems can interfere with the medical or surgical treatment of other conditions. Age-related changes and problems caused by immobility, chronic disease, debility, and change in immune function increase the older patient’s risk for skin damage.
Minor Skin Irritations
Dryness
Pathophysiology
Dry skin (xerosis) is a common problem, especially in older patients. It is seen as a fine flaking of the stratum corneum (outermost skin layer). The problem is usually worse on the lower legs where blood flow is poorer. Generalized pruritus (itching) often occurs with dry skin. In patients with chronic skin conditions, unrelieved itching causes the patient to scratch and rub the skin in an attempt to relieve the intense itching. These actions may result in secondary skin lesions, excoriations, lichenification (thickening), and infection.
Xerosis is worse in areas with dry climates and higher altitudes, such as in the southwestern part of the United States. Central heating and air-conditioning reduce the humidity in the air and increase skin dryness. Wind, cold, and sunlight also worsen the problem. Frequent bathing with harsh soap and hot water further dries the skin, especially if moisturizers are not applied immediately after bathing when skin is damp.
Patient-Centered Collaborative Care
Nursing interventions focus on teaching the patient and family how to maintain healthy skin, rehydrate the outer skin layers, and relieve itching. Chart 27-1 lists practical ways to avoid overdrying the skin. Remind the patient that bathing with moisturizing soaps, oils, and lotions may reduce dryness. Some soaps and body washes, especially those described as “antimicrobial” and those with perfumes and other scents, may make dry skin worse. Limiting the use of soap to soiled or skinfold areas can also reduce dryness. A 20-minute soak in a warm bath, followed by application of an emollient cream or lotion, will help rehydrate the skin and reduce itching. If the patient cannot take a tub bath, teach him or her to wrap the trunk and extremities in warm, moist towels covered by plastic sheeting or a clean garbage bag for 15 to 20 minutes before applying moisturizers. Skin creams or lotions are more effective when applied to slightly damp skin within 2 to 3 minutes after bathing.
Inform patients that, contrary to popular belief, the cream or lotion is not what makes the skin soft and supple. Water is the agent that softens the outer skin layers. Lubricating creams and lotions seal in the moisture provided by water, promoting suppleness and preventing flaking. Some skin lotions are hydrophilic (water seeking) and actually draw moisture from the skin, making the dryness worse if they are not applied directly to damp skin.
Pruritus
Pathophysiology
Pruritus (itching) is a distressing symptom that may or may not occur with skin disease. It is caused by stimulation of itch-specific nerve fibers at the dermal-epidermal junction. Physical or chemical agents either act directly on these nerve fibers or activate chemical mediators, such as histamine, which then act on the itch receptors.
Itching is a subjective symptom similar to pain. Thus the sensation varies among patients in location and severity. Regardless of the underlying cause, patients usually report that itching is worse at night when there are fewer distractions. Other conditions that make itching worse include poor skin hydration, increased skin temperature, perspiration, and emotional stress.
Patient-Centered Collaborative Care
The priority nursing interventions focus on increasing patient comfort and preventing skin injury. Patients usually try to relieve itching by scratching or rubbing the skin, a response that further stimulates the itch receptors and causes a pattern referred to as the “itch-scratch-itch” cycle. When itching occurs as a symptom of skin lesions, relief can usually be obtained by treatment of the underlying skin disorder with topical or systemic drugs. Systemic diseases, such as liver and venous disorders, can also cause itching without skin lesions. Liver disease often increases the buildup of bilirubin in the skin, which stimulates itch receptors. Pruritus can also be associated with too little or too much blood flow to an area (especially the feet and legs).
Plan care to promote comfort and prevent disruption of skin integrity that can result from vigorous scratching. Because dry skin worsens itching, emphasize proper bathing and skin moisturizing techniques (see Chart 27-1). Encourage patients to keep the fingernails trimmed short, with rough edges filed to reduce skin damage from scratching and to prevent secondary infection. Tell patients that wearing mittens or splints at night can help prevent inadvertent scratching during sleep. If the patient cannot perform self-care, teach the family (for home care) and unlicensed assistive personnel (UAP) to trim the patient’s fingernails and apply mittens or gloves. As always, be sure to stress the importance of not breaking the skin or digging into nail corners when trimming the nails of patients with diabetes.
A cool sleeping environment along with comfort measures such as a cool shower and application of moisturizers may help promote sleep. Additional measures such as using sleep-promoting herbal teas or sedating antihistamines at bedtime (when the side effect of drowsiness is welcome) may provide an uninterrupted night’s sleep. Therapeutic baths with colloidal oatmeal preparations or tar extracts may also provide temporary relief.
If antihistamines are prescribed, closely monitor the patient’s response to therapy so that the dosage can be adjusted as needed. The anti-inflammatory properties of topical steroid preparations and other topical agents are increased if the drug is applied to slightly damp skin.
Using topical drugs under an occlusive dressing increases the dose of anti-inflammatory being delivered. Avoid occluding treated areas unless specifically ordered by the health care provider.
Sunburn
Sunburn is a first-degree or superficial burn and a very common skin injury. Excessive exposure to ultraviolet (UV) light injures the dermis, stimulating an inflammatory response that dilates the capillaries, leading to redness, tenderness, edema, and occasional blister formation. When large areas of the body are sunburned, systemic inflammatory symptoms, such as headache, nausea, and fever, may be produced.
Erythema (redness) and pain begin within a few hours after sunburn has occurred and increase in intensity for 1 to 2 days before subsiding. Management is directed toward promoting comfort and includes cool baths and soothing lotions, such as bland lubricants or refrigerated moisturizing lotions. Antibiotic ointments are used only if blistering of the skin causes infection. If pain is severe, topical corticosteroids and NSAIDs may reduce the inflammation temporarily.
Urticaria
Urticaria (hives) is white or red edematous papules or plaques of various sizes. This problem is usually caused by exposure to allergens (different triggers for different people), which releases histamine in the dermal tissue. Blood vessel dilation and leakage of plasma proteins lead to formation of lesions or wheals. The exact cause is rarely identified although drugs, foods, infections, autoimmune diseases, cancer, and physical stimuli often trigger urticaria.
Management focuses on removal of the triggering substance and relief of symptoms. Because the skin reaction is caused by histamine release, antihistamines such as diphenhydramine (Benadryl) are helpful. Teach the patient to avoid overexertion, alcohol consumption, and warm environments (e.g., warm or hot showers), which contribute to blood vessel dilation and make the symptoms worse. In addition, alcohol may increase any sedating effect of antihistamines, increasing the risk for falls and other accidents.
Trauma
Pathophysiology
Skin trauma can vary from an aseptic surgical incision to a grossly infected, draining pressure ulcer with deep tissue destruction. Injury to the skin starts a series of actions to repair the skin and re-establish this protective barrier.
