Postpartum Assessment and Nursing Care
Objectives
2. Describe the postpartum period.
3. Explain the involution of the uterus, and describe changes in the fundal position.
4. Explain the cause of afterpains.
5. Distinguish between the characteristics of lochia rubra, lochia serosa, and lochia alba.
6. Explain how to assess the postpartum woman’s perineum.
8. Explain the importance of monitoring the vital signs during the first 24 hours postpartum.
9. List three factors that influence urinary retention after delivery.
10. Discuss three factors that contribute to postpartum constipation.
11. List two significant events that occur as a result of changes in the endocrine system.
12. Explain the factors involved in the woman’s weight loss after birth.
13. Interpret Rubin’s taking-in and taking-hold phases.
14. Explain the psychological alteration called postpartum blues.
15. Demonstrate three ways to prepare the sibling for the new family member.
16. Present two ways to encourage parent-newborn attachment.
17. Explain why early ambulation is encouraged.
18. Review the importance of Kegel (perineal tightening) exercises.
19. Describe five danger signs that the woman should report after discharge from the hospital.
Key Terms
afterpains (p. 228)
diaphoresis (d![]() -ă-fŏ-RĒ-s
-ă-fŏ-RĒ-s![]() s, p. 231)
s, p. 231)
diastasis recti (d![]() –
–![]() S-tā-s
S-tā-s![]() s RĔK-t
s RĔK-t![]() , p. 230)
, p. 230)
diuresis (d![]() -ŭr-Ē-s
-ŭr-Ē-s![]() s, p. 231)
s, p. 231)
episiotomy (ĕ-pēz-ē-ŎT-ō-mē, p. 229)
exfoliation (ĕks-fō-lē-Ā-shŭn, p. 226)
Homans’ sign (p. 230)
involution (![]() n-vō-LOO-shŭn, p. 226)
n-vō-LOO-shŭn, p. 226)
letting-go phase (p. 234)
lochia alba (LŌ-kē-ă ![]() L-bă, p. 228)
L-bă, p. 228)
lochia rubra (ROO-bră, p. 228)
lochia serosa (sĕr-Ō-să, p. 228)
postpartum blues (p. 234)
postpartum fatigue (p. 245)
puerperium (pū-ĕr-PĒ-rē-ŭm, p. 224)
REEDA scale (p. 229)
sitz bath (p. 241)
subinvolution (sŭb-![]() n-vō-LOO-shŭn, p. 227)
n-vō-LOO-shŭn, p. 227)
taking-hold phase (p. 234)
taking-in phase (p. 234)
 http://evolve.elsevier.com/Leifer/maternity
http://evolve.elsevier.com/Leifer/maternity
The postpartum period, or puerperium, is the 6-week interval from childbirth to the return of the uterus and other organs to a prepregnant state. An arbitrary time frame divides the period into the immediate postpartum (first 24 hours), early postpartum (first week), and late postpartum (second to sixth weeks). Care during this time presents a challenge to nurses. With the short hospital stay, the time must be well planned to assist in maternal recovery, newborn care, family preparation, and intensive patient teaching. Many hospitals offer extended postpartum care by home visits, hospital outpatient clinic visits, and telephone communication to assist the woman and family during the postpartum recovery period (Clinical Pathway 12-1).
