The Woman with an Intrapartum Complication
Learning Objectives
After studying this chapter, you should be able to:
• Explain abnormalities that may result in dysfunctional labor.
• Describe maternal and fetal risks associated with premature rupture of the membranes.
• Analyze factors that increase a woman’s risk for preterm labor.
• Explain maternal and fetal problems that may occur if pregnancy persists beyond 42 weeks.
• Describe common intrapartum emergencies.
• Explain therapeutic management of each intrapartum complication.
• Apply the nursing process to care of women with intrapartum complications and to their families.
![]()
http://evolve.elsevier.com/McKinney/mat-ch
Birth is usually free of major complications. Sometimes, however, complications make childbearing hazardous for the woman or her baby. The nurse’s challenge is to identify and manage the complications promptly and to provide effective care for these mothers while supporting the entire family at this significant time in their lives.
Dysfunctional Labor
Normal labor is characterized by progress. Dysfunctional labor is one that does not result in normal progress of cervical effacement, dilation, and fetal descent. Dystocia is a general term that describes any difficult labor or birth. A dysfunctional labor may result from problems with the powers of labor, the passenger, the passage, the psyche, or a combination of these. Dysfunctional labor is often prolonged but may be unusually short and intense. Combined medical and nursing care is indicated for care of the woman having dysfunctional labor.
An operative birth (vacuum extractor- or forceps-assisted or cesarean) may be needed if dysfunctional labor does not resolve or if fetal or maternal compromise occurs. Signs that indicate the need for an operative birth include persistent nonreassuring fetal heart rate (FHR) patterns (see Chapter 17), fetal acidosis, and meconium passage. Maternal exhaustion or infection may occur, especially during long labors.
Problems of the Powers
The powers of labor may not be adequate to expel the fetus because of ineffective contractions or ineffective maternal pushing efforts.
Ineffective Contractions
Effective uterine activity is characterized by coordinated contractions that are strong and numerous enough to propel the fetus past the resistance of the woman’s bony pelvis and soft tissues. It is not possible to say how frequent, long, or strong labor contractions must be. One woman’s labor may progress with contractions that would be inadequate for another woman. Possible causes of ineffective contractions include:
• Fluid and electrolyte imbalance