Phases of Wound Healing
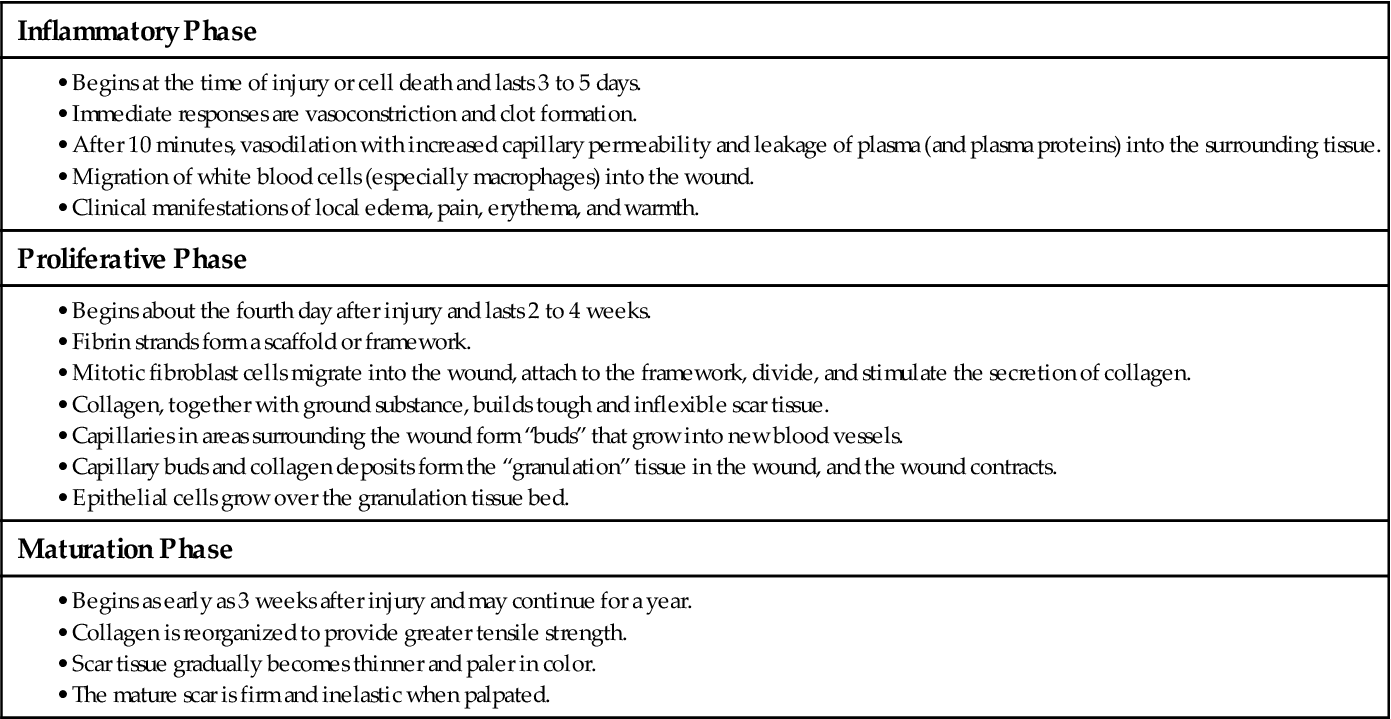
Wound healing occurs in three phases: the inflammatory (lag) phase, the proliferative (connective tissue repair) phase, and the maturation (remodeling) phase. Table 27-1 lists the key events of normal wound healing. The length of each phase depends on the type of injury, the patient’s overall health status, and whether the wound is healing by first, second, or third intention (Fig. 27-1).
TABLE 27-1
| Inflammatory Phase |
| Proliferative Phase |
| Maturation Phase |
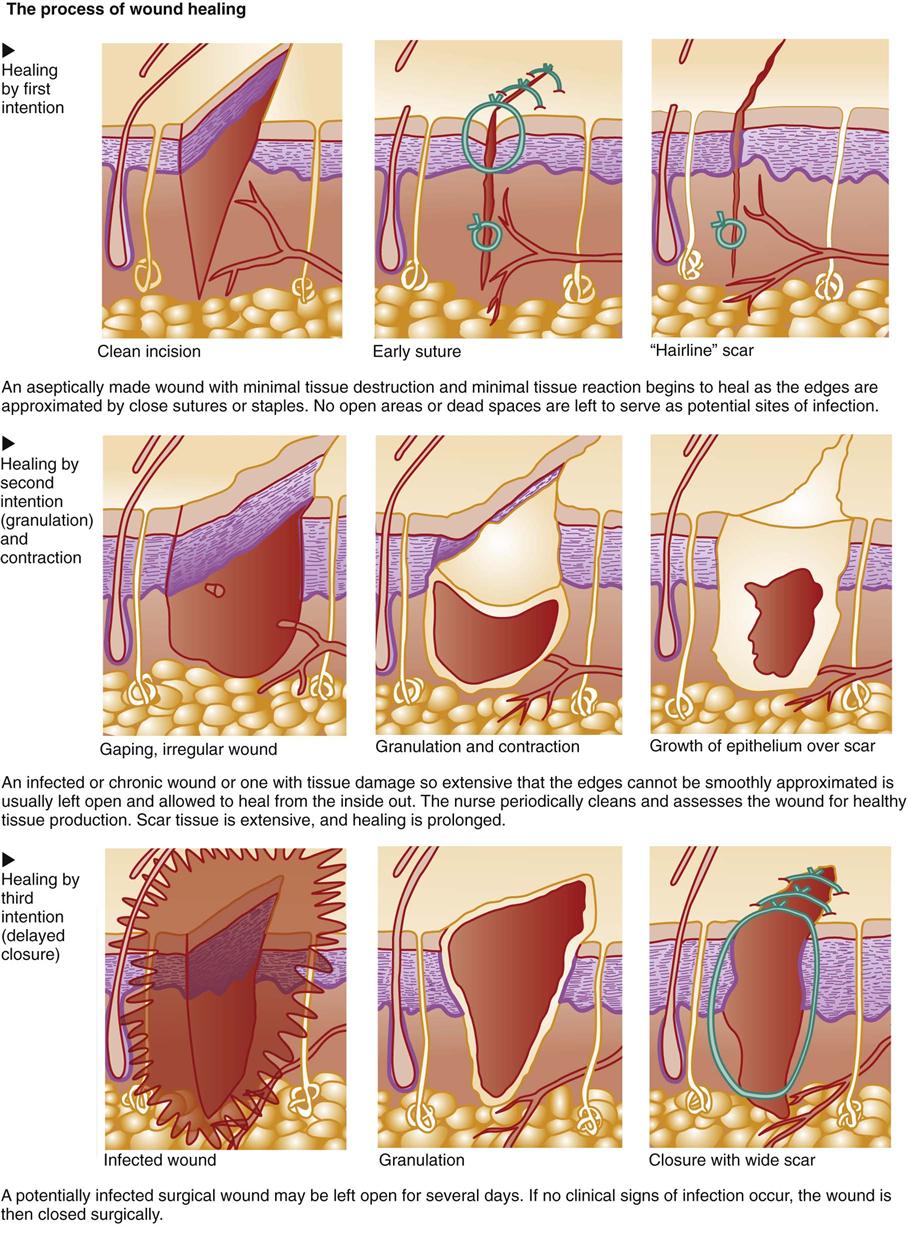
A wound without tissue loss, such as a clean laceration or a surgical incision, can be closed with sutures or staples. The wound edges are brought together with the skin layers lined up in correct anatomic position (approximated) and held in place until healing is complete. This type of wound heals by first intention because closing the wound eliminates dead space, thereby shortening the three phases of tissue repair. Inflammation resolves quickly, and connective tissue repair is minimal, resulting in less remodeling and a thin scar.