Goals of Postpartum Care
The main goals in postpartum care are to assist and support the woman’s recovery to the prepregnant state and identify deviations from the norm; educate the mother about her own self-care, newborn feeding, and newborn care; and promote bonding between the newborn and family. During the first 1 to 2 postpartum hours (i.e., the fourth stage of
Clinical Pathway 12-1
| Assessment | 1-8 Hours | 8-24 Hours | 24-48 Hours |
| Assessment | Assess q15 minute 1st hour; q30 minute 2nd hour then q4h: Fundus for firmness, level Lochia for color, amount, clots Bladder for voiding Perineum for sutures, bruising, hemorrhoids Breasts for softness, colostrum Vital signs (compare to baseline) Pain | Assess q4h: Fundus Breasts, nipples Newborn latch-on Colostrum Feeding technique for breast or bottle Vital signs (compare to baseline) Pain Homans’ sign Bonding Perineal healing Lochia | Assess: Breasts for softness, nipples, latch-on of newborn Feeding techniques and positioning Newborn care Hand hygiene Fundus q8h Perineal state Lochia Vital signs Family interaction |
| Teaching | Teach fundal massage, application of perineal pads, breastfeeding techniques. Discuss afterpains and pain management. Request assistance for first ambulation. Discuss orthostatic hypotension. | Explain cord care, bulb suctioning, circumcision care, newborn feeding techniques. Advise on maternal diet. Stress need for periods of rest. | Discuss: Maternal role Perineal care Newborn feeding Maternal diet Home setting and problems Support systems Plans to resume outside work Newborn care options Family planning Return of normal bowel function and the influence of medication on constipation |
| Medical and nursing interventions | Administer: Straight catheterization if unable to void Medications as ordered Stool softener if ordered Hep-Lock IV when taking oral fluids | Provide as needed: RhoGAM Hematocrit test Stool softener if no bowel movement Topical analgesics for sutures Medicine for pain Lactation nurse assistance | Provide shower and assistance with ambulation. Explain information and screening tests. Give return clinic appointments for mother and newborn. Assess bowel movements and diet. Provide discharge medication for pain, stool softener, lanolin for nipples. Provide community referral to WIC program if qualified. |
