CHAPTER 18
Thoracic Outlet Syndrome
Tiffany Street
First Edition Author: Catherine Wiegand
OBJECTIVES
1. Define thoracic outlet syndrome.
2. Differentiate between neurogenic, arterial, and venous symptoms.
3. Discuss conservative medical management and surgical intervention for treatment of thoracic outlet syndrome.
4. Identify nursing implications relevant to patients with thoracic outlet syndrome.
Introduction
Thoracic outlet syndrome (TOS) is a complex set of symptoms caused by abnormal compression of the neurovascular bundle in the thoracic outlet area. Entrapment of the neurovascular structures in the past has been described by a series of names, such as costoclavicular compression, hyperabduction syndrome, cervical rib syndrome, and first rib syndromes. Peet coined the term ‘‘thoracic outlet syndrome’’ in 1956 to indicate all compressions of the neurovascular bundle (Urschel & Razzuk, 1998). The name itself may be confusing because the area of compression between the scalene muscles and the first rib is correctly called the thoracic inlet. Currently, however, the term ‘‘thoracic outlet syndrome’’ is used to describe patients with compression of the subclavian vein, subclavian artery, and brachial plexus which are the three components of the thoracic outlet area. Compression usually occurs as a result of congenital or acquired changes in the surrounding bony or soft tissue. There are three major classifications of TOS: neurogenic, arterial, and venous.
The most common form of TOS is neurogenic and accounts for 95% of all TOS patients. These patients are usually young adults, and women predominate at approximately a ratio of 4:1 to men. Arterial TOS is rare and occurs in less than 5% of patients. Venous TOS is also uncommon and occurs in 2% to 3% of patients. These patients frequently present with a thrombotic event. Venous presentation is often a result of congenital anomalies of the costoclavicular space and a result of repetitive activities such as overhead shoulder movements, throwing, or swimming (Sanders, 2010).
The wide variability of patient symptoms, including vascular and neural signs, diffuse symptoms, and the lack of diagnosis-specific tests to confirm the diagnosis of TOS make it difficult to diagnose correctly. Patients may present with a variety of signs and symptoms rather than one specific symptom. Symptoms may be neurogenic, arterial, venous, or mixed (Stoney & Cheng, 1995).
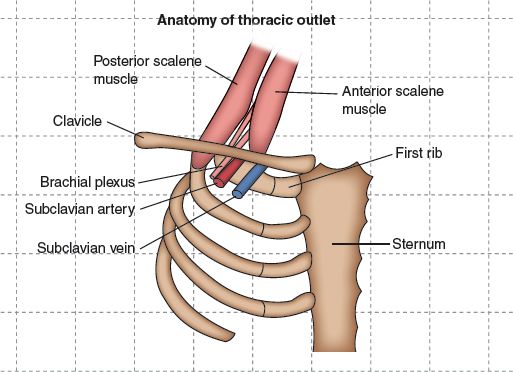
FIGURE 18.1 Anatomy of the thoracic outlet.
 I. Anatomy (Fig. 18-1) (Atasoy, 1996; MacKinnon & Novak, 2002; Stoney & Cheng, 1995)
I. Anatomy (Fig. 18-1) (Atasoy, 1996; MacKinnon & Novak, 2002; Stoney & Cheng, 1995)
A. First Rib forms the floor of the outlet. This rib is relatively flat, approximately 3 in long, with two transverse processes on the anterior surface. Located between the two groves is a tubercle for the attachment of the scalenus anticus muscle. The first rib forms the framework to which muscles and ligaments attach.
B. Clavicle with the Subclavius muscle forms superior portion.
C. Scalene Muscles are secondary respiratory muscles and raise the first rib and slightly rotate and bend the neck.
1. Scalenus anticus (anterior scalene muscle) muscle originates from the anterior tubercles of the transverse processes of C3 to C6 and inserts in the scalene tubercle on the first rib.
2. Scalenus medius (middle scalene muscle) muscle is the largest and longest and originates from the posterior tubercles of the transverse processes of the last six cervical vertebrae. It inserts inferiorly between the subclavian artery groove and the tubercle on the first rib. It is in close proximity to the posterior brachial plexus.
3. Scalenus minimus, if present (30% to 50%), arises from the transverse process of C6 to C7 and inserts in the fascial support of the pleura and first rib.
D. Neurovascular Bundle
1. Subclavian artery exits the chest by arching over the first thoracic rib posterior to the scalene anticus and anterior to the scalenus medius muscle. It lies just anterior to the brachial plexus.
2. Subclavian vein normally passes anterior to the scalene anticus and through the costoclavicular space between the first rib and the head of the clavicle.
3. Brachial plexus forms from the nerve roots C5 to T1. It gains access to the axilla by passing posterior to the anterior scalene muscle in close association with and superior to the subclavian artery. C8 and T1 nerve roots, which contribute to the medial cord and ulnar nerve, are commonly affected by pressure of the underlying first rib.
E. Cervical Bands (congenital myofascial bands/ligaments)
1. Can extend from the transverse process of C7 or from the tip of a cervical rib and attach to the scalene tubercle of the first rib.
2. Composed of posterior fibers of the anterior scalene and medial fibers of the middle scalene muscle, which lie either with the body of the scalenus medius or on the anterior surface of the muscles.
