CHAPTER 22
Diabetic Foot Management
Robyn Strauss
Cynthia Christensen
OBJECTIVES
1. Describe the pathophysiology of diabetes mellitus that leads to the formation of foot problems in this patient population.
2. Identify the essential elements of a complete assessment of the diabetic foot, with and without ulceration.
3. List appropriate nursing recommendations for primary and secondary prevention of diabetic foot ulcerations.
Introduction/Overview
Diabetes mellitus is a genetic disorder of carbohydrate metabolism characterized by hyperglycemia and glucose intolerance, resulting from defects in insulin production, insulin action at the tissue level, or both. This disease, which affects both the microvascular and macrovascular circulation, is common in the United States. Diabetes affects 25.8 million people (8.3% of the US population) (Centers for Disease Control and Prevention (CDC), 2011). The incidence of new cases for people over age 20 is 1.9 million per year, with the greatest increase in prevalence expected in the elderly (252% for women; 537% for men) over the next five decades.
• In contrast to the 2007 National Diabetes Fact Sheet, which used fasting glucose data to estimate undiagnosed diabetes and prediabetes, the 2011 National Diabetes Fact Sheet uses both fasting glucose and A1C levels to derive estimates for undiagnosed diabetes and prediabetes. These tests were chosen because they are most frequently used in clinical practice.
• Minority groups are more likely to have diabetes than Caucasians. After adjusting for population age differences, 2007 to 2009 national survey data for people aged 20 years or older indicate that 7.1% of non-Hispanic Whites, 8.4% of Asian Americans, 11.8% of Hispanics, and 12.6% of non-Hispanic Blacks had diagnosed diabetes. Among Hispanics, rates were 7.6% for both Cubans and for Central and South Americans, 13.3% for Mexican Americans, and 13.8% for Puerto Ricans.
• Compared to non-Hispanic White adults, the risk of diagnosed diabetes was 18% higher among Asian Americans, 66% higher among Hispanics, and 77% higher among non-Hispanic Blacks. Among Hispanics compared to non-Hispanic White adults, the risk of diagnosed diabetes was about the same for Cubans and for Central and South Americans, 87% higher for Mexican Americans, and 94% higher for Puerto Ricans. Native Americans, including Alaskan Natives, are also 2.2 times more likely to have diabetes than non-Hispanic Whites of similar age (CDC, 2011).
• Many people with diabetes will develop foot problems related to their disease. A foot problem is the most common reason that diabetic patients require admission to the hospital and is the number one cause of lower leg amputations in the United States (Frykberg, 2005). The annual incidence of lower extremity leg and foot ulcers is 200,000. There are approximately 65,000 lower extremity amputations in diabetic patients annually and in 2006, more than 60% of nontraumatic lower-limb amputations occurred in people with diabetes (CDC, 2011).
• 50% to 70% of all nontraumatic lower leg amputations occur in diabetic. Of these amputations, 85% are performed for complications of foot ulcers, 5% to 15% of all people with diabetes will require an amputation at some time in their lives. Fifty percent of diabetics who undergo amputation of one leg will go on to loose the other leg within 5 years (Yao & Pierce, 2001).
Patient education and proper foot care can reduce the amputation rate by 80% and hospitalizations by 65%. The three leading components that define the pathophysiologic triad of diabetic foot ulcers are ischemia, neuropathy, and altered response to infection (Frykberg, 2003).
 I. Anatomy/Pathology
I. Anatomy/Pathology
A. Predisposition to the Development of Foot Disorders Due to Vascular and Neuropathic Complications Common to the Disease
1. Enhanced vulnerability of the foot to damage by environmental trauma.
2. Arterial insufficiency resulting in ischemia may produce pathology in the lower extremity by tissue necrosis, or may adversely affect the ability to heal or fight infection.
3. Loss of pain and temperature sensation.
4. Decreased resistance to infection.
B. Anatomic Change in Shape of Foot: Charcot foot.
1. Two theories explain change in structure (Sommer & Lee, 2001)
a. Neurotraumatic theory: bony destruction due to loss of pain sensation and proprioception combined with repetitive and mechanical trauma to foot.
b. Neurovascular theory: joint destruction due to autonomically stimulated vascular reflex that leads to hyperemia (arteriolar–venular shunting) and periarticular calcium loss (osteopenia); trauma also contributes to change.
2. Muscle imbalance leads to increased pressure on heel and plantar surfaces.
3. Microfractures and ligament laxity result, causing progressive bony destruction.
4. Tarsometatarsal (Lisfranc) joint most common site for arthropathy (Sommer & Lee, 2001).
a. 70% midfoot
b. 15% forefoot or rearfoot.
5. 50% of patients can recall a precipitating trauma, for example, ankle sprain.
 II. Pathophysiology
II. Pathophysiology
A. Hyperglycemia
1. Chronic hyperglycemia and insulin resistance in insulin-sensitive target tissues causes major complications related to cardiovascular, peripheral vascular, retinal or renal comorbid conditions.
2. Diabetes accelerates development of all atherosclerotic complications causing vascular complications in microvessels (eye, kidney, and nervous system) and macrovessels (heart and peripheral circulation).
3. Changes in myo-inositol, polyol pathway, (producing excess sorbitol) NA/K/ATPase and phosphoinositol metabolism leads to accumulation of products toxic to nerve tissue. Water accompanies the sorbitol into these tissues, causing the nerve cell to expand. The result is decreased nerve conduction speed and eventual irreversible nerve damage. Decreased myo-inositol alters myelin synthesis, also decreasing NA/K/ATPase activity.
4. When blood glucose levels are elevated, a glucose molecule attaches itself to hemoglobin in a red blood cell. The longer the glucose remains above normal, the more glycosylated hemoglobins form. Raised levels of glycosylated hemoglobin, which binds oxygen to itself causes tissue hypoxia. Protein glycosylation results in decreased joint mobility, leading to high foot pressures (Frykberg, 2005).
