CHAPTER 11 Cardiovascular Emergencies
I. GENERAL STRATEGY
A. Assessment
1. Primary and secondary assessment/resuscitation (see Chapter 1)
C. Planning and Implementation/Interventions
F. Age-Related Considerations
II. SPECIFIC MEDICAL CARDIOVASCULAR EMERGENCIES
A. Acute Coronary Syndromes
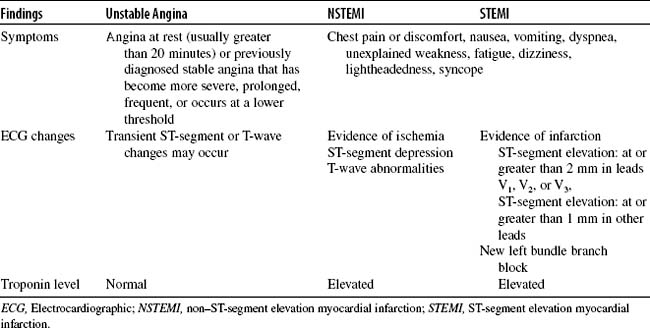
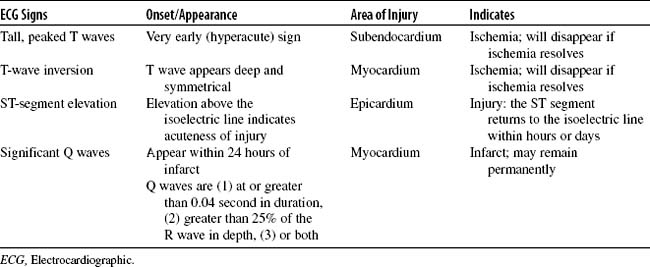
Regardless of the initial cause, if the myocardial oxygen supply-demand imbalance is severe or persistent, ischemia will produce irreversible cellular damage. The subsequent impact on myocardial contractility, stroke volume, and ventricular function will depend on the duration of ischemia, the extent of myocardial tissue involvement, and the patient’s preexisting cardiac status. Myocardial ischemia also stimulates catecholamine release, which increases peripheral vascular resistance, promotes tachycardia, and raises both preload and afterload. This increased demand on an infarcting myocardium can be overwhelming. Because many other conditions produce symptoms similar to those of ACS, careful examination and history taking are essential. Differential diagnoses include esophageal spasm, gastroesophageal reflux disease, biliary colic, chest wall pain, pericarditis, pulmonary embolism, aortic dissection, and cardiac dysrhythmias. Because each of the three ACSs is produced by the same underlying disease process, these syndromes are distinguished physiologically only by the extent of myocardial injury. Risk factors, assessment parameters, and many interventions are identical for all patients with ACS. Additionally, ACSs are currently an area of intense research; assessment and treatment recommendations change frequently. The development and implementation of a protocol or algorithm for care of the patient with ACS can help streamline the approach to this population (Fig. 11-1).
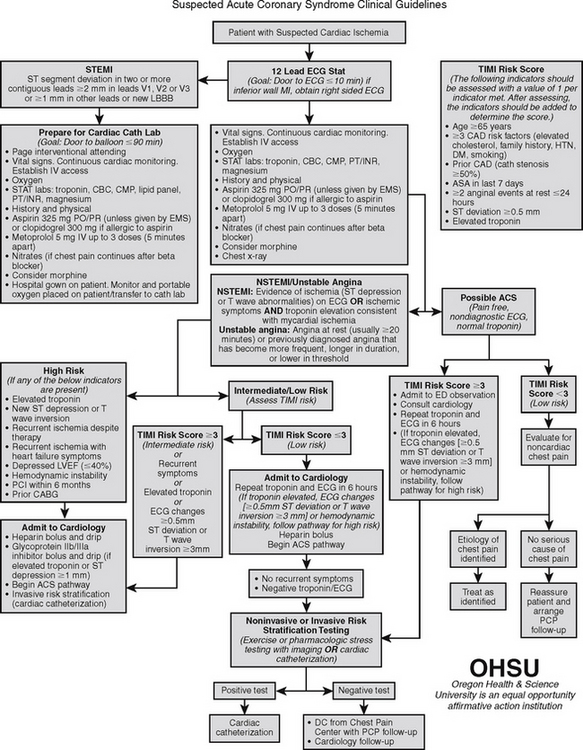
FIGURE 11-1 Acute coronary syndrome clinical guidelines.
(Modified from Cigarroa, J., MD, Davies, C., MD, & Johnson, K., RN MS CNS CCRN, Oregon Health & Science University, Portland, Oregon.)
2. Analysis: differential nursing diagnoses/collaborative problems
3. Planning and implementation/interventions
4. Evaluation and ongoing monitoring (see Appendix B)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree