CHAPTER 25 Toxicologic Emergencies
Toxicologic emergencies include acute poisonings and intake of substances of abuse. These situations pose a unique challenge to the emergency department nurse. The American Association of Poison Control Centers annual report for 2004 stated that 92.7% of cases occurred in the home, with 51.3% occurring in children younger than 6 years and 38.5% involving children younger than 3 years of age. In addition, it was noted that 94% of toxic exposures were acute and 84.1% were unintentional. Therapeutic medication errors, such as double dosing or taking the wrong medication, accounted for more than 10% of all poisonings.1 Ingestion or coingestion of over-the-counter (OTC) drugs such as antihistamines, antidiarrheals, or indigestion remedies in potential poisoning situations may cloud or mask true symptoms of acute poisoning. In 2004, nearly 1.3 million emergency department visits were associated with drugs of abuse or misuse, including prescription and OTC drugs, inhalants, and illicit drugs.2 Patients may also use more than one drug in combination, with resulting polysubstance abuse, or may ingest a substance in combination with alcohol, thus leading to fatalities.
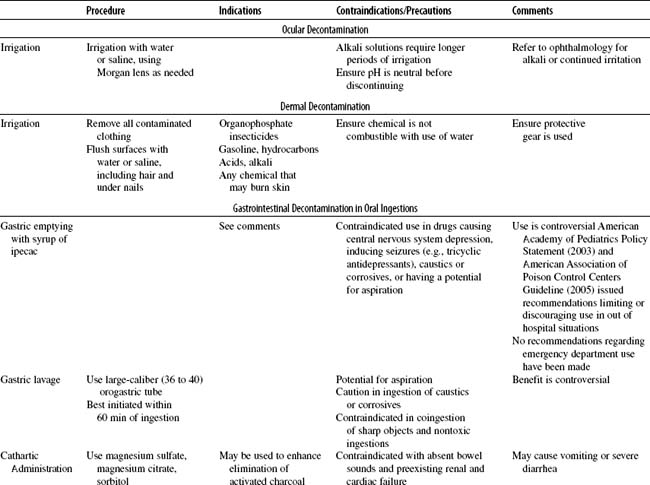
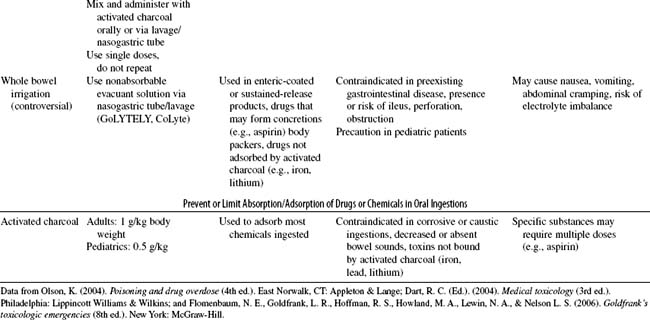
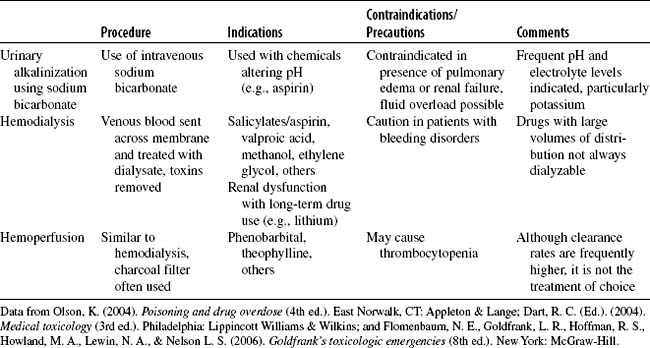
Treatment is directed toward preventing or decreasing absorption of the toxic substance (Table 25-1). This can be accomplished using measures to enhance elimination of the substance (Table 25-2) or by administering specific antidotes to counteract the toxic substance (Table 25-3).