3. David B. Ross, MD has classified extensively up to nine separate types of bands, the most common of which are as follows:
a. Type 3 (the most common), which is critical in compression of C8 and T1 branches of the brachial plexus.
b. Type 5 (the second most common), which may have its lower insertion in the first rib.
c. Type 4 (less commonly seen), which is a powerful band capable of compressing both nerve and artery.
F. Cervical Ribs
1. If a cervical rib is present, the brachial plexus may be displaced and impinge on the apex of the interscalene triangle.
2. Can be a natural anomaly that may be a complete bony structure or a fibrous band that stretches to the first rib from the cervical transverse process.
3. Cervical ribs occur in approximately 0.45% to 1.5% of the general population and up to 5% of patients with TOS (Sanders, 2010).
4. Female to male ratio is approximately 2:1 (Kieffer & Ruotolo, 1995).
G. Sites of Compression
1. Interscalene triangle bordered by the anterior scalene muscle, the middle scalene muscle, and first rib inferiorly. The subclavian artery and the three trunks of the brachial plexus traverse this space. The middle scalene muscle is a key factor in neurogenic compression.
2. Costoclavicular space bordered by the clavicle, first rib with the costoclavicular ligament anteriorly, and the edge of the middle scalene muscle posteriorly. The subclavian artery, vein, and brachial plexus are located in this space. Neurovascular compression in this space may occur as a result of a congenital or acquired changes in the clavicle first rib, structural changes in muscles, or changes in shoulder position or trauma.
3. Subcoracoid space beneath the pectoralis muscles, the coracoid process, and ribs posteriorly. The brachial plexus travels through this area and can be affected by hyperabduction of the arm.
 II. Pathophysiology (MacKinnon & Novak, 2002)
II. Pathophysiology (MacKinnon & Novak, 2002)
A. Neurogenic Compression
1. Pathophysiology is complex and may vary depending on the specific predisposing and causative factors. Severity of the condition depends on the duration and magnitude of compressive forces.
2. Mechanical and ischemic factors lead to acute and chronic inflammation
3. Intraneural edema and pressure lead to breakdown of blood–nerve barrier.
4. Pressure cannot escape the peripheral diffusion barrier.
5. Connective tissue thickening occurs.
6. Demyelination of nerve (focal and then more diffuse) occurs.
7. Nerve fibrosis occurs with axonal degeneration, which leads to symptoms and clinical findings.
B. Arterial Compression
1. Secondary to significant and longstanding compression
2. Frequently associated with presence of cervical rib
3. Congenital or acquired abnormalities of first rib, congenital bands, and hypertrophic muscles play a part but are less common than neurogenic factors (Kieffer & Ruotolo, 1995)
4. Arterial wall becomes thick and fibrotic
5. Inflammatory changes fix artery to surrounding structures
6. Poststenotic dilatation and associated chronic compression can progress to aneurysmal changes
7. Localized intimal damage of vessels can lead to thrombosis, subclavian artery occlusion, and ischemia
8. Platelet aggregation can lead to microembolization, distal ischemia, and Raynaud syndrome (Kieffer & Ruotolo, 1995)
C. Venous Compression
1. External pressure on vein results in compression.
2. Thick subclavian muscle, costocoracoid ligament, anterior scalene muscle, and bands create compression.
3. Inflammatory reaction from continuous compression can lead to endothelial injury and venous stasis (MacKinnon & Novak, 2002).
4. Thrombosis of subclavian vein is often referred to as Paget–Schroetter syndrome.
 III. Etiology/Predisposing Factors (Atasoy, 1996; MacKinnon & Novak, 2002; Martinez, 1999; Stoney & Cheng, 1995)
III. Etiology/Predisposing Factors (Atasoy, 1996; MacKinnon & Novak, 2002; Martinez, 1999; Stoney & Cheng, 1995)
A. Mechanical Factors are primary causes of impaired nerve function
1. Postural abnormalities of the shoulder girdle
a. Prolonged positioning leads to chronic nerve irritation
b. Decreased muscle length
1) Pectoralis minor
2) Scalene muscles
3) Sternocleidomastoid
4) Serratus anterior
c. Increased muscle length
1) Middle trapezius
2) Lower trapezius
2. Muscle imbalance/strain
a. Increased pressure of certain compression sites
1) Overuse of muscles
a) Upper trapezius
b) Levator scapulae
2) Underuse of muscles
a) Middle trapezius
b) Lower trapezius
c) Serratus anterior
B. Trauma
1. 60% to 70% of patients have had injury to neck and shoulder girdle area (Atasoy, 1996; Martinez, 1999).
2. Whiplash-type injuries may precipitate compression (Kieffer & Ruotolo, 1995).
C. Occupational Demand
1. Repetitive movements
2. Heavy lifting, particularly if associated with repeated vigorous abduction movement
 IV. Assessment
IV. Assessment
In the absence of a specific gold standard test for TOS, an accurate clinical history and evaluation are paramount in assessing patients.
A. History (Atasoy, 1996; Machleder, 1994; MacKinnon & Novak, 2002)
1. Subjective findings. Symptoms are usually insidious in nature.
a. Neural symptoms
1) In all types the most common symptoms are pain and paresthesia weakness with an easily fatigued arm.
2) Patients reported feelings of clumsiness and dropping things (Urschel & Razzuk, 1998).