Deeper tissue injuries or wounds with tissue loss, such as a chronic pressure ulcer or venous stasis ulcer, result in a cavity-like defect that requires gradual filling in of the dead space with connective tissue. This healing occurs by second intention and prolongs the repair process.
Wounds at high risk for infection, such as surgical incisions that enter a nonsterile body cavity or traumatic wounds that occur under unclean conditions, may be intentionally left open for several days. After debris (dead cells and tissues) and exudate have been removed (débrided) and inflammation has subsided, the wound is closed by first intention. This type of healing involves delayed primary closure (third intention) and results in a scar similar to that found in wounds that heal by first intention. Healing can be impaired by many factors (Table 27-2).
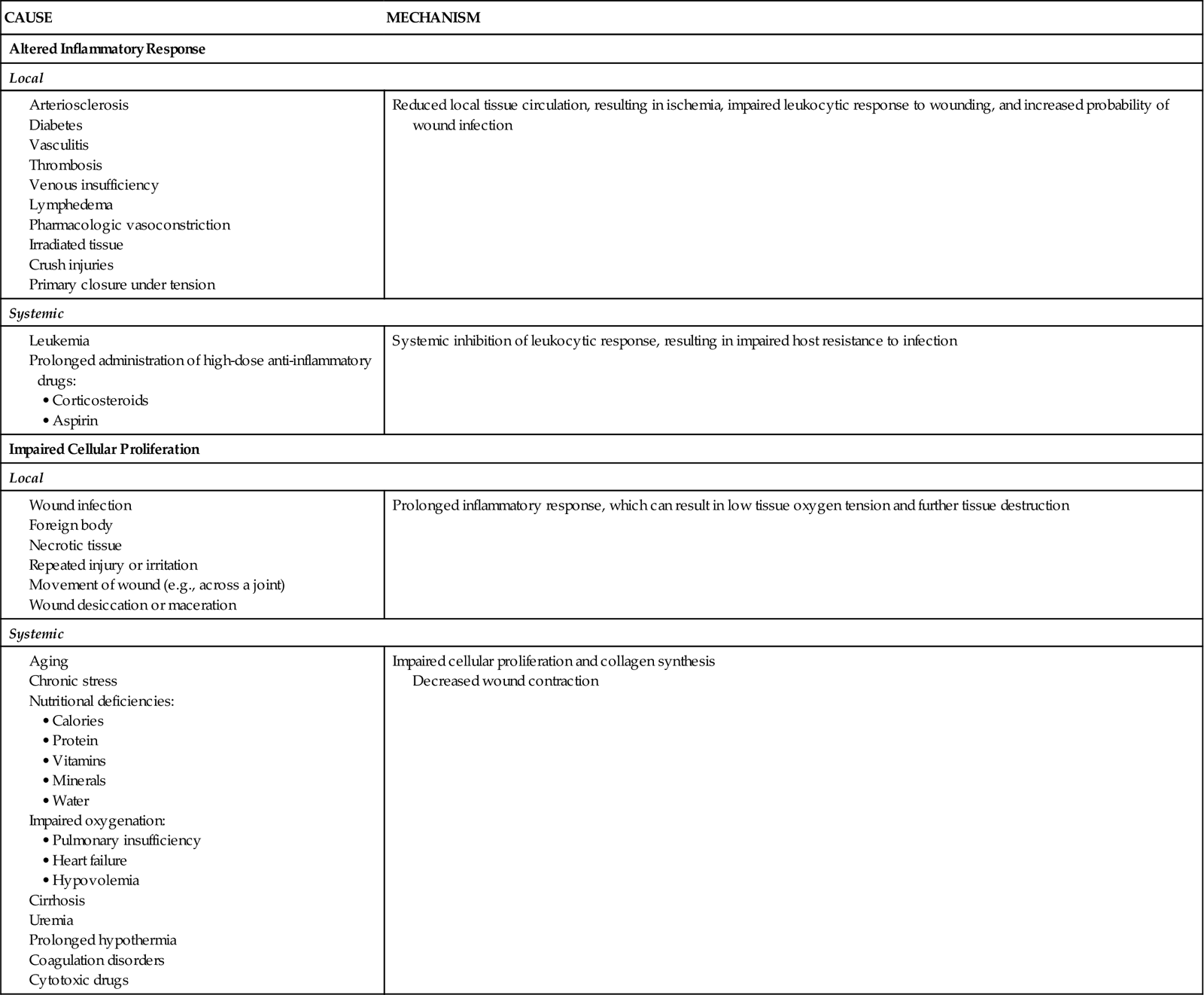
TABLE 27-2
CAUSES OF IMPAIRED WOUND HEALING
Mechanisms of Wound Healing
When injury occurs, the body restores skin integrity through three processes: re-epithelialization, granulation, and wound contraction. The depth of injury and extent of tissue loss determine how and to what degree each of these processes contributes to wound healing.
Partial-Thickness Wounds.
Partial-thickness wounds are more superficial, involving damage to the epidermis and upper layers of the dermis. These wounds heal by re-epithelialization, the production of new skin cells by undamaged epidermal cells in the basal layer of the dermis, which also lines the hair follicles and sweat glands (Fig. 27-2). Skin injury is followed immediately by local inflammation. The inflammatory response causes the formation of a fibrin clot and the release of growth factors that stimulate epidermal cell division (mitosis). New skin cells move into open spaces on the wound surface, where the fibrin clot acts as a frame or scaffold to guide cell movement. Regrowth across the open area (resurfacing) is only one cell layer thick at first. As healing continues, the cell layer thickens and stratifies (forms layers) to resemble normal skin. A healed wound re-establishes the protective barrier properties of the skin with keratin production.
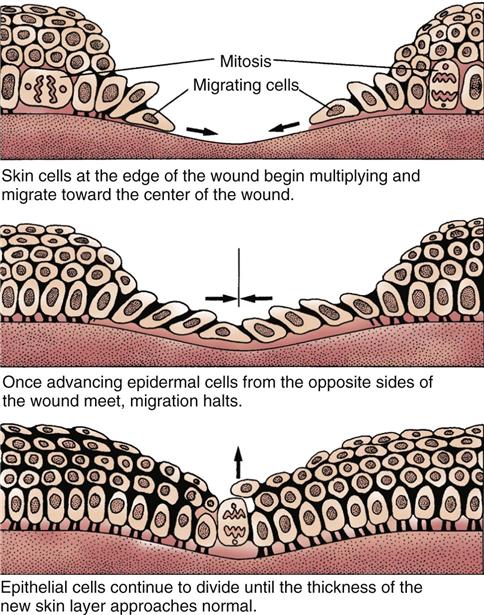
In a healthy patient, healing of a partial-thickness wound by re-epithelialization takes about 5 to 7 days. This process occurs more rapidly in tissue that is hydrated, oxygenated, and has few microorganisms present.
Full-Thickness Wounds.
In deep partial-thickness wounds and full-thickness wounds, damage extends into the lower layers of the dermis and underlying subcutaneous tissue. As a result, most of the epithelial cells at the base of the wound have been destroyed. Thus re-epithelialization is not the major healing process for this type of wound. Removal of the damaged tissue results in a defect that must be filled with scar tissue (granulation) for healing to occur. During the proliferative phase of healing, new blood vessels form at the base of the wound and fibroblastic cells begin moving into the wound space. Fibroblasts deposit new collagen to replace the damaged tissue.