5. Impedes outflow of leukocytes thus lowering resistance to infection and probably impairs host defense against infection. Functional abnormalities of neutrophils occur.
B. Neuropathy: 60% of patients with diabetes present for longer than 5 to 10 years have neuropathy (Frykberg, 2005).
1. Peripheral neuropathy
a. Distal symmetrical polyneuropathy most common form involving sensory, motor, and autonomic nerve fibers
1) Paresthesia: symptoms of tingling or buzzing
2) Dysesthesia: more severe manifestation of sensory nerve fiber destruction, causing sensations ranging from mildly painful “pins and needles” to intense burning pain like “hot poker”
3) Hyperesthesia: an exaggerated sensitivity in the skin
b. Changes in nerve cell axon causes a “dying back” of the nerve with distal neurons being affected producing a “stocking-glove” distribution. Loss of myelinated and unmyelinated nerve fibers.
c. Involvement of large sensory and motor fibers diminishes light touch and proprioception, the latter resulting in ataxic gait and unsteadiness, weakness of intrinsic muscles of hand and feet.
d. Involvement of small fibers diminishes pain and temperature perception.
e. Motor nerve impairment may cause muscle atrophy leading to foot deformation and maldistribution of pressure over surface of foot.
2. Autonomic neuropathy
a. Pseudomotor neuropathy: produces asymptomatic anhydrosis in “stocking glove” distribution causing absence of sweating leading to dry, cracked, fissured skin.
b. Vasomotor instability may produce arteriovenous shunt in foot possibly due to abnormal sympathetic innervation resulting in lower tissue oxygen tension.
C. Peripheral Vascular Disease
1. Changes in vessel walls, both in media and intima consist of deposits of platelets, smooth muscle cells, lipids, cholesterol, and calcium.
2. Small vessel or microangiopathy with involvement of the tibial and peroneal arteries and their smaller branches below the knee (infrageniculate) most common. However, the dorsalis pedis has been found to be spared, rendering revascularization to the foot a most viable option for this population.
a. Thickening of capillary basement membrane makes it highly permeable to fluid and protein.
b. Plasma becomes more viscous, erythrocyte and platelet aggregation increase, and fibrinogen levels rise while fibrinolytic activity fall causing formation of microthrombi and/or total occlusion of the capillary.
3. Large vessel or macroangiopathy: Thrombus formation and occlusions can cause gangrene in large segment of lower extremity depending on level and degree of vascular occlusion.
4. Hypoxia resulting from macrovascular and microvascular disease causes
a. Increased flow
b. Peripheral edema
c. Neuropathic edema
d. Endothelial dysfunction
e. Impaired nitric oxide production (Frykberg, 2005)
D. Diabetic Foot Ulcers
1. Progressive loss of peripheral nerve function leading to loss of protective sensation
2. Progressive loss of blood supply
3. Infection
a. Mild infection: monomicrobial organism; usually gram-positive cocci (Staphylococcus aureus and Group B beta hemolytic streptococci) found most frequently
b. Severe infection: polymicrobial; gram-negative rods and anaerobes from deeper wounds
c. Anaerobes frequent due to anoxia in poorly vascularized tissues
d. Up to 30% incidence of methicillin-resistant S. aureus (MRSA) (Frykberg, 2003)
e. Destroys tissue and leads to microthrombi resulting in gangrene and amputation
f. Ulceration is rarely caused by infection, but open ulcers serve as a portal of entry for pathogenic bacteria
g. Culturing wounds that are not clinically infected not recommended; cultures of deep or limb-threatening infections is reliable for isolation of causative organism (Frykberg, 2003)
 III. Etiology or Precipitating Factors
III. Etiology or Precipitating Factors
A. Chronic Hyperglycemia
1. Tight control of diabetes reduces risks for development of foot ulcers, infection, and hospitalization of foot problems. The DCCT and EDIC Diabetes Control and Complications Trial (NIH Publication No. 08-3874, 2008) landmark 9-year multicenter randomized clinical trial was designed to compare intensive with conventional diabetes therapy with regard to their effects on the development and progression of early vascular and neurologic complications of IDDM. The results show that tight control could reduce retinopathy by 70%, peripheral neuropathy by up to 60%, and nephropathy by up to 50% in patients with Type I diabetes. This was achieved by maintaining HgbA1C at or below 7.2% (NIH Publication No. 08-3874, 2008).
2. In March 2009, the long awaited results of the Normoglycemia in Intensive Care Evaluation–Survival Using Glucose Algorithm Regulation (NICE–SUGAR) were released. This created intense controversy in the area of glycemic control in the critically ill. NICE–SUGAR was powered to finally address the question of “does tight glycemic control in the intensive care unit (ICU) decrease mortality?”
3. NICE–SUGAR was a much larger study conducted in multiple countries at 41 different centers and was specifically powered to detect an absolute risk reduction similar to that of the original Leuven study. It included a heterogeneous population of medical and surgical patients, treating physicians, nurses, and other caregivers. It is unlikely that an intuitive culture for intensive insulin target (IIT) and nutrition was nurtured in this setting. In addition, insulin infusions were started through central lines and other venous access types as well. Furthermore, a variety of glucose determination methods were used to target glycemic control. Patients in this study were not started on a dextrose infusion on day 1, nor were they placed on combined enteral and parenteral nutrition to achieve a caloric goal. This study reported a significant 3% increase in mortality in the IIT group. Even though there was no increased morbidity with tighter glycemic ranges, there was no protective effect, which the original Leuven study had initially found (Scurlock, Raikhelkar, & Mechanick, 2010).
4. Multiple variables were not reproduced in the study aims of the NICE–SUGAR trial and several factors were not able to be controlled for. The various instruments to measure serum blood glucose, variation of control targets, serum blood glucose measurement access (arterial or venous line), variation of caregiver knowledge related to treatment algorithm, all lead to varied results in the ICU-managed diabetic patient (Scurlock et al., 2010).