| Discharge and follow-up plan | Discuss understanding of postpartum care and newborn care. Identify support person and culturally specific needs. | Check that birth certificate is completed. Provide referral for birth records. Discuss home care. Discuss need for follow-up care for mother and newborn. Assess bonding. Discuss role of siblings and husband or partner. Administer immunizations if needed (e.g., Rubella). | Review discharge instructions for breast care, perineal care, family planning, newborn feeding, resumption of sexual activity, postpartum exercises, diet. Provide telephone resources. Review family and support system. Provide prescriptions as needed. Give appropriate gift pack and picture of newborn, as available. |
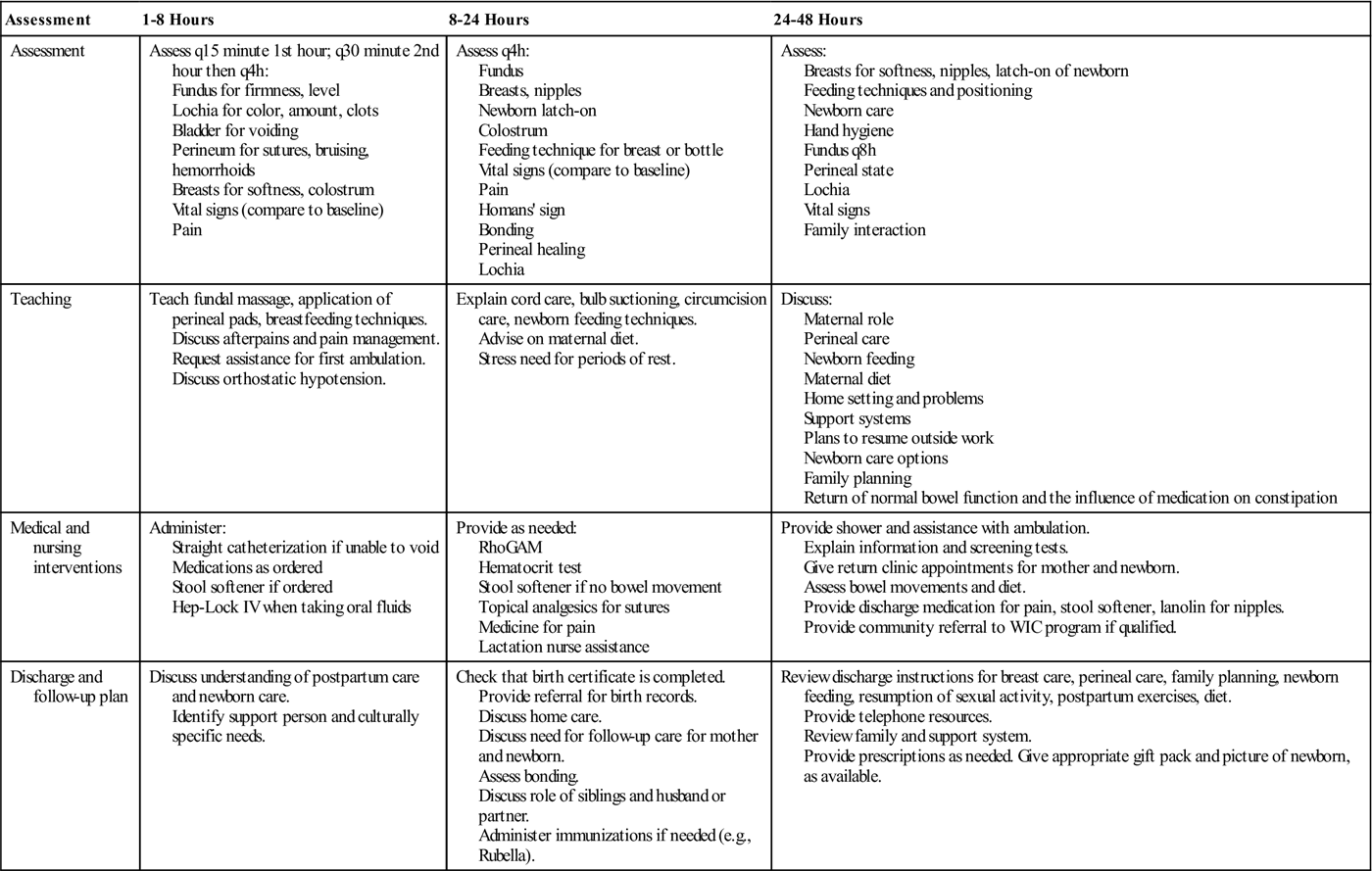
IV, intravenous; RhoGAM, Rho(D) immune globulin; WIC, Women, Infants, and Children.
labor), the woman is closely observed and assessed because it is a critical time to prevent the dangers of hemorrhage and hypovolemic shock. When her condition is stabilized, the woman may be moved to a postpartum unit.
To provide high-quality care, the nurse must be knowledgeable about the physical and emotional physiology of postpartum adaptation. After the initial dangers of hemorrhage and shock have passed, the primary postpartum danger is infection. The uterine cavity is easily accessible to microorganisms from the exterior. Also, the site where the placenta was attached is an open wound and can be easily infected.
The clinical pathway includes nursing assessments, teaching, medical and nursing interventions, discharge, and follow-up care for the postpartum woman. By indicating specific care and progress of the woman and newborn within a specified timeline that is related to a planned outcome, the nurse can clearly identify deviations from normal so they can be treated. The nurse documents the care and reports variation in progress during the postpartum period.
Physiologic Changes and Nursing Interventions
Changes in the Reproductive System
Involution of the Uterus
Involution refers to the changes that the reproductive organs (particularly the uterus) undergo after birth of the newborn to return to the pre-pregnant size and condition. The process begins after the expulsion of the placenta with uterine muscle contractions. Immediately after birth, the placental site contracts to a size less than half its original diameter. During contractions, the uterine muscles act like living ligatures and compress the blood vessels, which control and reduce the amount of blood loss (Figure 12-1). A unique healing process, called exfoliation, enables the placental site to heal without scarring. In exfoliation, necrotic tissue is sloughed off of the superficial tissues, leaving a smooth surface of endometrial tissue. This unique reparative process ensures that future fertilized ova will implant in an unscarred uterus. Endometrial regeneration is completed within 16 days (Oats & Abraham, 2010), except for the placental site, where regeneration is not complete until 6 weeks postpartum.