• Excessive analgesia or anesthesia
• Maternal catecholamines secreted in response to stress or pain
• Disproportion between the maternal pelvis and the fetal presenting part
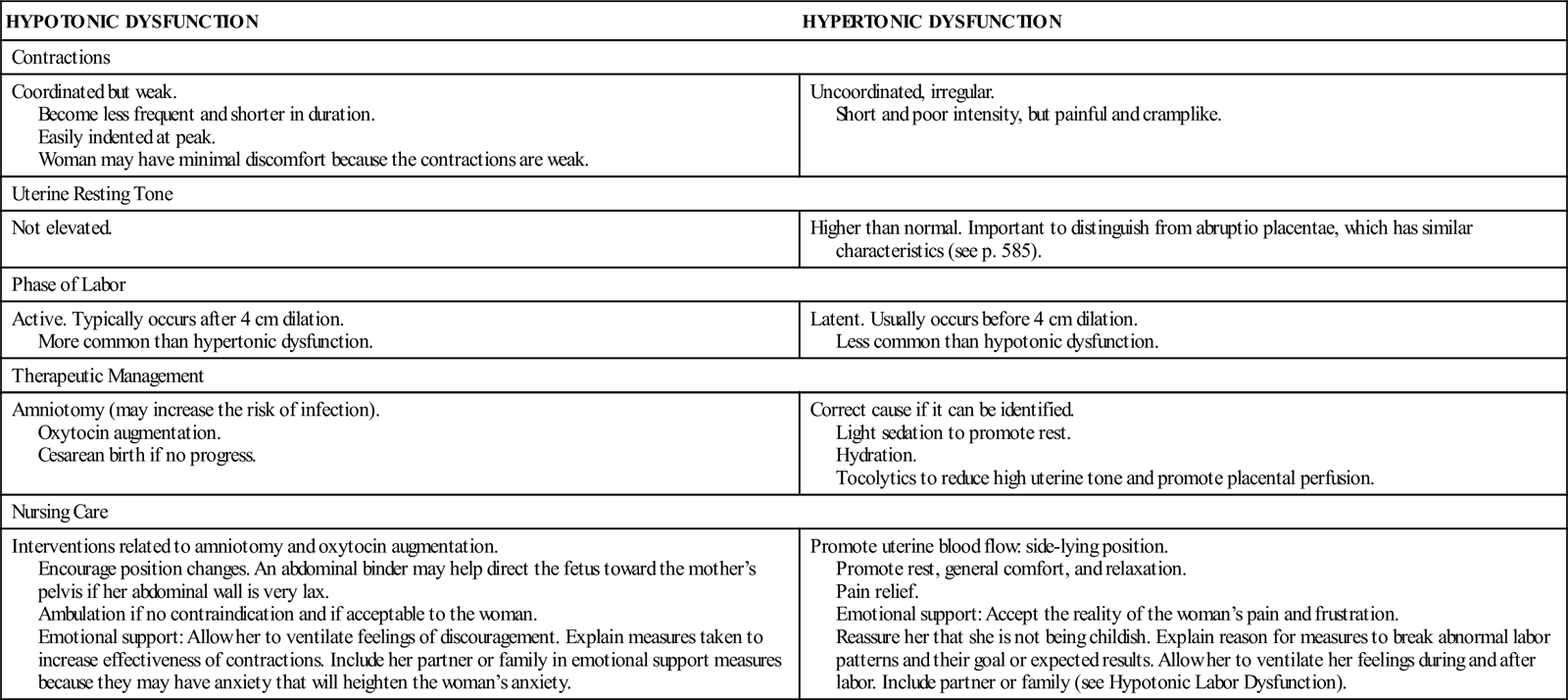
Two patterns of ineffective uterine contractions are hypotonic and hypertonic dysfunction (Table 27-1). Hypotonic dysfunction is more common than hypertonic. Characteristics and management of each are different, but the result—poor labor progress—is the same if they persist.
TABLE 27-1
| HYPOTONIC DYSFUNCTION | HYPERTONIC DYSFUNCTION |
| Contractions | |
| Coordinated but weak. Become less frequent and shorter in duration. Easily indented at peak. Woman may have minimal discomfort because the contractions are weak. | Uncoordinated, irregular. Short and poor intensity, but painful and cramplike. |
| Uterine Resting Tone | |
| Not elevated. | Higher than normal. Important to distinguish from abruptio placentae, which has similar characteristics (see p. 585). |
| Phase of Labor | |
| Active. Typically occurs after 4 cm dilation. More common than hypertonic dysfunction. | Latent. Usually occurs before 4 cm dilation. Less common than hypotonic dysfunction. |
| Therapeutic Management | |
| Amniotomy (may increase the risk of infection). Oxytocin augmentation. Cesarean birth if no progress. | Correct cause if it can be identified. Light sedation to promote rest. Hydration. Tocolytics to reduce high uterine tone and promote placental perfusion. |
| Nursing Care | |
| Interventions related to amniotomy and oxytocin augmentation. Encourage position changes. An abdominal binder may help direct the fetus toward the mother’s pelvis if her abdominal wall is very lax. Ambulation if no contraindication and if acceptable to the woman. Emotional support: Allow her to ventilate feelings of discouragement. Explain measures taken to increase effectiveness of contractions. Include her partner or family in emotional support measures because they may have anxiety that will heighten the woman’s anxiety. | Promote uterine blood flow: side-lying position. Promote rest, general comfort, and relaxation. Pain relief. Emotional support: Accept the reality of the woman’s pain and frustration. Reassure her that she is not being childish. Explain reason for measures to break abnormal labor patterns and their goal or expected results. Allow her to ventilate her feelings during and after labor. Include partner or family (see Hypotonic Labor Dysfunction). |
Hypotonic Labor Dysfunction
Hypotonic contractions are coordinated but are too weak to be effective. They are infrequent and brief and can be easily indented with fingertip pressure at the peak.