3) Symptoms can be aggravated by hyperabduction, elevation of the arm.
4) Pain is usually dull and aching and may progress to such a severity that strong analgesic agents are required for relief.
5) Upper plexus involvement may include pain in side of neck radiating to mandible and face, earache, and occipital headaches. Left upper chest pain can mimic angina pectoris.
6) Dizziness, vertigo, and blurred vision have been reported in some patients with upper plexus compression (woods).
7) Lower plexus symptoms include pain in supraclavicular area, back of neck, and scapular and rhomboid region. Pain can radiate along posterior axilla and inner aspect of arm down to ulnar nerve distribution.
8) Combined, usually is a mixture of symptoms.
9) Neural compression can cause vasomotor changes in the extremity. Changes include coldness and blanching of the hand.
b. Vascular symptoms
1) Arterial
a) Rare but most common manifestation is hand ischemia as a result of microembolization (pain, pallor, coldness, paresthesia)
b) Can be associated with less dramatic symptoms
c) Many times goes unrecognized because it occurs in younger populations without atherosclerotic risk factors
d) Mild symptoms are of exertional arm pain
e) Moderate to severe symptoms of exertional arm pain and even ulceration of the digits
2) Venous symptoms
a) Most common presenting symptom is arm edema
b) Also can have shoulder pain, extremity heaviness and dilated subcutaneous veins in the chest or arm
2. Objective findings
a. Detailed history of trauma
b. Attention to activity or injuries that involve stretching of plexus or hyperabduction, such as typing, painting, lifting, whiplash-type injuries
c. Sleeping postures with arms above the head and elbows flexed may cause complaints of numbness and tingling
d. Pain history, including aggravating activities, alleviating factors
B. Physical Examination
1. Inspection
a. Patient posture
b. Neck and shoulders for bony prominence, apparent muscle spasms
c. Hands for color temperature, muscle strength, and atrophy of small muscles
d. Range of motion of neck and shoulder
2. Palpation
a. Palpate for supraclavicular tenderness elicited by palpating over the anterior scalene muscle, which may reproduce the patient’s pain and numbness.
b. Palpate for a pulsatile mass. It may not indicate an aneurysm, but the artery may be pushed forward by an abnormal bony structure.
c. Palpate peripheral pulses, including brachial and radial. If nonpalpable pulses, obtain Doppler examination for signals.
3. Auscultation
a. Take blood pressure in both arms.
b. Listen for bruits over the supraclavicular fossa.
4. Postural maneuvers/provocative tests (Machleder, 1994; MacKinnon & Novak, 2002; Stoney & Cheng, 1995)
False-positive and false-negative results make monitoring of pulse unreliable in firm diagnosis. Tests that reproduce the patient’s symptoms may provide more accurate information.
a. EAST (elevated arm stress test; Dr. Roos). Arm elevation for 3 minutes with 90-degree shoulder abduction and external rotation and elbow flexed at 90 degrees. Patient opens and closes the hand rapidly. This test has positive results with reproduction of symptoms including pain, paresthesia, and weakness within 60 seconds.
b. Adson test. Patient’s arm is down at the side, head is turned toward the affected side, patient takes deep breath, and radial pulse is monitored. Test is modified with head turned toward unaffected side. Test result is positive if radial pulse is obliterated. This test is considered nonspecific in diagnosis of neurogenic TOS.
c. Roos maneuver. Supraclavicular compression of the brachial plexus at the scalenus anticus level. With compression, symptoms may be reproduced.
d. Halsted test (costoclavicular test). Patient assumes a military pose with shoulder backward and downward to narrow the costoclavicular space. The radial pulse is monitored and test result is positive with obliteration of pulse.
e. Wright test. Hyperabduction external rotation of shoulder to 180 degrees. The radial pulse is monitored and a positive test result is indicated with obliteration of radial pulse.
C. Differential Diagnosis (Stoney & Cheng, 1995)
1. Several disorders can have similar presenting symptoms and must be considered in the differential diagnosis of TOS. This list includes the following:
a. Cervical disc disease
b. Carpal tunnel syndrome
c. Ulnar nerve entrapment
d. Causalgia
e. Paraspinal muscle myofibrositis
f. Soft tissue disorders/tumors
g. Rotator cuff syndrome
h. Angina pectoris
i. Raynaud disease
j. Mitral valve prolapse
 V. Considerations Across the Life Span (Machleder, 1994; Stoney & Cheng, 1995)
V. Considerations Across the Life Span (Machleder, 1994; Stoney & Cheng, 1995)
A. TOS is usually a condition that affects young adults in the third to fifth decade (Stoney & Cheng, 1995).
B. TOS can affect people in their 60s but is usually associated with trauma.
C. Ratio of Female to Male is usually 4:1 (Stoney & Cheng, 1995).
D. Arterial TOS Patients are usually young and report a history of vigorous arm activity.
E. Venous Thrombosis tends to occur more in young men and is associated with strenuous work (MacKinnon & Novak, 2002).
 VI. Pertinent Diagnostic Testing
VI. Pertinent Diagnostic Testing
A. General Testing
1. Plain chest x-rays (posteroanterior and lateral) help determine apical lung pathology.
2. C-spine films provide information related to the presence of cervical ribs, elongated C7 transverse process, clavicular fractures, other bony abnormalities, or signs of degenerative disc disease.
3. Magnetic resonance imaging (MRI) or computed tomography (CT) scan may be indicated in the presence of upper plexus disease to rule out cervical disc compression.
B. Testing for Neurogenic TOS
1. Electromyelogram (EMG)/nerve conduction studies (NCS) determine impairment of nerve conduction function of the brachial nerve at the thoracic levels. It may assist with differential diagnosis of cervical disc disease or carpal tunnel syndrome.
a. Measurement taken when motor conduction velocity is slow across the supraclavicular transaxillary segment of ulnar nerve component of the medial core of the brachial plexus.
b. Normal is considered 60 to 72 m/sec. Less than 60 m/sec is suspicious for TOS (Urschel & Razzuk, 1998).
2. Somatosensory-evoked potential F-wave studies evaluate the brachial plexus.
a. Stimulation of distal part of the upper limb and recordings are in the supraclavicular fossa.
b. Results vary and may produce normal results even in the presence of TOS.
3. These tests have a low level of sensitivity for TOS
C. Testing for Arterial TOS
1. Arterial duplex of the subclavian and axillary arteries demonstrate aneurysmal changes or elevated velocities correlating with a compressive stenosis. TOS maneuvers include the arm at rest and in a horizontal and hyperextended position.
a. May quantify the postural changes in arterial circulation and localize the arterial occlusion
2. Assess collateral circulation. CT with intravenous contrast-enhanced angiography is helpful to obtain the diagnosis and can assist with surgical planning.
a. Can identify the exact point of compression and extent of arterial pathology
b. Has replaced conventional angiography as the main radiographic study in most institutions
3. Arteriogram is performed when patient has evidence of arterial involvement, such as supraclavicular bruit or evidence of microemboli.
a. “Gold standard”
b. Should include from the aortic arch to the digital vessels
c. Can demonstrate distal arterial occlusion and presence of collateral flow
D. Testing for Venous TOS
1. Venous duplex can be used to detect venous thrombosis.
2. Venogram, which is diagnostic for subclavian vein thrombosis. Films should be done in resting and hyperextended arm positions to confirm subclavian axillary vein stenosis or occlusion.
E. Other
1. Electrocardiogram and cardiac echocardiograms, which are conducted to eliminate conditions such as mitral valve prolapse and coronary artery disease
 VII. Medical/Conservative Management
VII. Medical/Conservative Management
A. Neurogenic: Success with conservative treatment of TOS ranges from 50% to 90%. Goal is to decrease compression on the brachial plexus and improve muscle imbalance.
1. Patient education
a. Pathology of nerve compression
b. Impact of activities of daily living on symptoms
c. Aggravating symptoms
d. Relieving strategies individualized to patients
e. Encouragement and support to follow recommended medical regimen and exercise program
2. Activity
a. Activity may need to be modified, especially in highly irritable conditions.
b. Evaluate sleep patterns.
1) Support cervical spine with neck pillows
2) May use neck rolls
c. Encourage patients to maintain work if possible. Occupational modifications, work reassignment, or leave may be needed.
d. Weight reduction, if applicable, may help relieve muscle strain.
3. Physical therapy (MacKinnon & Novak, 2002)
Goal is to restore movement of shoulder girdle and provide more space for neurovascular structures.
a. Posture correction with muscle-specific exercises
1) Neck exercise to increase range of motion
2) Stretching exercises should be low force and longer duration. Target muscles are upper trapezius, levator scapulae, scalene, and sternocleidomastoid
3) Strengthening started after adequate pain-free range of motion is achieved. Target is middle/lower trapezius, serratus anterior, and lower rhomboids
4) Swimming has been found to be a useful modality in some individuals but may aggravate symptoms in others
5) Supervised program is recommended for 2 to 3 weeks to ensure that proper techniques are used
6) Home exercise program may take up to 6 months for impact to be noted
7) Exercises that are too aggressive may lead to noncompliance and be labeled as failure
b. Massage
1) Used to produce muscle relaxation
2) Provides symptom relief and comfort
c. Thermal treatment
1) Moist ice packs in acute case
2) Moist heat in chronic pain
4. Medications
a. Anti-inflammatory agents provide relief from inflammatory reaction/swelling that occurs with nerve compression.
b. Muscle relaxants
1) Affect central nervous system and include carisoprodol (Soma), methocarbamol (Robaxin), and cyclobenzaprine HCl (Flexeril)
2) Affect spinal cord and include baclofen (Lioresal), chlorzoxazone (Parafon), and metaxalone (Skelaxin)
c. Analgesics
1) Pain control can be long term and significant problems occur with patients with chronic nerve entrapment.
2) Over-the-counter medications are recommended (acetaminophen) but may not be helpful after time.
3) Analgesics should be used in combination with other pain relief modalities, such as heat, massage, and diversional interventions.
4) Narcotic medications should be used as last resort and should be monitored carefully to prevent dependence.
