Nursing research is the road map to professional practice.
After completing this chapter, you should be able to:
• Define evidence-based practice.
• Understand the importance of evidence-based practice.
• Identify the steps in evidence-based practice.
• Explore the process of research utilization.
• Identify the steps in the process of research utilization.
• Discuss the difference between conducting research and research utilization.
• Identify resources for evidence-based nursing practice.
• Identify the characteristics of your practice context.
• Describe ways in which nursing research can be used to guide your nursing practice.
• Describe the function of the National Institute of Nursing Research.
What is Evidence-Based Practice?
Evidence-based practice (EBP) “is a problem solving approach to clinical practice that integrates: a systematic search for and critical appraisal of the most relevant evidence to answer a burning clinical question, one’s own clinical expertise, and patient preferences and values” (Melnyk & Fineout-Overholt, 2005, p. 6). Historically health care and more specifically, nursing care, was based on tradition. In other words, we simply replicated what had been previously done in nursing, without question to the support of evidence for what we were doing or the impact on patient outcomes. As nursing has evolved and the expectation for continually improving patient outcomes has come to the forefront, a greater emphasis has been placed on implementing nursing care that is supported through the use of the best research available. Evidence-based practice incorporates many additional sources of data that may contribute to improved nursing care.
Evidence-based practice goes beyond nursing research in considering other sources of documentation that may improve nursing care. Research published by other disciplines is included (e.g., medical research and social research), as well as nonresearch data that may contribute to practice (e.g., financial data and clinical experts). This is prudent at a time when the complexity of health problems is increasing, and the discovery of new data is more rapid than ever before (Research for Best Practice Box 24.1).
The U.S. Department of Health and Human Services has established evidence-based practice centers and clinical practice guidelines that are available through the Internet. These resources include the most current information on completed evidence reports and practice guidelines as well as those that are in progress (see http://www.ahrq.gov/research/findings/evidence-based-reports/overview/index.html and http://www.ahrq.gov/professionals/clinicians-providers/guidelines-recommendations/index.html). However, not all aspects of practice have been evaluated to date. Therefore, the decision to implement an evidence-based practice protocol that does not have a formal report requires a dedicated commitment on the part of all those involved. The steps in applying evidence-based practice include definition of the problem; identifying, reviewing, and evaluating the data applicable to the problem; designing a practice change based on the data; and implementing the change in nursing practice, while recognizing the nurse’s experience and patient preferences (see Relevant Websites and Online Resources).
Step 1: Define the Problem
As nursing professionals who will be responsible for implementing an EBP protocol with the goal of improving patient outcomes, we must first recognize and fully define the problem.
Step 2: Identify, Review, and Evaluate the Data Applicable to the Problem
Nurses must be able to locate and evaluate research studies that will serve as the foundation of any potential EBP protocol. The specific nursing practice that will be changed, in addition to the practice context, will determine the types of data included for review.
Step 3: Design a Practice Change Based on the Data While Incorporating the Clinical Expertise of the Nurse and Patient Preferences
Prepare a written plan for the new nursing practice. The plan needs to be consistent with your practice context to be effective. For maximum benefit, the plan will also require the consensus of those who will implement it.
Step 4: Implement the Change in Nursing Practice
Move the new plan into nursing practice on a defined schedule. Staff in-services may be required so that those involved can fully understand the change. Monitor and evaluate the implementation process. Moreover, as noted by Melnyk and Fineout-Overholt (2005), EBP must recognize the great experience that nurses bring to the practice setting and patient input and preferences if successful implementation is to be realized (Fig. 24.1).
Now let’s consider using the evidence-based practice process in a hypothetical situation.
Mario works in an intensive care unit in which many of the patients require mechanical ventilation. At a recent staff meeting, Mario and his co-workers learned that their unit’s rate of ventilator-associated pneumonia (VAP) was greater than rates in many other hospitals. Concerned by this, Mario volunteered to work on this project. He began with a review of the literature. Using a nursing literature database, Mario was able to find a number of research studies conducted in the past few years that examined the same issue. Additionally, he found that multiple professional organizations had issued evidence-based guidelines to reduce the occurrence of ventilator-associated pneumonia. After reading these articles, Mario drafted a set of clinical practice guidelines based on these articles that reflected the unique needs of his unit and its patient population. Mario then presented his guidelines to the nursing staff and provided short educational in-service sessions on their application. The staff agreed to adhere to these new practice guidelines for a period of 3 months. At the end of that time, they would compare their incidence of VAP using the new clinical guidelines with the incidence of VAP using the old clinical guidelines.