The uterus undergoes a rapid reduction in size and weight. The uterus weighs approximately 1000 g (2.2 lb) immediately after birth. It decreases to 500 g (1.1 lb) during the first week and 340 g (12 oz) by 2 weeks postpartum. The rate of decrease varies with the size of the newborn and the number of previous pregnancies. The primary cause of involution is the sudden withdrawal of estrogen and progesterone, which triggers the release of proteolytic enzymes into the endometrium. This release causes the protein material within the endometrial cells to be broken down into substances that can be excreted in the urine. The number of muscle cells does not change during involution, but the size of each cell is markedly reduced.
Factors that can slow uterine involution include (1) prolonged labor, (2) incomplete expulsion of placenta and membranes, (3) anesthesia, (4) previous labors, and (5) a distended (full) bladder. Factors that can enhance involution include (1) uncomplicated labor and birth, (2) breastfeeding, and (3) early, frequent ambulation.
The cervix after birth is soft. By 18 hours, it has regained its form. The cervical os (dilated to 10 cm during labor) gradually closes within 2 weeks. The external os never regains its original appearance; after childbirth, it appears as a slit instead of a circle.
Descent of the Uterine Fundus
Fundal height is measured in centimeters (or fingerbreadths) in relation to the umbilicus (Skill 12-1). It is used to assess the rate of uterine involution. The usual progression of uterine descent into the pelvis is 1 cm (about one fingerbreadth) a day. After delivery (especially when an oxytocin drug is
At 6 weeks after delivery, the uterus is approximately pre-pregnant size. Subinvolution is the failure of the uterus to return to the pre-pregnant state and is most commonly caused by retained placental fragments.
Afterpains
Intermittent uterine contractions, which represent relaxation and contraction of the muscle fibers, cause uterine cramping and are called afterpains. Afterpains occur for the first 2 or 3 days’ postpartum. The hormone oxytocin, released by the posterior pituitary gland, strengthens uterine contractions, compressing blood vessels and preventing excessive blood loss. If the mother breastfeeds, infant suckling stimulates oxytocin release. Therefore, the mother often notices the afterpains when she breastfeeds her newborn. Women who have had previous pregnancies often have stronger afterpains because the contraction of the uterine muscles is not sustained because of decreased muscle tone. Nonsteroidal antiinflammatory medications such as ibuprofen are more effective than acetaminophen or propoxyphene in relieving afterpains for most women (Gabbe, Niebyl, & Simpson, 2007). Ibuprofen is safe for nursing mothers (Gabbe, Niebyl, & Simpson, 2007).
Lochia
Lochia is postpartum vaginal discharge. It contains blood from the placental site, particles of necrotic decidua, and mucus. Lochia normally has a fleshy odor similar to that of menstrual flow. The quantity of lochia rapidly diminishes and becomes moderate and then scant. Lochia is the heaviest during the first 1 or 2 hours after birth. Initial lochia is bright red and commonly called lochia rubra (lasts 1 to 3 days); it may contain small clots. The vaginal flow then pales and becomes pink to brown after approximately 3 days; this is called lochia serosa. Lochia serosa should not contain clots and can last up to 27 days in some women (Gabbe, Niebyl, & Simpson, 2007). Typically, by 10 days’ postpartum, the vaginal discharge often becomes yellow to white and is called lochia alba. Lochia alba may continue, on average, to the sixth week postpartum (Table 12-1).