5. However, tight glycemic control was associated with a lower rate of septicemia and significantly increased risk of hypoglycemia (Scurlock et al., 2010).
6. Obesity was linked to poor control of diabetes and risk factor for heel problems and Charcot joint.
B. Neuropathy (see Fig. 22-1)
1. Sensory: loss of sensation in feet primarily responsible for initial foot wound and failure to heal.
a. Painless trauma
1) Mechanical
a) Blisters and calluses from ill-fitting shoes
b) Home surgery on corns and calluses or cutting toenails too close
2) Chemical
a) Use of irritating topical and keratolytic agents
b) Corrosive chemicals

FIGURE 22.1 Neuropathic foot medial callus.
3) Thermal
a) Bathing in hot water
b) Use of heating pads, hot water bottles, heaters, and so forth.
c) Frostbite
2. Motor: foot deformities from motor fiber destruction
a. Muscle atrophy secondary to motor nerve impairment causes change in configuration of foot and leads to new pressure points.
1) Depression of metatarsal heads that shift plantar fat pad
2) Hammer toes: buckling of toe into swan neck deformity caused by weakness of small muscles of foot; toes no longer stabilized on ground; leads to increased pressure over metatarsal head, elevated interphalangeal joint (middle knuckle) and tips of toes
3) Claw toes: more buckling and greater deformity than hammer toes; fixed flexion of interphalangeal joint with callus or ulcers on toe tips and dorsum of interphalangeal joints
4) Pes cavus: abnormally high arch or dome that extends between first metatarsal head and calcaneus; leads to decreased area of contact of forefoot with ground while walking and results in abnormal increased pressure with callus formation under metatarsal heads
5) Fibrofatty padding depletion: reduction of thickness of fat pad over metatarsal heads; cushion no longer able to pad normal walking pressures
6) Hallux valgus: deformity of first metatarsophalangeal joint with lateral deviation of hallux; medial aspect of foot more prominent and prone to ulcerate from tight shoes
b. Charcot foot
1) Bone and joint damage to midfoot leads to collapse
2) Rocker-bottom deformity: displacement of tarsus downward
3) Convexity of medial midfoot: talonavicular joint displaced
4) Bony prominence leads to difficult-to-heal ulceration on plantar foot
5) If the ankle is involved, the hindfoot becomes unstable
6) If the collapse is acute with marked swelling, erythema, and pain, it is difficult to distinguish from osteomyelitis or cellulitis
c. Foot drop/peroneal paralysis: lesion in lateral peroneal nerves
3. Autonomic
a. Denervation of sweat glands leads to cracking of dry skin and serves as portal for bacterial invasion, especially if hygiene poor
b. Fissures are common on heels or in calloused skin
c. Loss of sympathetic tone results in arteriovenous shunting and insufficient nutrient flow
C. Skin and Nail Problems
1. Skin
a. Dry, cracked
b. Stasis dermatitis: pruritus leads to self-inflicted wounds from scratching
c. Dependent edema: multiple etiologies; leads to blisters from tight shoes
d. Tinea pedis: chronic skin breakdown and source of infection; often interdigital
2. Nails
a. Onychomycosis: chronic fungal nail; may lead to complete destruction with detachment, odor, and purulent drainage
b. Neglected nail care: promotes fungal changes and ulceration of surrounding soft tissue
c. Improper nail trimming: cutting skin, creation of residual spikes, or attempting to trim nails on insensate foot may lead to infection
d. Involved nail: exaggerated C-shape with curvature of lateral edges into skin may require permanent removal to prevent recurrent infection or pain
D. Peripheral Vascular Disease: inadequate blood flow to meet demands of infection/wound healing
 IV. Assessment
IV. Assessment
A. Risk Factors/Primary Prevention
1. Smoking
2. Hyperglycemia
3. Hyperlipidemia
4. Age
5. Duration of diabetes
6. Hyperinsulinemia (insulin acts as a growth hormone-like substance and high insulin levels may stimulate growth of smooth muscle cells on these plaques)
7. Medications
a. Vasopressors, for example, dopamine: vasoconstriction effects
b. Inotropic drugs
c. Beta blockers: can impair peripheral circulation from unopposed alpha; vasoconstriction effects.
B. Ulcer History/Foot Injuries
1. Direct mechanical injury: skin is broken or penetrated
2. Ischemia injury: can result from very low pressures over 1 to 12 hours. Usually occurs over side of foot and is the result of shoes that are too tight
3. Repetitive stress
a. Most frequent cause of injury to insensitive foot due to constant, repeated, moderate repetitive pressure to plantar surface while walking long distances
b. High pressure point area will become blister and eventually forms ulcer
C. Spreading Infection
1. Infection is present in majority of foot ulcers and is a frequent precursor to amputation (Frykberg, 2003)
2. The patient does not change gait in the early stages of trauma as it is not perceived as painful and continues to walk on foot, thus spreading infection throughout the soft tissues
a. Chronic osteomyelitis
b. Necrotizing fasciitis
c. Gangrene
d. Synergistic necrotizing cellulitis
D. Patient History
1. Subjective findings
a. Patient’s chief complaint
1) Main reason for hospitalization is infection and impending loss of limb
2) Outpatient treatment/management possibly consists of debridement, wound care, antibiotics, and close follow up
3) History of events causing wound and development of ulcer
4) Painful or nonpainful wound
5) Previous treatment or therapy for problem; antibiotics
6) History of vascular disease
a) Intermittent claudication: walk for several minutes, legs cramp, need to stop until the discomfort stops, then walk again for several more minutes and pain comes back causing individual to stop again.
b) Rest pain: persistent pain caused by nerve and vessel ischemia; decreases with dependency of lower extremities; aggravated by heat, elevation, and exercise. Patients get relief by sitting up and dangling legs.
c) Nocturnal ischemic pain: form of ischemic neuritis usually precedes rest pain. Occurs at night during sleep with little perfusion of lower extremities; relieved by standing up or dangling feet over edge of bed or taking a few steps.