| Antidote | Poisoning |
|---|---|
| N-acetylcysteine | Acetaminophen (Tylenol) |
| Mucomyst (oral formulation) | |
| Acetadote (intravenous formulation) | |
| Atropine | Organophosphate, carbamate insecticide |
| Bradycardia caused by toxins | |
| Antivenins | |
| Polyvalent Equine | Rattlesnake, copperhead envenomation |
| Polyvalent Immune Fab-Ovine/Cro-Fab | Rattlesnake, copperhead envenomation |
| Black Widow Spider | Black widow spider bite |
| Dimercaprol (BAL in Oil) | Heavy metal |
| Botulinum antitoxin | Botulism |
| Calcium chloride or gluconate | Calcium channel blocker, hydrofluoric acid: skin exposure or poisoning, hypocalcemia |
| Cyanide antidote kit | Cyanide |
| Deferoxamine | Iron |
| Dextrose | Hypoglycemia caused by toxins |
| Digoxin Fab | Digoxin, oleander |
| DMSA (Succimer) (Chemet) | Heavy metal (especially lead, mercury) |
| Edetate disodium, D-Penicillamine | Heavy metal |
| Ethanol intravenously 10% | Ethylene glycol, methanol |
| Flumazenil (Romazicon) | Benzodiazepine |
| Folic acid | Methanol |
| Fomepizole (4 MP) (Antizol) | Ethylene glycol, methanol |
| Glucagon | Beta-blocker, calcium channel blocker |
| Methylene blue | Methemoglobinemia |
| Naloxone (Narcan) | Narcotic overdose |
| Oxygen, hyperbaric oxygen | Carbon monoxide |
| Octreotide (Sandostatin) | Oral sulfonylurea hypoglycemia |
| Physostigmine/Antilirium | Anticholinergic |
| Pralidoxime (2-PAM) (Protopam) | Organophosphate |
| Protamine | Heparin |
| Pyridoxine | Isonicotinic acid hydrazide (INH), ethylene glycol |
| Prussian blue | Thallium, radioactive cesium |
| Sodium bicarbonate | Sodium channel blockers, alkalinization of urine or serum |
| Sodium thiosulfate | Cyanide |
| Thiamine | Ethylene glycol, Wernicke’s syndrome, Gyromitra mushrooms, hydrazine |
| Vitamin K | Warfarin (Coumadin), warfarin-based rodenticides |
Data from Tintinalli, J. E., Kelen G. D. & Stapczynski J. S. (Eds.). (2003). Emergency medicine: A comprehensive study guide (6th ed.). New York: McGraw-Hill; Olson, K. (2004). Poisoning and drug overdose (4th ed.). East Norwalk, CT: Appleton & Lange; and Poisondex System (Internet database). Greenwood Village, CO: Thomson Micromedex. Available at www.thomsonhc.com. Updated periodically.
I. GENERAL STRATEGY
A. Assessment
1. Primary and secondary assessment/resuscitation (see Chapter 1)
B. Analysis: Differential Nursing Diagnoses/Collaborative Problems
C. Planning and Implementation/Interventions
F. Age-Related Considerations
II. SPECIFIC TOXICOLOGIC EMERGENCIES
A. Alcohol Use
2. Analysis: differential nursing diagnoses/collaborative problems
3. Planning and implementation/interventions
4. Evaluation and ongoing monitoring (see Appendix B)
B. Opiate Use
2. Analysis: differential nursing diagnoses/collaborative problems
3. Planning and implementation/interventions
4. Evaluation and ongoing monitoring
C. Cocaine Use
Cocaine is one of the most popular drugs of abuse. “Snorting” or intranasal use is the most common route of administration; however, it can be smoked or injected. “Crack,” “Rocks,” or free-based smokeable cocaine is more purified, it gives the user a “rush” similar to IV use, and it has a higher addiction potential. Cocaine stimulates the CNS and autonomic nervous system to increase the release of catecholamines from the adrenergic nerve terminals. It blocks the reuptake of dopamine and norepinephrine, thereby resulting in increased motor activity, insomnia, and euphoria. Patients seen in the emergency department for cocaine use are there predominantly for management of secondary complications. Treatment is aimed at supportive corrective measures. Medicinally, cocaine is used as an anesthetic and a vasoconstrictor in nasal surgery.
2. Analysis: differential nursing diagnoses/collaborative problems
3. Planning and implementation/interventions
4. Evaluation and ongoing monitoring (see Appendix B)
D. Amphetamine Use
Amphetamines are synthetic sympathomimetic drugs that stimulate the CNS and produce a feeling of excess energy. They are commonly used to suppress appetite, elevate mood, stay awake, and control symptoms of attention-deficit disorder. Amphetamines are available in oral, intranasal, or parenteral forms. Crystalline rock forms such as “ice” are smoked. “Body packers” are seen in the emergency department as a result of swallowing packages, condoms, or rocks while either transporting the drugs or evading police pursuit. Common amphetamines include crystal methamphetamine, dextroamphetamine, and methylphenidate (Ritalin). Recently, fenfluramine (Redux), the weight reduction medication, was withdrawn from the market because of its side effects, which included pulmonary hypertension and valvular heart disease.
2. Analysis: differential nursing diagnoses/collaborative problems
3. Planning and implementation/interventions
4. Evaluation and ongoing monitoring (see Appendix B)
E. Lysergic Acid Diethylamide Use
2. Analysis: differential nursing diagnoses/collaborative problems
3. Planning and implementation/interventions
4. Evaluation and ongoing monitoring (see Appendix B)
F. Phencyclidine Use