Table 12-1
Normal and Abnormal Characteristics of Lochia
| Lochia Type | Time | Normal Lochia | Abnormal Lochia |
| Lochia rubra | Days 1-3 | Bright red, bloody consistency; fleshy odor; temporary increase during breastfeeding and on rising | Numerous large clots; foul smell; saturation of perineal pad in 1 hour or less |
| Lochia serosa | Usually days 4-9 (can last to 27 days) | Pinkish brown; serosanguineous consistency | Foul smell; saturation of perineal pad in 1 hour or less |
| Lochia alba | Day 10 to approximately sixth week | Creamy white; fleshy odor | Foul smell; persistent lochial discharge over 3 weeks; return to pink or red discharge |

Estimating the amount of lochial flow by observation is difficult. Many facilities use perineal pads that have cold or warm packs in them. These pads absorb less lochia, which must be considered when estimating the amount of blood loss. If a mother has excessive lochia, a clean pad should be applied and checked within 15 minutes. The number of perineal pads applied during a given period should be counted or the pads weighed to help determine the amount of vaginal discharge. One gram of weight equals 1 mL of blood. In addition, the woman’s fundus should be checked for firmness. Nurses often estimate the amount of lochia in terms of the approximate size of the area soiled in 1 hour (Skill 12-2).
The amount of lochia is less after a cesarean birth. Breastfeeding or the use of oral contraceptives does not affect lochial flow. Lochia is briefly heavier when the mother ambulates because blood that has pooled in her vagina is discharged when she assumes an upright position. The gush of blood can be anxiety provoking to the woman and should not be confused with a postpartum hemorrhage. Excessive lochia rubra early in the postpartum period may suggest bleeding as a result of retained fragments of the placenta or membranes. Recurrence of bleeding in 7 to 10 days after birth suggests bleeding from the placenta site but may be the result of normal sloughing (Gabbe, Niebyl, & Simpson, 2007). After 3 to 4 weeks, late bleeding may also be caused by infection or subinvolution. Continued lochia serosa or alba suggests infection (endometritis) and is often accompanied by fever, pain, or abdominal tenderness and an offensive, foul odor to the lochia. Any abnormal lochia pattern should be documented and reported. Ultrasound is one of the diagnostic methods that can be used to confirm the cause of postpartum bleeding.
Assessment of uterine firmness, location, and position in relation to the midline (see Skill 12-1) is performed at routine intervals. A poorly contracted (soft, boggy) uterus should be massaged until firm to prevent hemorrhage. It is essential not to push down on an uncontracted uterus to avoid inverting it.
Vagina
The vagina usually appears edematous and bruised, and the opening in the vagina often gapes when intraabdominal pressure is increased, such as by
coughing. By the third postpartum week, the vagina resumes the appearance of the pre-pregnant state, with some relaxation of tissue. The rugae, or vaginal folds, disappear during pregnancy, and the walls of the vagina become smooth. The rugae reappear within 3 weeks postpartum. Within 6 weeks, the vagina has almost regained its pre-pregnancy form. Breastfeeding mothers, in particular, may have vaginal dryness and discomfort during sexual intercourse. A water-soluble vaginal lubricant such as K-Y Jelly makes intercourse more comfortable. Dryness usually disappears when ovulation and menstruation return.
Perineum
The perineum has been stretched and thinned to accommodate the size of the newborn. The pelvic floor muscles are overstretched and weak. The appearance of the perineum varies greatly, depending on the type and extent of the laceration(s) or episiotomy (cut in the perineum). The soft tissues of the perineum are often edematous and bruised.
The nurse puts on clean gloves before assessing the perineum to prevent contact with vaginal blood flow. The perineum is assessed for the type and amount of vaginal discharge, unusual swelling, discoloration, healing of the tissues, and discomfort (Skill 12-3). If an episiotomy was performed, the state of healing is assessed by the REEDA scale, a mnemonic for Redness, Edema, Ecchymosis (bruising), Discharge, and Approximation of the wound. Foul odor accompanied by drainage indicates infection; further examination of the incision and area of warmth and tenderness should be performed. Hemorrhoids, if present, are assessed for size, number, and discomfort. During the assessment, the nurse asks the woman about relief obtained from comfort measures (sitz bath, warm or cold applications, and medications). The nurse should record his or her findings.