7) History of neuropathy
a) Signs and symptoms of numbness, pain, or tingling in legs and feet.
b) Walking tends to relieve neuropathic pain.
8) History of diabetes duration and control: method of self-monitoring at home, frequency of diabetic complications (DKA and hypoglycemia), current treatment of diabetes including medications, meal plan, and diabetes self-management training.
b. Foot care behaviors at home
c. Previous ulcer: 70% risk of new ulcer if previous ulcer within past 5 years (Frykberg, 2005)
d. Other: history of other diabetic complications (e.g., retinopathy, nephropathy, heart disease)
2. Objective findings
a. Types of injury
1) Direct mechanical injury
2) Ischemic injury
3) Repetitive stress
4) High pressure point area will become blister and eventually form an ulcer
b. Metabolic control: HgbA1c
c. Metabolic disorders/autoimmune disorders
d. Medications which impede wound healing
1) Steroids
2) Nonsteroidal anti-inflammatory drugs
3) Antineoplastics
e. Vital signs and laboratory values indicating hypertension or infection (delineation of wet or dry gangrene): elevated blood sugars, white blood cell count, and presence of fever or chills
f. Nutritional assessment: vitamin/mineral deficiencies
g. Tumors
h. Family history
1) Hypertension
2) Hyperlipidemia
3) Noninsulin-dependent diabetes mellitus
4) Insulin-dependent diabetes mellitus
5) Atherosclerotic cardiovascular disease and age of onset
i. Social history
1) Occupation if working
2) Tobacco use in any form
3) Alcohol use or abuse
4) Compliance-related issues/barriers to care: family support, money to buy food, blood sugar testing supplies, or appropriate shoes
5) Medication history
6) Length of time on oral hypoglycemics
7) Length of time on insulin
8) Antibiotics for current problem
a) All current drugs including OTC and herbal supplements, past use of beta-blockers or vasopressors
E. Physical Examination
1. Inspection
a. Presence of wound or ulcer (neuropathic diabetic ulcers are usually found on the plantar surface of the foot, punched out margins with hyperkeratotic rim, round dry lesions, may be covered with green–brown eschar. Ischemic ulcers result usually from trauma to the foot, wound appearance is usually smooth with punched out margin, and pale and unhealthy granulation tissue)
1) Size and depth of ulcer, staging of ulcer if applicable (Stages 1 to 4)
2) Diameter
3) Drainage
4) Color of drainage
5) Gas bubbles present
6) Edema of surrounding tissues
7) Cellulitis
8) Abscess
9) Fluctuation
10) Inspect between toes
b. Color
1) Pale, bluish, mottled, or dusky tone of feet indicate poor circulation
a) Note color changes of extremity in relation to position change
b) Pallor on elevation, prolonged filling time, and dependent rubor are hallmarks of significant lower extremity vascular insufficiency. Feet will pale on elevation after 30 seconds especially in soles, heel, and toes. Then dangle legs; normally color will return to toes in 10 seconds
c) Dependent rubor after 2 minutes indicates severe ischemia
2) Redness or early inflammation or irritation. the normal responses to infection, vessel dilation, heat, and redness are not always seen in the diabetic patient
3) Dark brown patches may be vascular abnormalities
4) Dark brown scars, indicate past lesions
c. Hair loss on lower extremities
d. Shape of foot or change in shape—foot drop or abnormal gait.
e. Hygiene
1) Cleanliness
2) Condition of stockings and shoes. Look at signs of wear inside the shoe
f. Condition of toenails and presence of fungal infections
2. Palpation
a. Pulses bilaterally, amplitude as well as deficits
1) Popliteal, posterior tibial, dorsalis pedis
2) Noncompressible arteries are common in diabetes due to arterial calcification
b. Skin temperature: compare one side to the other; note any line of coolness. “Hot spots” are among first signs of inflammation but may not always be present
c. Assess for pedal edema or edema of surrounding area of ulcer
d. Note any crepitus indicating gas gangrene and nonclostridial gangrene
3. Percussion
a. Decreased vibratory sensation indicate peripheral neuropathy; normally perceived for 20 to 25 seconds
b. Achilles deep tendon reflex: decreased or absent in presence of peripheral neuropathy
4. Auscultation: may have fixed tachycardia or orthostatic hypotension with autonomic neuropathy
F. Wound Classification
1. Even though several scales are currently utilized, American Diabetes Association (ADA) does not recommend a specific classification scheme (Frykberg, 2005)
2. Meggitt–Wagner: most commonly used scale worldwide (Frykberg, 2005)
a. Grade 0: preulcer lesions, healed ulcers, presence of bony deformities
b. Progresses to grade 5: gangrene of entire foot
c. Does not address ischemia or infection
3. University of Texas classification system
a. Used to document depth, presence of infection, and vascular impairment
b. Validated to predict amputation as depth of wound progresses from grade 0 to 3 and through four stages
1) Stage A: no infection
2) Stage B: infection
3) Stage C: peripheral vascular disease
4) Stage D: infection plus peripheral vascular disease
4. ADA consensus recommendations for diabetic wound evaluation (Frykberg, 2005)
a. History of trauma: penetrating, blunt, or burn
b. Duration of wound: acute versus chronic
c. Progression of local or systemic symptoms: improving, stable, or deteriorating
d. Prior treatment of wounds and effectiveness of interventions
G. Considerations Across the Life Span
1. Young adulthood: neuropathic changes can develop in young adults with type I DM if disease poorly controlled for extended period of time
2. Women of childbearing age: diabetic foot ulcers unlikely in gestational diabetes due to short duration of illness
3. Elderly: highest risk for ulceration due to longevity of disease process and other co-morbidities, especially atherosclerosis
 V. Diagnostic Study Findings
V. Diagnostic Study Findings
A. Laboratory
1. Glucose, electrolytes, HbA1c to determine diabetic control
2. Acetone if indicated or insulin-dependent diabetes mellitus
3. Creatinine and microalbumin to detect nephropathy from longstanding or uncontrolled diabetes
4. Albumin and total lymphocyte count to determine nutritional status
5. Lipid profile: hyperlipidemia connected with poor glycemic control and development of atherosclerosis in the coronary vessel as well as carotids and renal arteries
6. Complete blood count and sedimentation rate: detect infection
B. Radiologic
1. X-ray to rule out subcutaneous gas, foreign body, fracture, osteomyelitis, Charcot foot; chronic osteomyelitis: x-ray shows mottled lytic lesions
2. Observe x-ray for arterial and medial calcification which is not related to atherosclerotic occlusive disease but may prevent accurate ankle blood pressure measurement
3. Bone scan or MRI to differentiate osteomyelitis from Charcot foot
C. Special
1. Test for loss of protective sensation. Assess peripheral neuropathy with Semmes-Weinstein 5.07 (10 g) monofilament wire system test.