Some of these fibroblasts act like smooth muscle cells and begin to pull the wound edges inward along the path of least resistance (contraction) (see Fig. 27-1). This causes the wound to decrease in size at a uniform rate of about 0.6 to 0.75 mm/day. Complete closure of a wound by contraction depends on the mobility of the surrounding skin as tension is applied to it. If tension in the surrounding skin exceeds the counterforce of wound contraction, healing will be delayed until undamaged epidermal cells at the wound edges can bridge the defect. Unlike re-epithelialization in partial-thickness wounds, which results in the return of a near-normal epithelial barrier, the bridging of epithelial cells across a large area of granulation tissue results in an unstable barrier. A venous leg ulcer is one example of a skin defect that heals poorly by contraction. Re-epithelialization of these chronic wounds often results in a thin epidermal barrier that is easily re-injured.
Re-epithelialization, granulation, and contraction do not continue indefinitely. Natural healing processes can slow down and even stop in the presence of infection, unrelieved pressure, or mechanical obstacles. For example, dead tissue not only supports the overgrowth of organisms but also obstructs collagen deposition and wound contraction. Therefore thorough wound débridement is necessary for healing to occur. In the case of chronic wounds, healing may cease spontaneously and without an obvious cause. In addition, infection in chronic wounds may not show the expected manifestations. Often the only manifestation is an increase in wound size or failure of the wound to decrease in size (Broderick, 2009).
Patient-Centered Collaborative Care
Management of skin trauma varies with the depth and type of injury. The collaborative management for any type of skin trauma focuses on enhancing wound healing, preventing infection, and restoring function to the area. Effective management of pressure ulcers or of burns includes interventions that support a healing environment (see Chapter 28).
Pressure Ulcers
Pathophysiology
A pressure ulcer is tissue damage caused when the skin and underlying soft tissue are compressed between a bony prominence and an external surface for an extended period. Although they commonly occur over the sacrum, hips, and ankles, pressure ulcers can occur on any body surface. For example, nasal cannula tubing that is too tight can cause pressure ulcers behind the ears or in the nares.
Tissue compression from pressure restricts blood flow to the skin, resulting in reduced tissue perfusion and oxygenation and, eventually, leading to cell death. Ulcers occur most often in people with limited mobility because they cannot change their position to relieve pressure. Sensory impairment is also a contributing factor. Patients who cannot feel or communicate the pain that occurs with unrelieved pressure are more likely to develop pressure ulcers. Once formed, these chronic wounds are slow to heal, resulting in increased morbidity and health care costs. Complications associated with chronic pressure ulcers include sepsis, kidney failure, infectious arthritis, and osteomyelitis.
Other factors increase the risk for pressure ulcer formation. Friction and shear are mechanical forces that impair skin integrity and set the stage for skin breakdown. Excessive skin moisture, such as urinary or fecal incontinence, increases the risk for skin damage when external mechanical forces are applied. Nutritional status is also an important concern. Protein malnutrition not only makes normal tissue more prone to breakdown but also delays healing (Slachta, 2008).
Mechanical Forces
Pressure occurs as a result of gravity. Dependent tissues in contact with a fixed surface experience varying degrees of pressure. Pressure is determined by the amount of weight exerted at the point of contact, the distribution of weight at the point of contact, and the density of the contacting surface. Excessive or prolonged pressure can compress blood vessels at the point of contact, such as over bony prominences. Unrelieved pressure leads to ischemia, inflammation, and tissue necrosis. Pressure occurs when the patient is positioned on a hard surface that does not diffuse his or her weight or when he or she remains in the same position too long.
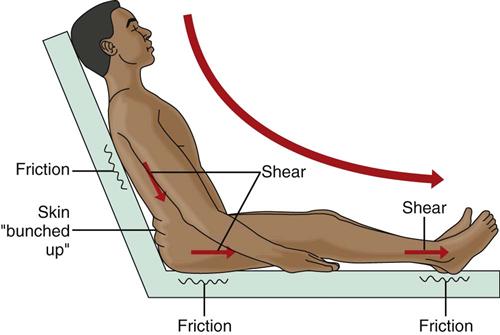
Friction occurs when surfaces rub the skin and irritate or directly pull off epithelial tissue. Such forces are generated when the patient is dragged or pulled across bed linen.
Shear or shearing forces are generated when the skin itself is stationary and the tissues below the skin (e.g., fat, muscle) shift or move (Fig. 27-3). The movement of the deeper tissue layers reduces the blood supply to the skin, leading to skin hypoxia, anoxia, ischemia, inflammation, and necrosis.
Gravity plays a role in the development of shearing forces. A shear injury usually occurs when a patient is in bed in a semi-sitting position and gradually slides downward. Often the skin over the sacrum does not slide down at the same pace as the deeper tissues; thus the skin is mechanically “sheared,” causing blood vessels to stretch and break. Shearing leads to soft-tissue ischemia and deep tissue injury, even though no external break in skin integrity is observed.
Incidence/Prevalence
Pressure ulcer development is a problem found among patients in the acute care setting, long-term care facility, and home care setting. Although patient care has improved in many ways and new products are available for prevention and treatment, 3% to 14% of hospitalized patients still experience pressure ulcer formation (Dunleavy, 2008).
Health Promotion and Maintenance
Pressure ulcers can be prevented if the risk is recognized and intervention begins early (Chart 27-2) (Ackerman, 2011). Key health care team members for pressure ulcer prevention and management are the certified wound care specialist and the dietitian.
A pressure ulcer prevention program consists of two steps: (1) early identification of high-risk patients, and (2) implementation of aggressive intervention for prevention with the use of pressure-relief or pressure-reduction devices. Pressure mapping is a method for identifying specific anatomic areas at risk for breakdown and planning interventions for patients who are bedridden or wheelchair bound. The process of pressure mapping involves the use of a computerized tool that measures pressure distribution for a person sitting in a chair or lying on a mattress (Hanson et al., 2007). The map is displayed as colored areas on the computer screen based on temperature differences. Shades of red indicate areas of greater heat production and are associated with increased pressure loads. Shades of blue indicate cooler areas under lower pressure. When used in combination with more traditional risk assessment tools, pressure mapping appears to help identify problem areas before visual changes occur and allows for more targeted prevention strategies.
Effective risk identification and prevention measures include education of the patient and the caregiver. Documentation of risk assessment, implementation of prevention measures, and education of all people involved in the care of the patient at risk for pressure ulcer formation are key to the plan’s success (Dunleavy, 2008). Periodic re-assessment of risk and continuing evaluation are critical, especially when the patient’s condition changes.