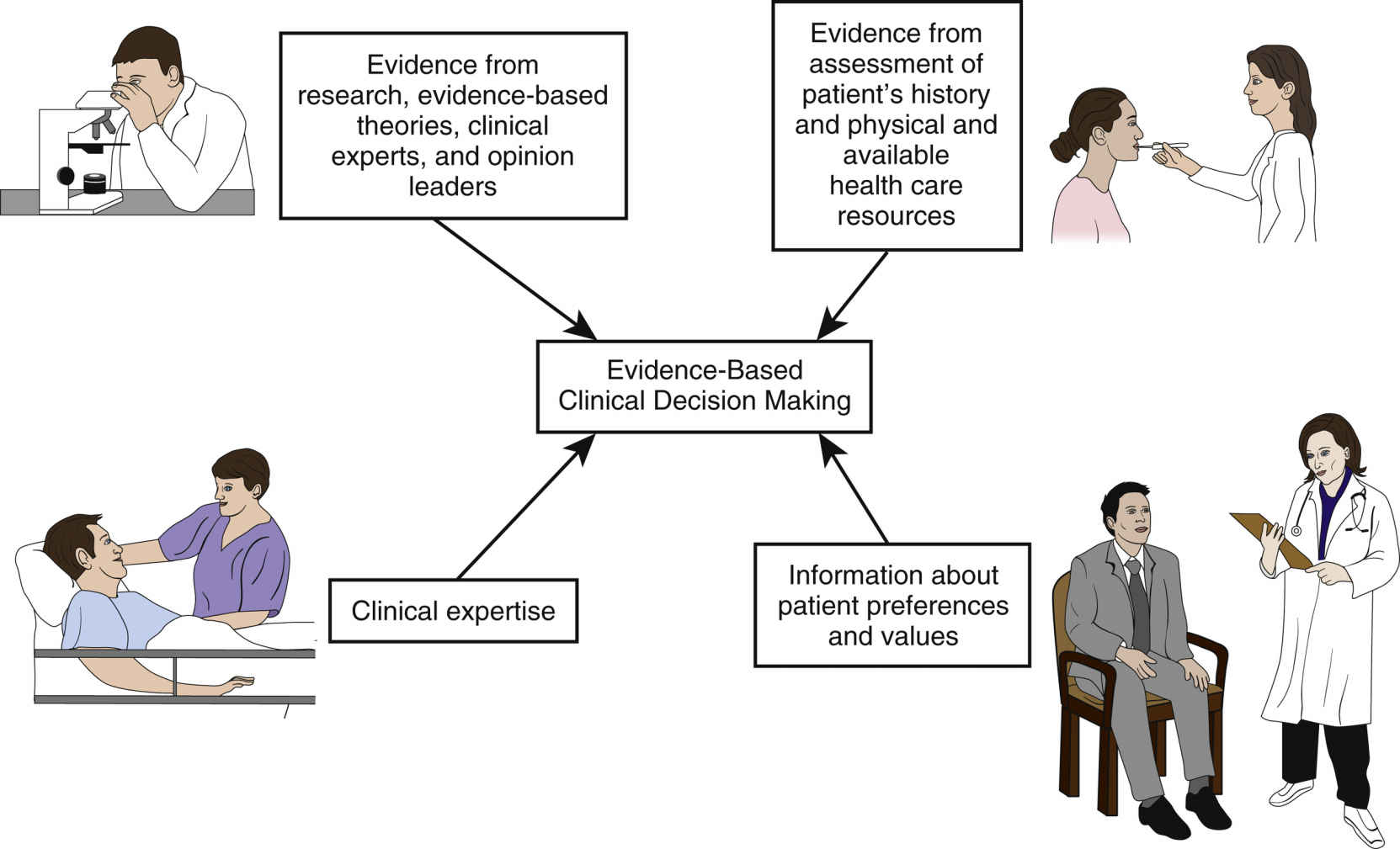
FIG. 24.1 Model of evidence-based clinical decision making. Reprinted with permission from Potter, P. A., Perry, A. G., Stockert, P. A., Hall, A. M., & Ostendorf, W. R. (2017). Fundamentals of nursing (9th ed.). St. Louis: Elsevier, p. 53.