a. Used to evaluate neural sensory threshold and quantify the severity of peripheral neuropathy.
b. Twelve test sites: most common sites of diabetic ulcer.
c. Filament lightly pressed against skin just to point of flexing the filament: failure to detect the filament’s pressure indicates increased/high risk for ulcer formation.
2. For all patients with diabetes, perform an annual comprehensive foot examination to identify risk factors predictive of ulcers and amputations.
3. Additional testing for protective sensation includes any one of the following
a. Vibration using 128-Hz tuning fork
b. Pinprick sensation
c. Ankle reflexes
d. Vibration perception threshold (American Diabetes Association (ADA), 2011)
4. Transcutaneous Oxygen Tension Determination (TcPO2). Electrodes placed directly on the skin, the measured TcPO2 levels reflect the perfusion of the skin. In general, the TcPO2 is approximately 80% of the arterial oxygen tension (PO2). The normal TcPO2 value in a patient breathing room air is greater than 55 mm Hg. A value greater than 30 mm Hg suggests the presence of adequate tissue perfusion for wound healing to occur. Most patients with ischemic foot ulcers have a TcPO2 on the dorsum of the foot of less than 10 mm Hg.
5. If a diabetic ulcer probes to bone there is direct correlation with osteomyelitis (Grayson, Gibbons, Balogh, Levin, & Krachmer, 1995).
6. Vascular studies
a. Ankle–arm indices; ankle–brachial indices: Ankle–arm index of the affected limb of less than 0.5 has high risk of ischemia and is in need of revascularization in order to heal wound
b. Vascular laboratory criteria for prediction of foot lesion healing: ABI normal is 1.0. Probability for wound healing and degree of ischemia is directly proportional to declining values. Must also assess wave forms to observe a correlation relationship
c. Arterial Doppler waveform analysis
1) Diagnostic pressures in Doppler testing are higher in diabetics because of greater degree of atherosclerosis and calcification in vessels and need for higher pressure to compress these arteries
2) Toe pressure should always be measured in the diabetic secondary to noncompressible larger vessels. Normal brachia/toe pressure indices is 0.7
d. Arteriography and/or digital subtraction angiography: for locating blockage and determining feasibility of vascular surgery
1) Carries risk and should be used only as preoperative diagnostic technique. May also be helpful to have stenting prior to surgery (usually of larger iliac and femoral arteries) as well to enhance or eliminate need for surgery
2) Check creatinine and hydrate well if procedure is required
e. Magnetic Resonance Angiography (MRA): one of the most advanced developments in magnetic resonance imaging is the MRA which can evaluate blood flow and identify blockages in arteries and veins (refer to Chapter 5, Vascular Diagnostic Studies)
1) Minimally invasive, no radiation exposure
2) Selected patients per practitioner
 VI. Medical Management
VI. Medical Management
A. Offloading: use of an orthotic device allows the patient to ambulate on a limited basis as well as provide pressure relief to the heel in bedbound patients.
1. Devices redistribute plantar pressures evenly, protect vulnerable margins, protect the sheering effect when patients push with their heels to sit up as well as shift pressure to area of the foot that can bear more stress.
2. Examples include commercial boot for heel offloading and the wedge shoe to prevent pressure on the forefoot.
3. May also require crutches, wheelchair, or bedrest (total non–weight bearing rarely practical)
B. Infection Control
1. Up to one fourth of diabetic foot wounds contain anaerobes as well as aerobes. Assure that gram-positive and negative coverage is extended.
2. Deep tissue cultures are the best way to assess bacterial growth. Surface swabbing is inconclusive.
3. An infected diabetic foot ulcer can lead to limb loss in a matter of days, but not all ulcers are infected.
a. Many wounds have bacterial colonization, with the distinction between this and infection being difficult
b. Clinical signs are the most reliable indicators. The presence of swelling, pus, and loss of control of blood glucose levels usually dictates the need for antibiotics
4. Pain in a numb foot is a worrisome finding.
5. With severe infection, there may be crepitus owing to gas formation and fluctuance indicating abscess.
6. The most common organisms include staphylococci, streptococci, gram-negative organisms, and anaerobes. MRSA has become an increasing problem.
7. Osteomyelitis should be suspected in a deep ulcer if a sinus tract is present or the ulcer fails to heal (Deery & Sangeorzan, 2001; Shaw & Boulton, 2001)
C. Edema Reduction: leg elevation above the level of the heart if tolerated by patient level of pain related to ischemia in the lower extremity.
D. Enzymatic Debriding Agents: enzymes or solutions applied to devitalized tissue in the wound for the purpose of selective debridement. Able to lyse fibrin, denatured collagen, elastin but not normal tissue.