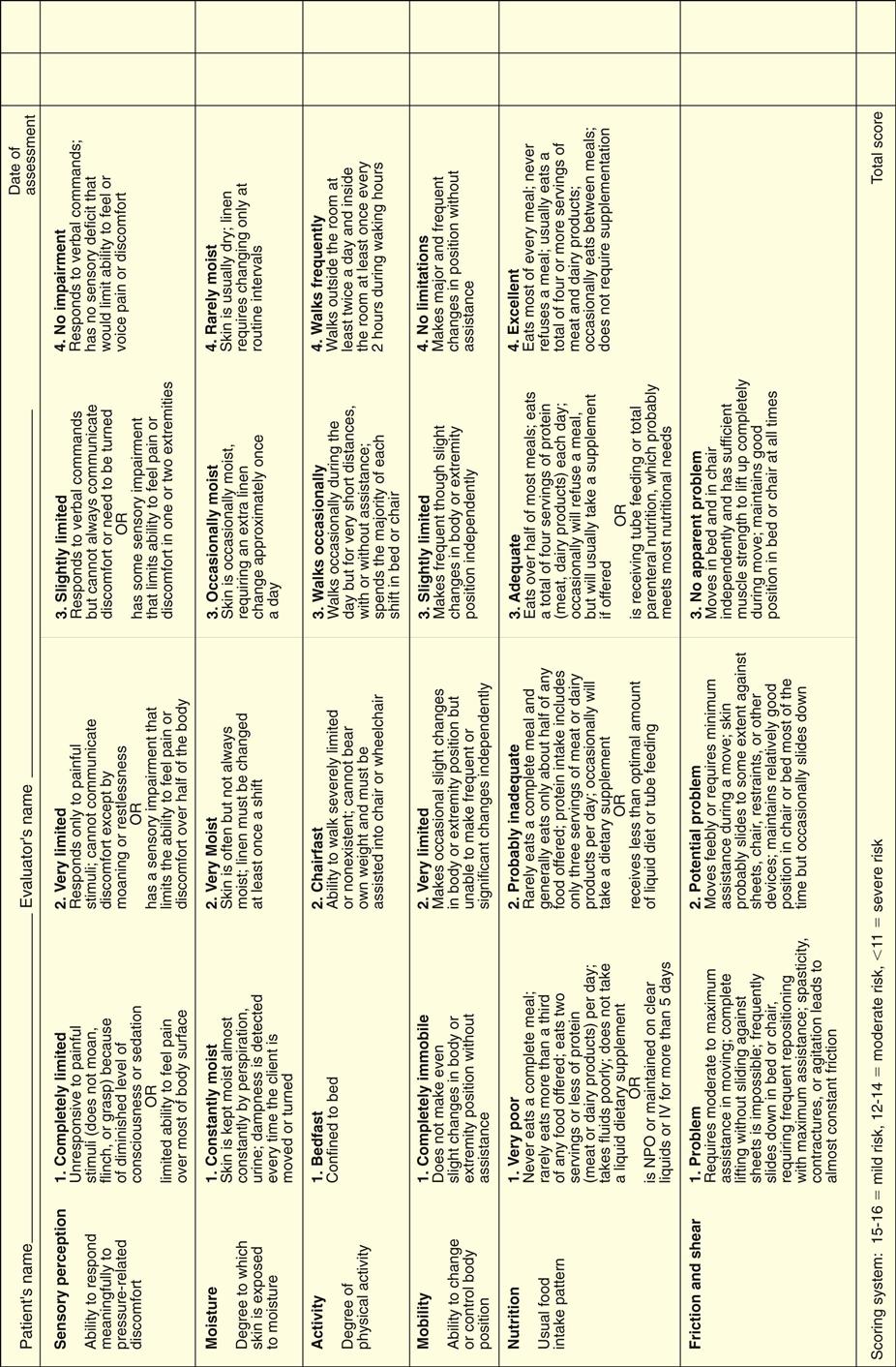
Identification of High-Risk Patients
As suggested by The Joint Commission’s National Patient Safety Goals (NPSGs), all patients admitted to a health care facility or home care agency should be assessed for pressure ulcer risk. The use of a risk assessment tool increases the chances of identifying those patients at greater risk for skin breakdown. The Braden Scale (Fig. 27-4) is the most commonly used skin risk assessment tool. This validated tool helps the nurse assess and document the various risk categories for pressure ulcer formation including mental status, activity and mobility, nutritional status, and incontinence.
Mental status changes and decreased sensory perception determine whether the patient is a partner in the prevention of pressure ulcers. When the patient understands that turning and shifting of weight prevent tissue damage, the risk for pressure ulcers decreases. Stroke, head injury, organic brain disease, Alzheimer’s disease, or other problems with cognition increase the risk for pressure ulcer formation.
Independent mobility is a direct factor in the risk for pressure ulcer formation. Patients who have unimpaired mobility and can respond to pain are at low risk for pressure ulcer formation. Regardless of age, any patient who requires assistance with turning and positioning or who is unable to verbalize discomfort is at higher risk for pressure ulcer formation. Anyone who is confined to bed or a chair also is at higher risk than a patient who requires assistance only with ambulation.
Nutritional status is a critical risk factor for pressure ulcer development and for successful healing (Slachta, 2008). Intact skin and wound healing depend on a positive nitrogen balance and adequate serum protein levels. The patient in negative nitrogen balance not only heals more slowly but also is at greater risk for accelerated tissue destruction. Draining wounds contribute to protein loss and require more aggressive intervention.
Nutritional status assessment includes laboratory studies; evaluation of weight and recent weight change; ability of the patient to consume an adequate diet; and the need for vitamin, mineral, or protein supplementation. Serum albumin and prealbumin levels are often used to monitor nutritional status. Prealbumin is a more sensitive marker because it has a shorter half-life. Nutrition is considered inadequate when the serum albumin level is less than 3.5 g/dL, the prealbumin level is less than 19.5 mg/dL, or the lymphocyte count is less than 1800/mm3. However, serum protein levels are affected by a number of other factors including level of hydration, metabolic stress, and infection. Therefore laboratory values are valuable only when supported by additional assessment information. Other indicators of inadequate nutrition include poor daily intake of food and fluids with a weight loss greater than 5% change in 30 days or greater than 10% change in 180 days (Dorner et al., 2009).
A positive nitrogen balance requires an intake of 30 to 35 calories per kilogram of body weight daily with a protein intake of 1.25 to 1.5 g/kg/day. Up to 2 g/kg/day of protein may be needed when nutritional deficits are severe or protein loss is ongoing. Vitamin and mineral supplementations are based on the patient’s nutritional status.
Incontinence results in prolonged contact of the skin with such substances as urea, bacteria, yeast, and enzymes carried in urine and feces. These substances are irritants that destroy the integrity of the skin’s barrier, predisposing that patient to skin breakdown. Excessive moisture macerates intact skin, further increasing the risk for breakdown. Daily inspection of the skin for any areas of redness, maceration, or skin breakdown is a major part of pressure ulcer prevention. Maintenance of clean, dry, intact skin also assists in the prevention process. The skin should be washed with a pH-balanced soap to maintain the normal acid level. Creams or lotions are used to lubricate and moisturize the skin. Barrier ointments protect intact skin from urine and feces when incontinence is present. Absorbent pads or garments must be changed immediately with each incontinence episode to avoid prolonged skin contact with urine or feces.
Pressure-Relieving and Pressure-Reducing Techniques
The cornerstone in the prevention (and treatment) of pressure ulcers is adequate pressure relief. A factor in pressure relief is the capillary closing pressure, which is the amount of pressure needed to occlude skin capillary blood flow, in the area at risk. The normal capillary closing pressure ranges from 12 to 32 mm Hg. An effective pressure-relieving device is one that keeps tissue pressure below the capillary closing pressure to ensure adequate tissue perfusion and oxygenation. Most devices have a standardized guaranteed pressure-relief reading; however, these readings do not ensure that capillary blood flow for any given patient is adequate. Observe skin color, integrity, and temperature directly to determine capillary flow adequacy.
Devices are classified according to whether they relieve pressure or merely reduce pressure. In addition, devices are further classified as dynamic or static. Dynamic systems alternate inflation and deflation of the device through the use of electricity. Static devices made of gel, water, foam, or air are in a constant state of inflation that distributes the patient pressure load over a larger area and reduces the pressure experienced by any particular area.
Pressure-relief/pressure-reduction products come in many forms, such as specialty beds, mattress replacements, overlays, and assistive devices. Choosing the correct product is important in the success of the prevention plan. Re-evaluate the selected product in use daily for effectiveness in reducing pressure, providing comfort, and eliminating “bottoming out.” Bottoming out occurs when the selected product is not providing adequate pressure relief and the patient’s bony prominences sink into the mattress or cushion.
Pressure-relief devices consistently reduce skin pressure below capillary closing pressure. These devices are recommended for patients who need:
• Prevention of skin breakdown because they cannot turn (e.g., immobility, loss of sensation)
• Prevention of extension of skin breakdown that has already occurred
• Promotion of healing for breakdown present on several turning surfaces
Pressure-reduction devices lower pressure below that of a standard hospital mattress or chair surface but do not reduce pressure consistently below the capillary closing pressure. These devices are effective for preventing pressure ulcers only when used together with a turning schedule and other skin care measures.
Frequent repositioning of bedbound patients, as described in Chart 27-2, is critical in reducing pressure over bony prominences. A good plan for positioning is the 30-degree rule. This plan ensures that the patient is positioned and propped so that whatever part of the body is elevated is tilted back at least a 30-degree angle to the mattress rather than resting directly on a dependent bony prominence. This rule applies to side-lying as well as head-of-bed elevation positions. The patient who requires greater head elevation because of respiratory difficulties should be tilted forward more than 30 degrees with pillows behind the back to keep pressure off of the sacral/coccyx area. Often positioning is delegated to UAP. Teach UAP the importance of proper positioning, and demonstrate how to perform it. Also teach family members to use these techniques in the home.
The patient at risk for pressure ulcers in bed is also at risk while sitting. Carefully assess for proper wheelchair or regular chair cushioning. Collaborate with physical therapists and rehabilitation specialists for selection of these products. High-risk patients who are chair bound should also be periodically assisted to a standing position to promote tissue perfusion and prevent breakdown over the sacral area.
Even with an appropriate mattress or cushion, the patient needs to change or be helped to change positions periodically. Many facilities require turning and positioning every 2 hours. However, pressure can occur in less time, and the actual turning or repositioning schedule for each patient must be individualized. When this action is delegated to UAP, teach them the importance of maintaining a repositioning schedule.
Use pillows and other positioning or padding devices to keep heels pressure-free at all times for high-risk patients. Assess heel positioning every 4 hours to ensure that pressure is not redistributed to another high-risk area, such as the ankles or sides of the feet. Check heels even more frequently when devices that hide the feet (e.g., boots, heel protectors) are used, especially if the patient has a peripheral vascular problem. In addition to the heels, check knees and elbows at regular intervals, especially when the patient is in a side-lying position.
Patient-Centered Collaborative Care
Assessment
History
When taking a history from the patient with a pressure ulcer, identify the cause of skin loss, as well as factors that may impair healing. Ask about the specific circumstances of the skin loss. Often patients with chronic pressure ulcerations have a history of delayed healing or recurrence of the ulcer after healing has occurred. Because pressure-related skin loss is common among severely debilitated patients, determine whether a patient has any of these contributing factors:
Physical Assessment/Clinical Manifestations
Inspect the entire body, including the back of the head, for areas of skin injury or pressure. Give special attention to bony prominences (e.g., the heels, sacrum, elbows, knees, trochanters, posterior and anterior iliac spines) and areas that are vulnerable to excessive moisture. In addition, assess the patient’s general appearance for issues related to skin health, such as body weight and the proportion of weight to height. Obese patients, as well as thin patients, are at increased risk for malnutrition and pressure ulcer formation. Check overall cleanliness of the skin, hair, and nails. Determine whether any loss of mobility or range of joint motion has occurred. This assessment should not be delegated to UAP.
Wound Assessment
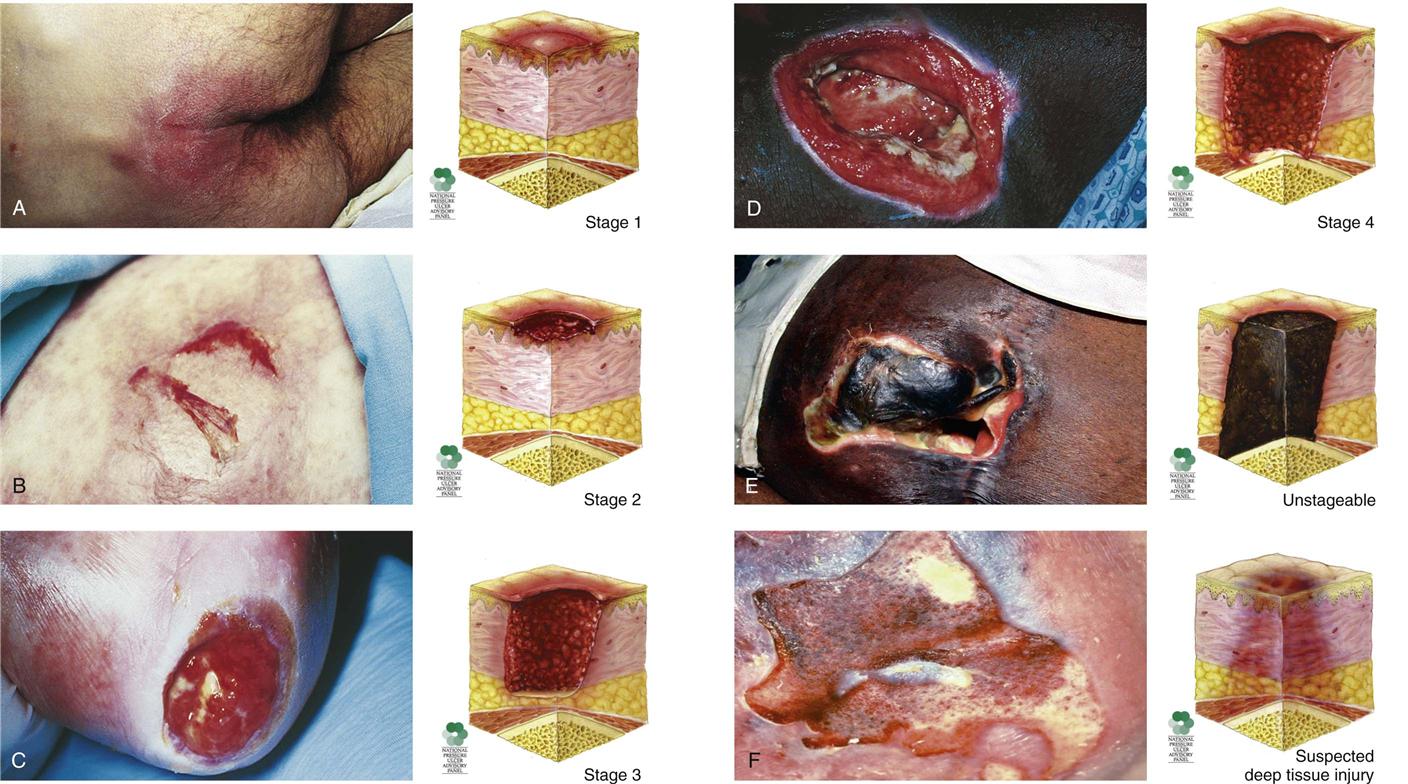
The appearance of pressure ulcers changes with the depth of the injury. Chart 27-3 lists the features of the six categories or stages of pressure ulceration, and Fig. 27-5 shows examples.