At the end of the 3-month period, Mario and his co-workers were pleased to find a significant decrease in the occurrence of VAP among their patients. Working with nursing administration, Mario’s proposed clinical practice guidelines became the new standard of care on his unit.
The Need for Nursing Practice Based on Research
In the recent past, there has been a continuing increase in costs associated with the delivery and receipt of health care in the United States. At the same time, there has been more and more scrutiny of how those health care dollars are spent. The decision of which health care treatments receive funding from health care insurance is now based primarily on documentation of favorable patient outcomes. In addition, patients want to know that the dollars they spend on health care will help them to get well and feel better—they want to purchase something that works for them. Nurses must be able to demonstrate that the nursing care they provide is cost-effective and improves the health of patients. As we continue to move to a health care setting that recognizes the importance of patient care that utilizes the most current and appropriate evidence, we must understand how research utilization will assist us in meeting the goal of improving patient outcomes through EBP.
What is Nursing Research Utilization?
The ability to transfer research into clinical practice is essential for ensuring quality in nursing. The process of research utilization involves transferring research findings to clinical nursing practice. In the process of research utilization, the emphasis is on using existing data (findings or evidence) from previous nursing research studies to evaluate a current nursing practice. A major component of the process is reviewing completed nursing research studies that have been published in the literature. In contrast, conducting new research involves the collection of new data to answer a specific clinical practice question. Nursing research utilization is a step-by-step process incorporating critical thinking and decision making to ensure that a change in practice has a sound basis in nursing science.
What Are the Steps for Nursing Research Utilization?
Step 1: Preutilization
The first step in the application of nursing research to nursing practice is the recognition that some aspect of nursing practice could be done in a safer, more efficient, more beneficial, or simply a different way. This begins an exploratory phase in which nursing colleagues in the practice setting are consulted regarding their opinions about the need to find a new approach for some aspect of nursing practice. An early question should be: “Is the current practice research based?” When current practice is research based, the next question should be “Is the research on which the practice is based current?” (e.g., the specific details of taking temperatures with mercury thermometers became outdated when digital thermometers were used exclusively in practice).
A second phase of Step 1 is consensus building, which is used to identify the specific practice to be changed. In this phase, the incorporation of the principles of change theory will increase the possibility of success. (See Chapter 10 for information about the challenges of change.) In any practice setting in which there are several nurses, a change will be more acceptable if those affected are included in the decisions related to the change. Clear communication and teamwork are essential elements of this process. Group consensus is crucial for the successful application of research findings.
The third and final phase of Step 1 delineates the aspect of nursing practice that will be changed into a concise statement of the practice problem. This statement will answer the question, “In our current nursing practice, what do we want to change, improve, or make more efficient?” The narrower and more specific the statement of the practice problem, the easier your task will be in Step 2.
Step 2: Assessing
The second step in research utilization is the identification and critical evaluation of published research that is related to the practice problem you have identified (Fig. 24.2). Nursing literature is searched to identify those studies that address your practice problem. Although some studies may have explored the exact practice problem that you are examining, it is likely that most research will have approached the problem from a different point of view. Your task will be to analyze and critically evaluate the research reports to determine which findings are adaptable to your practice problem and context.
While reviewing the literature for research reports that have examined your practice problem, it is essential that the research reports you are reviewing are peer-reviewed to ensure credibility. Peer-reviewed or refereed research studies are different from popular sources and non–peer-reviewed research reports, in that the research manuscript is submitted to a scholarly journal where it is reviewed by a panel of experts (peer reviewers or referees) in that respective field or area of study. An editorial board that is not expert in the content area under study typically reviews non–peer-reviewed reports (e.g., editorials, newsletters, opinion statements). Additionally, peer-reviewed articles have a designated manuscript format, which includes an abstract, research problem/objective, methodology, data collection, discussion, conclusion, and references; whereas non–peer-reviewed or popular/trade journals do not ascribe to a specific formatting style (NCSU Libraries, 2014). So, you might be asking yourself, “What does the peer-review process involve and what are my chances of publishing a research report in a peer-reviewed journal?” North Carolina State University (NCSU) offers an overview of the peer-review process via an online video available at http://www.lib.ncsu.edu/tutorials/peerreview/.
FIG. 24.2 Nine out of ten nurses recommend….

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