Studies have shown a positive response to cold sitz baths (Gabbe, Niebyl, & Simpson, 2007). Occasionally, the cause of perineal pain is prolapsed hemorrhoids. Witch-hazel pads, astringent pads, suppositories, or local anesthetic sprays are helpful. Healing usually takes place within 6 weeks. Daily perineal care is described in Skill 12-4.
Changes in the Musculoskeletal System
Muscles and Joints
During the first few days, levels of the hormone relaxin decrease and ligaments and cartilage of the pelvis begin to return to the pre-pregnancy state. With the delivery of the placenta, the effect of progesterone on muscle tone is removed. Therefore, muscle tone begins to be restored throughout the body. In particular, the
tone in the rectus abdominis muscles and the pubococcygeal muscle is restored. The abdominal muscles, including the rectus abdominis muscles, may be separated, and diastasis recti can occur (Figure 12-2). Special exercises can strengthen the abdominal wall. Women need to be advised that with proper diet, exercise, and rest, the abdominal muscle tone is usually regained more rapidly. Good body mechanics and correct posture are important to help relieve low back pain. Kegel exercises help the pubococcygeal muscle (muscle that aids bowel and bladder control) to regain normal function (see Chapter 5).

A generalized decrease in bone mineralization occurs after birth. This bone loss is not affected by calcium intake or exercise but returns to normal within 18 months (Gabbe, Niebyl, & Simpson, 2007).
Lower Extremities
Venous stasis, particularly during the later part of pregnancy, contributes to the risk of blood clots (thrombosis) forming in the lower extremities. By passively dorsiflexing the woman’s feet, the nurse determines whether there is pain in the calf (a positive Homans’ sign) (Figure 12-3). This may be an early sign of venous thrombosis and should be reported. In addition, the nurse inspects the legs for redness, swelling, and warmth.
Changes in the Cardiovascular System
Dramatic changes to the maternal cardiovascular system occur in the postpartum period. During pregnancy, an approximately 50% increase in circulating blood volume occurs (hypervolemia), which allows the woman to tolerate considerable blood loss at birth without adverse effects. Many women lose at least 200 to 500 mL of blood during vaginal births and approximately twice as much during cesarean births. Readjustments in the maternal vasculature after childbirth are rapid. During postpartum adaptation, dramatic and immediate changes take place in the circulating blood volume that prevent hypovolemia from normal blood loss during delivery. These changes include (1) elimination of the placenta, which diverts 500 to 750 mL of blood flow into the maternal systemic circulation; (2) rapid reduction of the size of the uterus, which puts more blood in the systemic circulation; (3) increase of blood flow to the vena cava from elimination of compression by the gravid uterus; and (4) mobilization of body fluids accumulated during pregnancy. Cardiac output may remain increased for 1 year or more (Gabbe, Niebyl, & Simpson, 2007). A healthy woman’s body can make these changes, but a woman with a heart disorder can encounter problems.
Excess blood volume, which is necessary during pregnancy, is removed to help the woman’s body return to the pre-pregnant state. This excess is disposed of in two ways: (1) diuresis (increased excretion of urine), in which a daily urinary output can be as much as 3000 mL; and (2) diaphoresis (profuse perspiration).
Blood Values
During the first 72 hours after childbirth, the loss in plasma volume is greater than that in the number of red blood cells (RBCs). This results in a temporary rise in the hematocrit and hemoglobin levels. Any excess will gradually disappear in accordance with the RBC life span. The normal levels are achieved within 2 to 4 weeks’ postpartum. The excess body fluids are excreted by the kidneys, which cause a marked increase in daily urinary output. Leukocytosis, an increase in the white blood cell count to 15,000/mm3 or more, occurs immediately after birth in women without infection; the levels return to normal within 10 days.