E. Total Contact Cast: complete offloading of wound with medication placed at wound site. Covered with plaster casting. Disadvantage: unable to visualize wound and reassess ability to heal.
F. Autolysis: involves the use of moisture-retentive dressings
1. Occlusive, semi-occlusive and nonocclusive that cover the wound and allow enzymes normally present in wound fluids to self-digest devitalized tissue.
2. Conservative approach and may require 3 to 7 days to accomplish.
3. Effective, inexpensive, and painless.
4. Autolysis with occlusion is contraindicated when infection is present
 VII. Surgical Management
VII. Surgical Management
A. Goals of Diabetic Foot Surgery
1. Establish drainage
2. Remove infected necrotic soft tissue or bone
3. Correct deformity
4. Reduce risk of ulceration or amputation
5. Restore stability and alignment
6. Preserve function
7. Achieve cosmetically acceptable result
8. Prevent major limb amputation (Edmonds, Foster, & Sanders, 2004)
B. Types of Procedures (Edmonds et al., 2004)
1. Elective
a. Correction of defect in a patient with intact sensation, adequate perfusion, and well-controlled diabetes
b. Risks and benefits similar as for nondiabetic patient
c. Example: bunion correction
2. Prophylactic
a. Procedures necessary to prevent further problems or ulcerations/wounds
b. “At risk” foot: neuropathic, insensate, deformity
c. Examples: stable Charcot foot with residual deformity that cannot be accommodated by shoe or brace; correction of hammer toe deformity; lengthening of Achilles tendon
3. Emergent
a. Usually present with serious foot infection; signs of systemic infection present or not present
b. Rapid assessment to distinguish between limb-threatening versus life-threatening wound
c. Requires immediate hospitalization for treatment of infection and surgery; antibiotics alone usually inadequate to control infection
1) Incision and drainage
2) Wound exploration
3) Debridement of necrosis
4) Revascularization
5) Amputation
C. Indications for Revascularization via dorsalis pedis artery bypass or popliteal to dorsalis pedis artery bypass graft with and without superficial femoral artery balloon angioplasty (refer to Chapter 9, Lower Extremity Arterial Disease).
1. Tissue necrosis in the presence of moderate-to-severe ischemia (limb salvage) (Pomposelli & Campbell, 2002)
a. Ischemic heel ulcers
b. Ischemia complicated by foot infection
2. Presence of an outflow artery in direct continuity with the foot (Yao & Pierce, 2001)
3. Multilevel occlusive disease with poor distal runoff
4. Disabling rest pain (Dale, 1985)
5. Active infection must first be controlled before dorsalis pedis bypass. Adequate control implies resolution of cellulitis, lymphangitis, and edema; especially in areas of proposed incisions required to expose the distal artery of saphenous vein
D. Contraindications for Revascularization
1. Bedridden patient with no hope of ever ambulating/bearing weight (Dale, 1985); may vary depending on surgeon’s discretion and patient’s risk assessment.
2. Advanced disease states: for example, malignancy in a patient for whom predicted death is within 6 months may be more amendable to primary amputation (Dale, 1985).
3. Relative contraindications
a. Careful consideration should be used in patients with unstable or irreversible pulmonary, cardiac, hepatic, or cerebral disease states
b. If comorbid disease states are stable or reversible, a vascular repair under spinal anesthesia is indicated
c. Preoperative evaluation with specific comorbid risk factor analysis is warranted
d. Absence of autologous venous conduit: prosthetic graft material is not ideal for distal bypasses (below the knee), although composite or prosthetic grafts have been used if other options are limited (Hughes et al., 2004; Yao & Pierce, 2001)
E. Preoperative Evaluation
1. Thorough physical examination with aggressive management of diabetes and medical comorbidities
a. Cardiovascular, renal, peripheral vascular, and infectious disease consults may be indicated
b. Nutritional status
2. Noninvasive arterial examination
3. Perform contrast angiography with digital subtraction to include complete infrapopliteal circulation including foot vessels. Anteroposterior and lateral foot views should be included to differentiate branch vessels and to visualize all stenosis (Yao & Pierce, 2001). MRA may be used as an alternative
F. Technical Considerations, Results, and Risks of Distal Bypass Procedures
1. Proximal bypass to the popliteal or proximal tibioperoneal arteries may restore foot pulses, but these are often not robust enough to normalize arterial pressure in the target area and subsequently heal a diabetic heel ulcer.
a. Peroneal bypass: not in continuity with the foot vessels; reserved for rare instances where there is no dorsalis pedis or posterior tibial artery or insufficient venous conduit; more distal reconstruction often needed to heal wounds of the forefoot (Yao & Pierce, 2001).
b. Autogenous vein grafting to the dorsalis pedis artery with subsequent anastomosis to tarsal, plantar, and malleolar or paramalleolar arteries: skin bridging with preliminary subcutaneous graft tunneling will avoid ischemia owing to tension (Pomposelli & Campbell, 2002; Yao & Pierce, 2001).
2. Results
a. Five-year patency rates to the pedal arteries are reported to be 68% to 80% with limb salvage of 87% to 90% (Pomposelli & Campbell, 2002; Roddy et al., 2001).
b. Review experience of lower extremity revascularization in a largely diabetic population of nearly 1,000 patients observed 5 years or longer: a total of 962 vein grafts were performed on 843 patients, of which 83% (795 grafts) were in patients with diabetes. Minimum follow-up was 5 years and extended up to 9 years. The dorsalis pedis or plantar/tarsal arteries served as the outflow artery in 271 (35%) of the diabetic patients. Cumulative primary graft patency was 74.7% overall, with no difference among patients with and without diabetes (diabetic, 75.6% vs. nondiabetic, 71.9%; P = NS). Most importantly, 5-year limb salvage and survival rates were virtually identical in diabetic and nondiabetic patients. The overall limb salvage rate was 87.1% (diabetic, 87.3% vs. nondiabetic, 85.4%; P = NS). Survival at 5 years was 58.1% in the entire cohort (diabetic, 58.2% vs. nondiabetic, 58.0%; P = NS) (Akbari et al., 2000).
c. These data strongly emphasize that concern for long-term mortality, limb loss, and graft patency in diabetic patients is unwarranted and should not prevent aggressive attempts at distal bypass required for limb salvage.