5) Medications may need to be alternated to minimize tolerance to one specific agent.
d. Antidepressants may be helpful in select cases, especially with sleep pattern disturbances
5. Other modalities
a. Transcutaneous electrical nerve stimulator (TENS)
b. Braces, which maintain posture in presence of weak muscles, have been used for short-term relief of assistance
c. Nerve blocks, such as brachial plexus and anterior scalene muscle blocks, may grant temporary relief
6. Psychological support
a. Living with chronic pain is stressful to patient and family.
b. Can lead to emotional strain and financial strain if unable to work.
c. Affects body image/role performance in family.
d. Counseling/education should be offered to patient and family members.
e. Specific social services may be needed.
f. Referral to psychologist or psychiatrist may be indicted if patients have severe depression or express suicidal ideation.
7. Rehabilitation
a. Work evaluation may be required for a patient to continue in the same job or determine if work reassignment is required.
b. Evaluation of the activities of the job should include overall ergonomics.
c. Evaluation of need for lifting, working with arms above the head, repetitive motions is noted.
d. Close communication with occupational nurse case managers is necessary.
e. Work reassignment may be required to prevent continued injury.
f. Vocational rehabilitation nurses are a prime resource to assist an individual in continuing to work.
B. Arterial
1. An exercise program is contraindicated in arterial TOS.
2. Overall treatment is surgical intervention.
C. Venous
1. In acute phase, the immediate treatment is that of an acute deep venous thrombosis
a. Anticoagulation with unfractionated heparin followed by conversion to oral warfarin for 2 to 4 months
b. Thrombolysis is frequently used to restore patency.
2. An exercise program is contraindicated.
3. May be followed by surgical decompression
 VIII. Surgical Management
VIII. Surgical Management
Goal is complete decompression of the thoracic outlet with excision of the first rib, cervical bands, and cervical ribs, if present, to relieve constriction on the neurovascular bundle.
A. Indications for Surgery (Martinez, 1999; Urcshel & Razzuk, 1998)
1. Decision for surgery is multifactorial
2. Failure of carefully supervised exercise program
3. Increasing decree of disability
4. Clinical deterioration
5. Evidence of arterial insufficiency or aneurysm
6. Venous thrombosis
B. Surgical Approaches—Various combinations of surgical approaches are available, including first rib resection, scalenectomy
1. Supraclavicular approach: The incision is parallel and 2 cm above the clavicle in the supraclavicular fossa.
a. Advantages
1) Access to interscalene triangle is easier via this approach
2) Exposure to the posterior two thirds of first rib
3) Direct visualization of all four nerve roots
4) Identification of anatomic relationship between bony and fascial structures brachial plexus
5) Removal of cervical rib, if present
b. Disadvantages
1) Access to costoclavicular space and subcoracoid space is poor
2) Incomplete decompression of cervical bands
2. Transaxillary approach is used for rib resection in presence of neurologic symptoms. A transverse incision is made across the axilla to provide safe access to the first rib.
a. Advantages
1) Good access to costoclavicular space
2) Possibility of complete resection of first rib
b. Disadvantages
1) Deep limited exposure. Limitations of exposure can lead to injury of long thoracic nerve and vascular structures
2) Inability to perform cervical rib resection, if needed
c. Endoscopic-assisted transaxillary approach (Martinez, 1999) was developed to address issues of inadequate visualization.
1) Provides direct visualization of structures, including anatomic variations (i.e., cervical bands)
2) Magnifies basic anatomic structures
3) Allows minimally invasive approach
3. Scalenectomy is the division of scalenus anticus and resection of lower portion of muscle at the attachment of the first rib.
a. Advantages
1) Used frequently in arterial TOS and with history of trauma.
2) Complications of this procedure are rare.
3) May be used in combination with first rib resection to provide complete decompression.
b. Disadvantages
1) Phrenic nerve injury possible
2) Procedure alone usually is not sufficient for decompression of thoracic outlet
4. Other approaches, such as the posterior and infraclavicular, have been reported for first rib resections. They are not widely used, and outcome data are not readily available.
5. Arterial reconstruction
a. May be required with arterial TOS.
b. Alternatives may include placement of prosthetic graft, patch, angioplasty, and stent.
c. Postoperative considerations would be same for any patient undergoing arterial reconstruction.
C. Potential Complications of Surgical Intervention (Stoney & Cheng, 1995)
1. Nerve injury
a. Brachial nerve injury is serious. Permanent damage is rare, but arm paralysis has been reported.
b. Long thoracic nerve damage can result in winging of the scapula.
c. Phrenic nerve injury can be identified on chest film with elevation of hemi-diaphragm. Treatment is conservative.
2. Vascular injury
a. Subclavian artery or subclavian vein can be entered inadvertently and repaired intraoperatively.
3. Thoracic duct injury
a. Lymphatics can be damaged during the procedure.
b. When identified, lymphatics are ligated. Small collection may need to be managed in the postoperative period.
4. Pleural complications
a. Most common complication is small tear in the pleura, which can lead to pneumothorax.
b. Small drain can be used or chest tube may be needed for larger injury.
5. Wound infection
a. Uncommon after this type of procedure
b. Treated with local wound care and antibiotic therapy
D. Results—Successful treatment is often reported based on pain relief and return to work/activities. Excellent result is one in which there is complete pain relief and return to work at same job (Urschel & Razzuk, 1997).
1. Mortality is extremely low. No reports of deaths were identified in the literature reviewed.
2. Success outcomes vary. Between 70% and 95% of patients have good or positive outcomes (Machleder, 1993).
3. Approximately 5% of patients have poor results.
4. Symptoms can persist or recur (Mingoli et al., 1995).
a. Scar tissue formation
b. Remnants of first rib
c. Chronic myofibrositis and paraspinal muscle spasms (Martinez, 1999)
 IX. Nursing Diagnosis
IX. Nursing Diagnosis
A. Conservative Care
1. Alteration in comfort related to chronic pain of TOS
a. Expected outcome: appropriate management of pain levels
b. Nursing intervention
1) Assess pain level on specific scale (e.g., scale of 0 to 10).
2) Identify aggravating and alleviating factors.
3) Set pain level target with patient.
4) Avoid blood pressure, IV, venipuncture in affected arm.
5) Discuss effect of chronic pain on ADL and family role.
6) Use nonmedication strategies as appropriate.
a) Modify activity to avoid repetitive motion, heavy lifting
b) Provide alternative measures, including breathing techniques, relaxation, positioning, diversion therapy, heat, and massage
7) Reinforce physical therapy exercise program
8) Administer medication as appropriate, including muscle relaxants and nonsteroidal anti-inflammatory agents
c. Evaluation of nursing care
1) Pain level on scale at or less than identified target
2. Anxiety related to threat of self-image, chronic pain, uncertainness of treatment options
a. Expected outcome: management of anxiety-related physical and behavioral symptoms
b. Nursing interventions
1) Assess anxiety level and causative factors
2) Identify manifestations of anxiety
3) Educate on identified knowledge deficit that may aggravate anxiety
4) Reinforce effective coping strategies
5) Assist in setting realistic goals for symptom relief
c. Evaluation of nursing care
1) Recognize anxiety and coping patterns
2) Identify potential anxiety relief techniques
3. Potential alteration in family processes related to illness of patient and potential change in roles
a. Expected outcome: support in management of family environment
b. Nursing interventions
1) Encourage participation by family members/significant others in process
2) Assess current family dynamics
3) Identify potential needed resources
4) Educate to alleviate knowledge deficit
5) Refer to appropriate social service agencies as appropriate
6) Encourage and support questions and open dialogue of family members
c. Evaluation of nursing care
1) Verbalize potential coping strategies to relieve situational stressors
2) Refer to appropriate agencies, if needed
4. Potential sleep pattern disturbance
a. Expected outcome, experience an optimal balance of rest and activity
b. Nursing intervention
1) Provide measures to induce sleep, such as soft music, back rub, warm showers
2) Use support mechanism such as neck rolls, pillows for proper positioning at night
3) Limit number of daytime naps
4) Reduce or eliminate environmental distractions
c. Evaluation of nursing care
1) Verbalize effective measures for personal environment
2) Verbalize improvement in night-time sleep pattern
5. Knowledge deficit related to disease processes, treatment options, and pain control
a. Expected outcome
1) Express understanding of causes of TOS, aggravating factors, and alleviating factors
2) Describe needed alterations in lifestyle
3) Discuss medications, including dose indications and potential adverse reactions
b. Nursing intervention
1) Assess current knowledge level.
2) Assess readiness to learn, including learning barriers, cultural influences, current pain level, and anxiety.
3) Review anatomy, probable etiology.
4) Discuss management of aggravating activities.
5) Identify with patient mechanism to alleviate pain.
6) Review and reinforce information about medications.
c. Evaluation of nursing care
1) Verbalize understanding of TOS.
2) Identify strategies to minimize symptoms.
3) Take medication as ordered and report any adverse events.
B. Postoperative Care
1. Alteration in comfort related to postoperative pain from surgical incision
a. Expected outcome: adequate control of acute postoperative pain
b. Nursing intervention
1) Assess pain level on specific scale (e.g., 0 to 10 scale); reassess after implementation of pain management techniques.
2) Identify aggravating and alleviating factors.
3) Set pain level target with patient.
4) Use nonmedication strategies as appropriate, including breathing techniques, relaxation, positioning, and diversion therapy.
5) Administer medication as appropriate.
c. Evaluation of nursing care
1) Pain level on scale of 10 is 4 or less or at identified target
2. Ineffective airway clearance related to pain and potential ineffective cough
a. Expected outcome: exhibits adequate respiratory function
b. Nursing intervention
1) Assess lung sounds and respiratory rate, temperature at regular intervals (potential for atelectasis and pneumonia)
2) Encourage lung expansion
a) Cough and deep breathing frequently
b) Use incentive spirometer, if indicated.
c) Ambulate at regular intervals.
3) Maintain adequate hydration
4) Review postoperative chest film and report abnormal findings to physician
c. Evaluation of nursing care
1) Demonstrate effective coughing and deep breathing.
2) Maintain patent airway and clear lung sounds.
3. Potential neurodeficit related to neurocompromise
a. Expected outcome: absence of neurocompromise
b. Nursing interventions
1) Monitor ulnar, radial, and palmar arch pulses.
2) Assess color warmth and movement of fingers/hand.
3) Assess sensory motor function of affected arm.
4) Elevate arm on pillow in presence of edema.
c. Evaluation
1) Motor sensory function intact
4. Potential alteration in peripheral tissue perfusion
a. Expected outcome: maintenance of adequate circulation and perfusion to affected extremity
b. Nursing intervention
1) Assess arterial and venous circulation.
a) Monitor radial pulse, color, warmth, movement, numbness, and tingling.
b) Examine for edema, venous distention.