Assess wounds for location, size, color, extent of tissue involvement, cell types in the wound base and margins, exudate, condition of surrounding tissue, and presence of foreign bodies. Document this initial assessment to serve as a starting point for determining the intervention plan and its effectiveness. How often a wound is assessed is determined by the written policies and procedures at the facility or agency. Weekly documented assessment is the standard in many long-term care facilities; however, daily assessment is needed when the patient is in an acute care setting. Also assess the wound at each dressing change, comparing the existing wound features with those documented previously to determine the current state of healing or deterioration.
For intact areas that are red (in lighter-skinned patients), press firmly with fingers at the center of the area and assess whether the area blanches (lightens) with pressure. An area that blanches with pressure and then returns to normal when pressure is removed indicates color changes related to blood vessel dilation rather than tissue damage or inflammation. When blanching does not occur with pressure, the redness is more likely to be a manifestation of skin injury. Document whether the reddened area blanches with pressure.
Record the location and size of the wound first. Wounds are sized by length, width, and depth using millimeters or centimeters. In standardizing wound size for documentation and communication purposes, assess the wound as a clock face with the 12 o’clock position in the direction of the patient’s head and the 6 o’clock position in the direction of the patient’s feet. Always measure the length from the 12 o’clock position to the 6 o’clock position and the width between the 9 o’clock position and the 3 o’clock position. Measure depth as the distance from the deepest portion of the wound base to the skin level. Use disposable paper tape measures to obtain the length and width of a wound. Touch the bottom of the wound with a cotton-tipped applicator or swab and mark the place on the swab that is level with the skin surface to obtain wound depth. Then measure the area of the swab between the tip and the mark. When all caregivers use this format, measurement is accurate and wound progress can be determined (Hanson et al., 2007).
Inspect the wound margins for cellulitis (inflammation of the skin cells) extending beyond the area of injury. Progressive tissue destruction, seen as an increase in the size or depth of the ulcer and increased wound drainage, usually indicates impairment in the patient’s ability to resist infection if proper measures have been taken to relieve pressure.
Inspect the wound for the presence or absence of necrotic tissue. Because of the depth of tissue destruction, a full-thickness pressure ulcer is often covered by a layer of black, gray, or brown nonviable, denatured collagen called wound eschar.
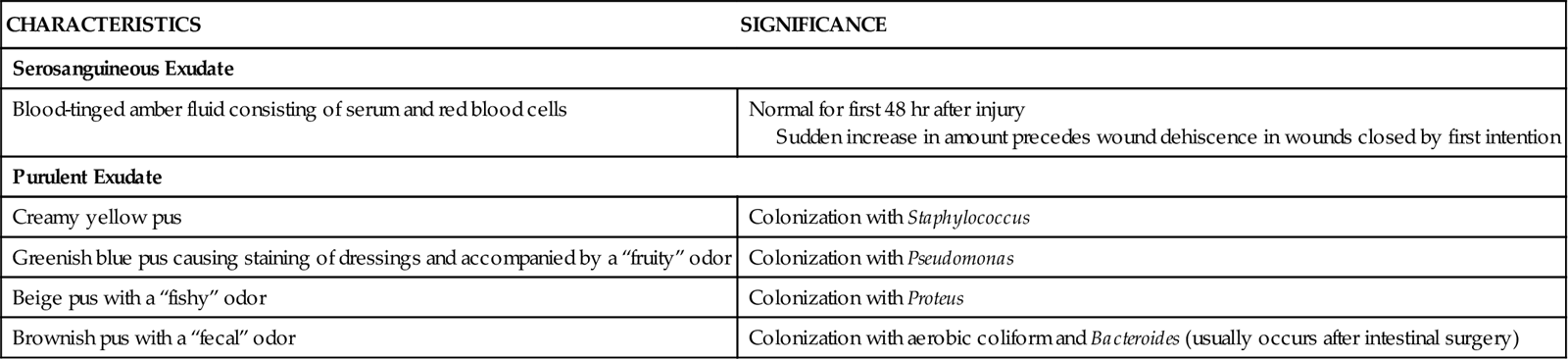
In the early stages of wound healing, the eschar is dry, leathery, and firmly attached to the wound surface. As the inflammatory phase of wound healing begins and removal of wound debris progresses, the eschar starts to lift and separate from the tissue beneath. This nonliving eschar is a good breeding ground for bacteria normally found on the skin surface, as well as those introduced by incontinence or other means. As bacteria increase, they release enzymes that soften necrotic tissue. This tissue becomes softer and more yellow. In the presence of bacterial colonization, wound exudate increases substantially; the color and odor of wound exudate indicate the major organism present. The features of wound exudate are listed in Table 27-3.
TABLE 27-3
| CHARACTERISTICS | SIGNIFICANCE |
| Serosanguineous Exudate | |
| Blood-tinged amber fluid consisting of serum and red blood cells | Normal for first 48 hr after injury Sudden increase in amount precedes wound dehiscence in wounds closed by first intention |
| Purulent Exudate | |
| Creamy yellow pus | Colonization with Staphylococcus |
| Greenish blue pus causing staining of dressings and accompanied by a “fruity” odor | Colonization with Pseudomonas |
| Beige pus with a “fishy” odor | Colonization with Proteus |
| Brownish pus with a “fecal” odor | Colonization with aerobic coliform and Bacteroides (usually occurs after intestinal surgery) |
Beneath the separating dead tissue, granulation tissue appears. Early granulation is pale pink, progressing to a beefy red color as it grows and fills the wound. Palpate the wound to determine the texture of the granulations. Healthy granulation tissue is moist and has a slightly spongy texture. Wounds with poor local arterial blood supply or that have stopped healing appear dry with granulation tissue that is hard (fibrotic) when palpated. Venous obstruction causes an excessively moist ulcer surface with a deep reddish purple color (reflective of the deoxygenated blood beneath the ulcer surface).
Pressure ulcers may involve more extensive tissue destruction than is first seen on inspection. Separation of the skin layers at the wound margins from the underlying granulation tissue is known as undermining. Inspect undermined areas for gradual filling with healthy granulations and for wound-healing progress. Palpate the bony prominences for deep hardening of the surrounding soft tissue, which often occurs with deep tissue ischemia.
After ischemia has occurred, continued pressure over the area increases tissue destruction from the deep tissue layers toward the surface, resulting in the formation of tunnels. This “hidden” wound may first have a small opening in the skin with purulent drainage. If such an opening is observed, use a cotton-tipped applicator to probe gently for a much larger tunnel or pocket of necrotic tissue beneath the opening. Additional tunnels may also occur along the main wound. Check all wounds for tunneling and, if present, document the location and length of each tunnel.
Psychosocial Assessment
The patient with pressure ulcers may have an altered body image. Ineffective coping patterns emerge as the patient and family strive to adhere to changes in lifestyle that are needed for healing. In addition, chronic ulcers are often painful and costly to treat.