3. Risks: graft infection, repeat operations, postoperative lymphedema, limb loss, and death often related to high cardiovascular risks (Nehler, Hiatt, & Taylor, 2003).
4. Distal bypass graft failure and outcomes (Domenig et al., 2005).
a. Early failure: occurs within 30 days of surgery and usually results in amputation; further intervention to maintain graft patency is futile.
b. Late failure: occurs after 30 days postoperatively; rate of amputation is lower owing to higher rate of successful graft revision and lower occurrence of critical limb ischemia.
G. Management of Gangrene/Necrosis
1. Wet gangrene: odorous wet wound with swelling, necrosis, and erythema.
a. Acute immediate need to remove gangrenous area surgically to salvage limb
b. Gas (crepitus or crackling of soft tissues) is a serious finding requiring immediate surgical drainage of all affected areas and intravenous antibiotics
c. Initiate intravenous antibiotics with hospitalization and workup for limb salvage, revascularization, or amputation
2. Dry gangrene: chronic dry black eschar
a. Protect and keep dry until workup of limb salvage completed.
b. Revascularization may be needed, after which the gangrenous area can be surgically debrided or amputated.
c. Auto-amputation (digit falls off without surgical intervention) of dry gangrenous toe is painless and safe as long as digit remains dry.
H. Amputation of Diabetic Foot (refer to Chapter 25, Amputation)
1. Nonemergent
a. Neuropathic feet with structural impairment leading to recurrent nonhealing wounds
b. Intact circulation and controlled infection
2. Emergent
a. Gangrene, severe soft tissue infection, osteomyelitis, peripheral vascular disease, trauma
b. Level of amputation determined by extent of healthy tissue and blood supply
3. Ideal wound healing criteria (Edmonds et al., 2004)
a. Tissue oxygen perfusion (TcPO2) >30 mm Hg
b. Toe pressured >60 mm Hg or toe–brachial index >0.60
c. Ankle–brachial index >0.50
d. Serum albumin >3.0 g/dL
e. Serum protein >6.0 g/dL
f. Total lymphocyte count >1,500
g. Medically stable with diabetes and infection under control
4. Types of foot amputations
a. Digital: used for fixed deformity, osteomyelitis, recurrent tip ulcers
b. Ray: excision of toe and metatarsal; may lead to new pressure point ulceration
c. Transmetatarsal and midfoot, including Lisfranc and Chopart
d. Procedures for Charcot foot: ostectomy of prominent plantar, medial, or lateral bones; arthrodesis to stabilize neuropathic joints via open reduction and internal fixation
 VIII. Wound Care
VIII. Wound Care
A. Assessment
1. Presence of infection: if infection is suspected, avoid occlusive dressings
2. Amount of wound drainage
3. Size of wound, including depth and tunneling
4. Wound base: granulation tissue, fibrinous slough, necrosis, eschar, bone
5. Periwound skin: erythematous, warm, pale or cool, cyanotic, tender, thin or dry, calloused
6. Limb: insensate, edematous, pale, cool, cyanotic, warm, or erythematous
B. Phases of Wound Healing: wound healing is a physiologic process that involves a series of sequential yet overlapping stages.
1. Homeostasis occurs immediately at the time of injury. During hemostasis a provisional matrix seals the injury site and initiates the process of wound healing.
2. Inflammation is triggered by a variety of mediators released from injured tissue cells and capillaries, activated platelets and their cytokines, and the by-products of hemostasis.
3. The wound surface is covered with new skin, and vascular and structural integrity is restored as granulation tissue fills the defect.
4. Remodeling is responsible for maturation of the granulation tissue into mature connective tissue, scar, or both.
5. A thorough understanding of wound healing physiology is an important prerequisite to providing care that optimizes wound healing and prevents unnecessary complications.
6. Wound dressings are now considered interactive products able to affect the microenvironment of the wound to promote rapid wound healing.
C. Wound Goals and Treatments: management goals to consider
1. The etiology of the wound
2. Contributing factors and local wound care
3. Practical, consistent, and takes into consideration the overall health and lifestyle of the patient
4. Management goals or patient outcomes may vary depending on the general health of the host and the severity of the injury
5. Odor control: odor management is achieved through control of bacteria levels. It includes removal of devitalized tissue and modulating the amount of exudate in the wound
D. Select Primary Dressing Based on Exudates and Wound Bed Appearance
1. Dry: apply moist dressing, such as wound gel
2. Mild-to-moderate drainage: light absorbent, such as hydrocolloid
3. Heavily draining: absorbent, such as alginate
4. Fibrinous slough: autolytic debridement or chemical debridement agent
5. Hard, dry eschar: may require sharp surgical debridement before dressing application
E. Wound and Limb Protection
1. Pain management: a significant decrease in pain perception has been reported with moisture-retentive dressings. Moisture also limits mechanical damage to tissues during dressing removal. Always premedicate before dressing removal, with the exception being the insensate foot.