2) Position for comfort in neutral position, may elevate on pillow
c. Evaluation of nursing care
1) Circulation intact
5. Potential for infection
a. Expected outcome: free from infection
b. Nursing intervention
1) Monitor vital signs at regular intervals
2) Monitor laboratory work, especially WBC as indicated
3) Maintain aseptic technique in dressing changes and management of drains
4) Assess IV sites and drain sites
c. Evaluation of nursing care
1) Temperature within normal limits
2) Wound healing without evidence of infection
 X. Patient Teaching
X. Patient Teaching
A. Conservative Management
1. Encourage participation by family/significant others.
2. Define TOS.
3. Discuss effect of chronic pain on ADL and family role.
4. Discuss alterations and methods to adjust lifestyle; identify strategies to deal with symptom management.
5. Reinforce and encourage physical therapy exercises to be continued at home after initial instruction in physical therapy department.
6. Discuss diet: high protein, low animal fat.
7. Discuss activity, balance of activity, and rest.
8. Discuss medication, including pain cycle use, dose, and adverse effects.
B. Preoperative
1. Complete required preoperative testing (laboratory work, ECG, and others as indicated)
2. Discuss hospital admission process (registration, surgery, postoperative unit)
3. Anticipate postoperative course, including nursing assessments, medication administration, and length of stay
4. Encourage questions for clarification and understanding
5. Provide support to patient and family/significant others
C. Postoperative
1. Wound care
a. Observe for changes and note swelling, redness, drainage, or bleeding
b. May shower, wash with soap and water, pat dry
c. Wear deodorant only above incision line until wound healed
2. Medications, including pain cycle use, dose, adverse effects
3. Activity
a. Activity as tolerated
b. No driving until first postoperative visit
c. May use arm for simple activities (e.g., brushing teeth, eating), but maintain below shoulder level until given instructions on postoperative exercise
d. Do not carry purse or backpack with affected arm until postoperative visit.
4. Diet
a. High-protein diet is needed for wound healing
b. Low animal fat
5. Signs and symptoms of infection
a. Observe for signs of redness or drainage from surgical incision
b. Report elevated temperature
c. Maintain good handwashing
d. Take acetaminophen or ibuprofen for fever, unless specifically contraindicated. Discuss with physician or nurse
6. Follow-up appointments
a. Usually 1 to 2 weeks after discharge
b. Notify sooner for any questions or unusual findings
c. Postoperative exercise instructions usually given at first postoperative visit
CASE STUDY
EJ is a 29-year-old woman who was referred to the vascular surgeon for evaluation of possible TOS. With the exceptions of her current problems, her past medical history is negative. Current medications include birth control pills and over-the-counter treatment for arm pain and headaches. She states that the acetaminophen is no longer effective.
She started teaching 6 months previously, which required increased computer work and arm elevation to write on the board. She is a harp player and plays or practices five nights a week for minimum of 1 hour duration.
Current symptoms include pain in the upper right arm for 2 years, but the pain has worsened since starting teaching. She has paresthesia when playing harp. She also states that she is having increasing numbers of headaches and neck pain.
Objective evaluation exhibited the following findings: A young female, 5’7’’ tall and 127 lbs, with a slight frame. She is right handed. Blood pressures are equal bilaterally. There is no bruit noted over the supraclavicular fossa. Brachial, radial, and ulnar pulses are 2+ at rest and elevation. Hands are pink and warm and have strong hand grasp. No evidence of micro-embolization or venous distention. There is tenderness over the supraclavicular area, and her symptoms are reproducible with pressure.
Review Questions
1. What provocative maneuvers during physical examination can assist in the diagnosis of TOS?
2. List three disorders that must be considered in the differential diagnosis of TOS.
3. Diagnostic testing, including chest x-ray, C-spine films, EMG/NCV, and MRI were completed, and the diagnosis of neurogenic TOS on the right side was made. At this time, patient had not exhausted medical treatment.
Patient education should include what conservative measures to improve symptoms and control pain?
4. Patient did well with exercise for 2 years. Now returns with complaint of increased pain in lower arm, numbness in the fourth and fifth digits of right hand. She states that she has clumsiness and seems to have difficulty with fine motor movement necessary to play the harp.
On physical examination, her right hand is cool at rest and pale when elevated. Pulses are 1+ at rest and absent with elevation. Medications now include Tylenol #3, which she states she is taking at night to help her sleep and once or twice a day as needed. An arterial duplex scan is positive for diminished flow during TOS maneuvers.
What were the indications for surgery?
5. Patient underwent a right transaxillary rib resection and was discharged on the second postoperative day. What should her discharge teaching include?
Answers/Rationales
1. (a) EAST (elevated arm stress test; Dr. Roos). Arm elevation for 3 minutes with 90-degree shoulder abduction and external rotation and elbow flexed at 90 degrees. Patient opens and closes the hand rapidly. The test result is positive with reproduction of symptoms; (b) Adson test. With the patient’s arm at the side and his or her head turned toward the affected side, the patient takes a deep breath and the radial pulse is monitored. Test is modified with head turned toward unaffected side. Test result is positive if radial pulse is obliterated. This test is considered nonspecific in diagnosis of neurogenic TOS; (c) Roos maneuver. Supraclavicular compression of the brachial plexus at the scalenus anticus level. With compression, symptoms may be reproduced; (d) Halsted test (costoclavicular test). Patient assumes a military pose with shoulder backward and downward to narrow the costoclavicular space. The radial pulse is monitored and test result is positive with obliteration of pulse; (e) Wright test. Hyperabduction external rotation of shoulder to 180 degrees. The radial pulse is monitored and a positive test result is indicated with obliteration of radial pulse.