Blood Coagulation
Blood clotting factors that increased during pregnancy tend to remain elevated during the initial postpartum period. Fibrinogen levels may return to normal within 2 weeks of delivery. This fact, along with trauma, immobility, and infection, predisposes the woman to the development of a thromboembolism (one of the leading causes of maternal death is an embolus or thrombus). To decrease this risk, early and frequent ambulation is essential. Dyspnea (difficulty breathing) and tachypnea (rapid breathing) are hallmark signs of pulmonary embolus and require immediate medical intervention.
Varicose veins that have developed during pregnancy usually diminish during the puerperium because the venous stasis that was caused by the gravid uterine compression (pressure of the uterus on pelvic blood vessels) decreases. In addition, progesterone level is decreased, which during pregnancy is largely responsible for a decrease in smooth muscle tone.
Orthostatic Hypotension
Resistance to the blood flow in the vessels of the pelvis decreases after birth. As a result, the woman’s blood pressure falls when she sits upright or stands, and she may complain of feeling dizzy, lightheaded, or faint. Guidance and assistance are needed during early ambulation to prevent injury.
Postpartum Diaphoresis
Diaphoresis (perspiration) is the elimination of excess fluid through the skin. It is the body’s way of getting rid of excess fluid accumulated during pregnancy. Profuse diaphoresis (excessive sweating) often occurs at night. This adjustment has implications for nursing care. Showers, frequent changes of clothing, and adequate fluid intake are important for the woman’s comfort.
Vital Signs
Temperature
The woman’s temperature during the first 24 hours after delivery may rise to 38° C (100.4° F) as a result of the dehydration and exertion of labor. After the first 24 hours, the woman should be afebrile, and any temperature greater than 38° C suggests infection. An elevated temperature that persists longer than 24 hours or that exceeds 38° C should be reported to the physician or nurse-midwife. A short-term elevation on the second or third postpartum day can occur as a result of breast engorgement.
Pulse
The heart rate often decreases to a rate of 50 to 60 beats/min (bradycardia, or slow pulse) for the first 6 to 8 days’ postpartum. An elevated heart rate may indicate undue blood loss, infection, pain, anxiety, or cardiac disease.
Blood Pressure
Blood pressure readings should remain stable after birth. A decrease in blood pressure may be related to excessive blood loss. Blood pressure elevation—especially when accompanied by a headache—suggests gestational hypertension and indicates the need for further evaluation (see Chapter 13).
Changes in the Urinary System
The bladder of the postpartum woman has increased in capacity and has lost some of its muscle tone. In addition, during the birth, the urethra, bladder, and tissue around the urinary meatus may become edematous and traumatized. Urination is also impeded by anesthetic drugs. The diminished awareness of the need to urinate may result in decreased sensitivity to fluid pressure, and the woman may not feel an urge to void. This is important to remember because the bladder fills rapidly as a result of intravenous fluids administered during labor and after birth. With bladder distention, the uterus is displaced (often over to one side, usually the right) and has a reduced ability to contract. When the uterus fails to contract, blood vessels are free to bleed. Therefore, it is important that the nurse monitor the woman for voiding. The urinary output in the early postpartum period can be great (diuresis). Tenderness over the costovertebral angle, fever, urinary retention, and dysuria with urinary frequency signify potential urinary infection, and further evaluation is necessary. Glomerular filtration may remain elevated for up to 8 weeks postpartum.


 Skill 12-1
Skill 12-1

 Skill 12-2
Skill 12-2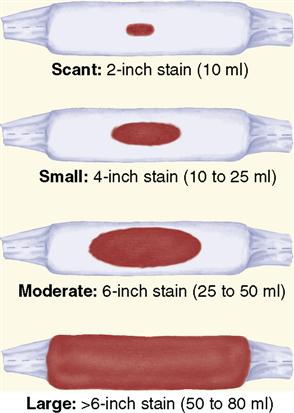
 Skill 12-3
Skill 12-3 Skill 12-4
Skill 12-4