2. Periwound protection: use of skin sealant and barriers before dressing application.
3. Off-load pressure from wound and limb as listed in Medical Management.
4. Keep extremity warm; use protective socks and closed-toe shoes if possible.
5. If the patient can wear shoes, select extradepth, extrawidth shoes with orthotic linings to off-load pressure points.
6. Perform close monitoring for signs/symptoms of infection or change in appearance.
 IX. Nursing Diagnoses
IX. Nursing Diagnoses
A. Impairment of Skin Integrity Related to Diabetic Foot Disease (Datta, 2001; Fahey & Schindler, 2004; Gibson, 2001; MacVittie, 1998)
1. Assessment for defining characteristics
a. Change in appearance of wound and surrounding tissues
b. Change in vital signs
c. Increased weakness
2. Expected outcome: infection will not spread and wound will heal preventing amputation of area and lower leg
3. Nursing interventions
a. Assess wound and provide wound care as directed
b. Do not use tape on skin but apply tape to gauze wrap
c. Protect affected extremity with bed cradle, use of heel guards, offloading
d. Monitor vital signs for increased signs of infection
e. Administer IV antibiotics as directed
f. Absolute need to refrain from walking on infected area; will need wheelchair, crutches, or bed rest
g. Nutrition: consults dietitian for proper diet; weight loss diet not appropriate at this time.
4. Evaluation of nursing care
a. All changes in status are recorded and reported immediately.
b. Medicines and dressing changes are performed in timely manner.
B. Alteration in Tissue Perfusion Relating to Impaired Peripheral Vascular Function (Bryant, 2001; Fahey & Schindler, 2004; MacVittie, 1998)
1. Assessment for defining characteristics
a. Change in pulse quality, capillary refill time
b. Change in skin color, temperature
2. Expected outcome: patient will maintain tissue perfusion
3. Nursing interventions
a. Avoid smoking: refer to smoking cessation program
b. Avoid vasoconstrictive drugs
c. Avoid constricting clothing, crossing of legs, tight bandages
d. Avoid long periods of standing or sitting that may cause tourniquet effect on circulation resulting in pooling of blood and edema of dependent tissues; muscle action facilitates venous return
e. Monitor for cool skin, tingling, pallor, poor capillary refill time, the presence of petechiae, and mottling of limbs
4. Evaluation of nursing care: skin remains intact, warm, and with appropriate color, with brisk capillary refill and pulses intact
C. Disturbance in Self-Concept Related to Wounds and Treatments (Fahey & Schindler, 2004; Gibson, 2001; MacVittie, 1998)
1. Assessment for defining characteristics
a. Disease state requires changes of lifestyle, long-term prognosis is uncertain
b. Mood change or depression
c. Self-destructive or unhealthy health behaviors
2. Expected outcome: patient will have a positive body image
3. Nursing interventions
a. Assess level of acceptance and adaptation of patient and significant others
b. Encourage verbalization of fears and life changes
c. Explain procedures and tests involved; allow patient to verbalize fears
d. Refer for counseling as needed
e. Establish a trusting relationship
f. Promote social interaction
4. Evaluation of nursing care
a. Patient is able to take responsibility for life style changes needed
b. Patient and significant other acknowledge ongoing care and treatment needed
D. Potential Knowledge Deficit of Management of Diabetes; Impairment in Metabolic State
1. Assessment for defining characteristics
a. Chronic hyperglycemia
b. Obesity
c. Hypertension
d. Self-management of diabetes
2. Expected outcomes
a. Diabetes will be under acceptable control
b. Patient will take responsibility for self-management at home
3. Nursing interventions
a. Monitor blood glucose and electrolytes; I & O, daily weights
b. Correct factors that precipitate development of diabetic ketoacidosis
c. Avoid fluctuations in blood sugar to prevent hyperglycemia and hypoglycemia
d. Assess need for referral for psychosocial counseling
e. Assess and review medication administration, importance of dietary regulation, and weight control
f. Teach and reinforce importance of home glucose monitoring
g. Consult with dietitian if needed
4. Evaluation of nursing care
a. Blood sugar remains in normal range (70 to 110 mg/dL)
b. Patient expresses understanding of medication and administration
c. Patient expresses understanding of diabetes and its complications, glucose monitoring, diet, and weight control (American Diabetes Association(ADA), 2004b; Gibson, 2001; MacVittie, 1998)
E. Potential for Infection Related to Diabetes
1. Assessment for defining characteristics
a. Change in vital signs
b. Change in skin integrity or wound appearance
2. Expected outcome: infection will resolve; patient will remain free of infection
3. Nursing interventions
a. Assess for fever, cellulitis, wound drainage, and elevated white blood cell count
b. Use aseptic technique for dressing changes
c. Administer antibiotics as directed
4. Evaluation of nursing care
a. Patient remains afebrile
b. Wound size decreases and is without drainage, redness, increased warmth, or odor (Fahey & Schindler, 2004; Gibson, 2001; MacVittie, 1998)
 X. Patient Teaching
X. Patient Teaching
A. Disease Prevention/Health Promotion
Since diabetes often causes the feet to become less sensitive and not feel pain, you have to look at your feet to find a problem.
1. Using a good light, inspect your feet and between the toes every day for blisters, corns, cuts, and sores. Use a mirror to see the bottoms of your feet or have a family member help you (see Fig. 22-2).
2. Do not soak your feet as soaking dries out the skin, but do wash your feet every day with mild soap and warm water. Test the water with your elbow before putting your feet in.
3. Dry the feet well but carefully, especially between the toes, by blotting with the towel; be gentle.
4. Use a nonperfumed, moisturizing lotion on your feet immediately after washing and drying them to seal in the moisture. Do not put lotion between the toes, as this area must be kept dry. Report any sign of fungal infection immediately.
5. Clippers should be used to cut your toenails, but it is recommended that someone trained in diabetic foot care cut your toenails. You may use a cardboard emery board and file straight across the nail, but do not use scissors or a metal file.
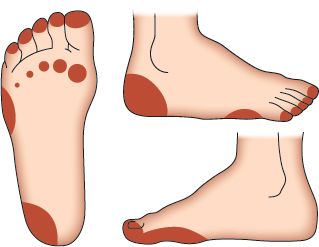
FIGURE 22.2 Pressure areas on the foot.