2. Any of the following:
| Cervical disc disease | Carpal tunnel syndrome |
| Ulnar nerve entrapment | Causalgia |
| Rotator cuff syndrome | Paraspinal muscle myofibrositis |
| Mitral valve prolapse | Angina pectoris |
| Raynaud disease | Soft tissue disorders/tumors |
3. (a) Physical therapy to restore movement of shoulder girdle and provide more space for neurovascular structures. Should include postural correction and strengthening exercises. This starts with a supervised program and continues in a home exercise program; (b) Massage to produce muscle relaxation and comfort; (c) Heat in chronic TOS is recommended as pain relief and to help reduce spasms; (d) Medications, which may include anti-inflammatory agents, muscle relaxants, and analgesics. Antidepressant drugs may be helpful in some patients; (e) Analgesics, if necessary, should start with over-the-counter medication before narcotics are initiated. They should be used in combination with other pain control modalities; (f) Pain control measures should include alternatives to medications, such as biofeedback, diversion, and relaxation therapy; (g) Psychological support should be offered to patient and family because TOS can affect body image, role in family, and financial and social status of the entire family.
4. (a) Increase in neurogenic symptoms: pain in lower arm extending down to digits, ‘‘clumsiness,’’ and decreased fine motor movement of fingers; (b) Evidence of an arterial component: cool hand, pale on elevation, diminished pulses at rest and absent with elevation; (c) Increasing requirements for medication for pain control. Decreasing quality of life.
5. (a) Wound care: Observe for changes and note swelling, redness, drainage, or bleeding. May shower, wash with soap and water, and pat dry. Wear deodorant only above incision line until wound healed; (b) Activity: Activity as tolerated; no driving until first postoperative visit. May use arm for simple activities (i.e., brush teeth, eat, but maintain arm below shoulder level until given instructions on postoperative exercise). Do not carry purse or backpack with affected arm until postoperative visit; (c) Diet: Low animal fat, high-protein diet is needed for wound healing; (d) Signs and symptoms of infection: Observe for signs of redness or drainage from surgical incision. Report elevated temperature. Maintain good handwashing. May take acetaminophen or ibuprofen for fever, unless specific contraindications. Discuss with physician or nurse; (e) Rehabilitation: May be slow and should not be rushed. Work evaluation may be required for patient to continue in the same job or determine if work reassignment is required.
REFERENCES
Atasoy, E. (1996). Thoracic outlet compression syndrome. Orthopedic Clinics of North America, 27(2), 265–303.
Kieffer, E., & Ruotolo, C. (1995). Arterial complications of thoracic outlet syndrome. In R. Rutherford (Ed.), Vascular surgery (4th ed., pp. 992–999). Philadelphia, PA: W.B. Saunders.
Machleder, H. (1993). Vascular disease of the upper extremity and the thoracic outlet syndromes. In W. Moore (Ed.), Vascular surgery: A comprehensive review (pp. 597–605). Philadelphia, PA: W.B. Saunders.
Machleder, H. (1994). Thoracic outlet disorders: Thoracic outlet compression syndrome and axillary vein thrombosis. In F. Veith, R. Hobson, R. Williams, & S. Wilson (Eds.), Vascular surgery principles and practice (2nd ed.). New York, NY: McGraw Hill.
MacKinnon, S., & Novak, C. (2002). Thoracic outlet syndrome. Current Problems in Surgery, 39, 1070–1145.
Martinez, B. (1999). Thoracic outlet syndrome: Endoscopic transaxillary first rib resection and thoracodorsal sympathectomy for causalgia. In R. White & T. Fogarty (Eds.), Peripheral endovascular interventions (2nd ed., pp. 531–538). New York, NY: Springer.
Mingoli, A., Feldhaus, R. J., Farina, C., Cavallari, N., Sapienza, P., di Marzo, L., & Cavallaro, A. (1995). Long-term outcome after transaxillary approach for thoracic outlet syndrome. Surgery, 118(5), 840–844.
Sanders, R. J. (2010). Thoracic outlet syndrome, general considerations. In J. L. Cronenwett & K. W. Johnston (Eds.), Rutherford’s vascular surgery (7th ed., pp. 1865–1877). Philadelphia, PA: Saunders.
Stoney, R., & Cheng, S. (1995). Neurogenic thoracic outlet syndrome. In R. Rutherford (Ed.), Vascular surgery (4th ed., pp. 976–992). Philadelphia, PA: W.B. Saunders.
Urschel, H., & Razzuk, M. (1997). Upper plexus thoracic outlet syndrome: Optimal therapy. Annals of Thoracic Surgery, 63, 935–939.
Urschel, H., & Razzuk, M. (1998). Neurovascular compression in thoracic outlet: Changing management over 50 years. Annals of Surgery, 228(4), 609–617.
< div class='tao-gold-member'>