Assess the patient’s and family’s knowledge of the treatment goals at each stage of the healing process, as well as adherence to the prescribed treatment regimen. Also assess the patient’s skills in cleaning the wound and applying a dressing. Poor adherence to pressure ulcer care procedures may reflect an inability to accept the diagnosis or to cope with the pain, cost, or potential scarring associated with prolonged healing. Depending on the patient’s activity level and the location of the ulcer, assistance of a family member or home care nurse may be needed to provide initial care of the pressure ulcer at home.
Explore with the patient specific changes in ADLs that are needed to relieve pressure and promote healing. Promote increased activity whenever possible to enhance circulation to the affected tissue. Leg position changes may be needed for chronic leg ulcers, depending on whether or not peripheral vascular problems contribute to their formation. For patients who have arterial insufficiency, having the legs and feet in a dependent position works with gravity to help ensure adequate blood flow to the lower legs. When arterial blood flow is adequate but venous return is impaired, elevation of the legs may be needed for healing. When the patient is bedridden, frequent repositioning to relieve pressure (every 2 hours in bed, every 1 hour in a chair) can be labor intensive. In the home, repositioning, incontinence management, and dressing changes are often needed around the clock, disrupting family routines and contributing to stress.
Laboratory Assessment
A wound that is exposed is always contaminated but is not always infected. Contamination is the presence of organisms without any manifestation of infection. The normal immune defenses of the body keep the number of bacteria to a minimum and prevent infection. Wound infection is contamination with pathogenic organisms to the degree that growth and spread cannot be controlled by the body’s immune defenses. Wounds that are red and indurated with moderate to heavy exudate and an odor should be cultured to identify the causative organism and determine sensitivity to antibiotics. The presence of purulent exudate alone does not indicate a local or systemic infection because pus formation occurs when necrotic tissue liquefies and separates.
If wounds are extensive, if the patient is severely immunocompromised, or if local blood supply to the wound is impaired, bacterial growth may exceed the body’s ability to defend against invasion into deeper tissue layers. The result is deep wound infection and eventually bacteremia and sepsis (systemic infection).
Swab cultures are helpful only in identifying the types of bacteria present on the ulcer surface and may be misleading when trying to identify or quantify bacteria in deeper tissues. Wound biopsies allow the numbers of bacteria to be analyzed, but these tests are time consuming, costly, and unavailable in many laboratories. Therefore clinical indicators of infection (cellulitis, progressive increase in ulcer size or depth, changes in the quantity and quality of exudate) and systemic signs of bacteremia (e.g., fever, elevated white blood cell [WBC] count) are used to diagnose an infection.
Other Diagnostic Assessment
Additional laboratory studies are performed on the basis of the suspected cause of the wound. For pressure ulcers to show progress toward healing, the factors contributing to delayed healing must be diagnosed and treated. For example, noninvasive and invasive arterial blood flow studies are indicated if arterial occlusion is suspected in delayed healing of a pressure ulcer on the heel or ankle. Blood tests to establish specific nutritional deficiencies (e.g., prealbumin, albumin, total protein) are helpful in treating the debilitated, malnourished patient with a pressure ulcer.
Analysis
Priority problems for patients with pressure ulcers are:
Planning and Implementation
The Concept Map on p. 484 addresses care issues related to patients who have or are at risk for pressure ulcers.
Managing Wounds
Planning: Expected Outcomes.
The patient with a pressure ulcer is expected to demonstrate progress to complete wound healing and not develop new pressure ulcers. Indicators include:
Interventions.
Wound care techniques for pressure ulcers vary according to each patient’s needs and the health care provider’s preferences. Surgery with aggressive removal of necrotic tissue may be indicated for some patients, whereas a nonsurgical approach to ulcer débridement is preferred for an older patient who has adequate defenses but is too ill or debilitated for surgery.
Nonsurgical Management.
General interventions for pressure ulcer care are listed in Chart 27-4. Nonsurgical intervention of pressure ulcers is often left to the discretion of the nurse, who coordinates with the health care provider and certified wound care specialist (if available) to select a method of wound dressing on the basis of the identified goal of wound management. Many agencies have guidelines or protocols for wound dressings based, for example, on wound size and depth and presence of drainage.
Dressings.
A properly designed dressing can speed healing by removing unwanted debris from the ulcer surface, protecting exposed healthy tissues, and creating a barrier between the body and the environment until the ulcer is closed. For a patient with a draining, necrotic ulcer, the dressing must also remove excessive exudate and loose debris without damaging epithelial cells or newly formed granulation tissue. If necrosis is extensive and the eschar is thick, dead tissue must be surgically or chemically removed before further débridement with dressings can be effective. Depending on the dressing material used, dressings help remove debris either through mechanical débridement (mechanical entrapment and detachment of dead tissue), topical chemical débridement (enzyme preparations applied topically to loosen necrotic tissue), or by natural chemical débridement (creating an environment that promotes self-digestion of dead tissues by naturally-occurring bacterial enzymes [autolysis]) (Table 27-4).
TABLE 27-4
COMMON DRESSING TECHNIQUES FOR WOUND DÉBRIDEMENT
| TECHNIQUE | MECHANISM OF ACTION |
| Wet-to-damp saline-moistened gauze | As with the wet-to-dry technique, necrotic debris is mechanically removed but with less trauma to healing tissue. |
| Continuous wet gauze | The wound surface is continually bathed with a wetting agent of choice, promoting dilution of viscous exudate and softening of dry eschar. |
| Topical enzyme preparations | Proteolytic action on thick, adherent eschar causes breakdown of denatured protein and more rapid separation of necrotic tissue. |
| Moisture-retentive dressing | Spontaneous separation of necrotic tissue is promoted by autolysis. |
After all the dead tissue has been removed, protection of any exposed tendons, bone, and newly formed collagen is critical to pressure ulcer care. The ideal environment for healing is a clean, slightly moist ulcer surface with minimal bacterial colonization. Heavy moisture from an excessively draining ulcer or a dressing that is too wet interferes with healing by promoting the growth of organisms and causing maceration (mushiness) of healthy tissue. Likewise, if a clean ulcer surface is exposed to air or if highly absorbent dressing materials are used for prolonged periods, the drying effect can dehydrate surface cells, form scabs, and convert the wound to a deeper injury.
Assess the ulcer for necrotic tissue and the quantity of exudate. Coordinate with a wound care specialist to select a dressing material with properties that promote an optimal environment for healing. For example, a material that does not stick to the wound surface and does not remove fragile epithelial cells when it is changed is the dressing of choice for protecting new tissue. Depending on the amount of drainage, select either a hydrophobic or a hydrophilic material:
A variety of synthetic materials with different absorbent properties are available (Table 27-5). Unlike cotton gauze dressings, these may be left intact for extended periods. Biologic and synthetic skin substitutes are available that can also prevent tissue dehydration and promote healing (see Chapter 28). However, the use of these products for chronic wounds is often cost prohibitive.
TABLE 27-5
COMMONLY USED DRESSING MATERIALS
| ALGINATE | BIOLOGIC DRESSING | COTTON GAUZE DRESSING | FOAM | HYDROCOLLOIDAL | HYDROGEL DRESSING | ADHESIVE TRANSPARENT FILM* | |
| Indications | |||||||
| Advantages | Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|