Hypotonic dysfunction, or secondary arrest, usually occurs during the active phase of labor, when progress normally quickens. Uterine overdistention is associated with hypotonic dysfunction because the stretched uterine muscle contracts poorly.
The woman may be fairly comfortable because her contractions are weak. Persistent hypotonic dysfunction is fatiguing and frustrating for the mother. Fetal hypoxia is not usually seen with hypotonic labor.
Management depends on the cause. Providing intravenous (IV) or oral fluids corrects maternal fluid and electrolyte imbalances or hypoglycemia. Maternal position changes, particularly upright positions, including walking or showering, favor fetal descent and promote effective contractions. The woman who moves about actively typically has better labor progress and is more comfortable than one who remains in one position. Pain management techniques such as epidural block may have outcomes that reduce contraction effectiveness, requiring interventions specific to that factor. Effective pain management may improve progress of labor, however.
The nurse should use therapeutic communication to help the woman identify anxieties or beliefs about labor and its progress. Helping her to get her anxieties in the open is the first step to managing them effectively so the stress response does not slow her labor.
Some women need measures such as amniotomy or oxytocin infusion to promote labor progress. The birth attendant evaluates the woman’s labor to confirm that she is having hypotonic active labor rather than a long latent phase (about the first 3 cm of dilation) of labor. The maternal pelvis and fetal presentation and position are assessed to identify problems.
Amniotomy or oxytocin augmentation (see Chapter 19) may be used to stimulate a labor that slows after it is established. Reduced placental perfusion caused by excessive uterine contractions is the most common risk of oxytocin labor augmentation (Cunningham, Leveno, Bloom, et al., 2010; Gee, 2011; Thorp, 2009).
Hypertonic Labor Dysfunction
Hypertonic dysfunction of labor is less common than hypotonic. Contractions are uncoordinated and erratic in their frequency, duration, and intensity. The contractions are painful but ineffective. Hypertonic dysfunction usually occurs during the latent phase of labor.
The uterine resting tone between contractions is high, reducing uterine blood flow. This ischemia decreases fetal oxygen supply and causes the woman to have almost constant cramping pain. Because high resting tone and constant pain are also seen in abruptio placentae (premature separation of the normally implanted placenta), this complication should be considered as well.
The mother becomes very tired because of long yet nonproductive discomfort. She may lose confidence in her ability to cope with labor and give birth. Frustration and anxiety further reduce her pain tolerance and interfere with normal processes of labor. The nurse should accept her frustration and discomfort. It is important not to equate cervical dilation with the amount of pain a woman “should” experience.
Management of hypertonic labor depends on the cause. Relief of pain is the primary intervention to promote a normal labor pattern. Warm showers or baths promote relaxation and rest, often allowing a normal labor pattern to ensue. Systemic analgesics for therapeutic rest or epidural analgesia may be needed to achieve this purpose.
Oxytocin is not usually given because it can intensify the already high uterine resting tone. Very low doses of oxytocin, however, sometimes promote coordination of uterine contractions. Amniotomy may be done if the hypertonic contractions occur in active labor. Tocolytic drugs (inhibit uterine contractions) may be ordered to reduce uterine resting tone and improve placental blood flow (Cunningham et al., 2010; Gee, 2011).
Ineffective Maternal Pushing
A reflex urge to push with contractions usually occurs as the fetal presenting part reaches the pelvic floor during second-stage labor. Ineffective pushing may result from:
• Use of incorrect pushing techniques or inefficient pushing positions
• Fear of injury because of pain and tearing sensations felt by the mother when she pushes
• Minimal or absent urge to push
• Regional block analgesia that may suppress the woman’s urge to push
Management focuses on correcting the causes contributing to ineffective pushing. If maternal and fetal vital signs are normal, there is no maximum allowable duration for the second stage. Each woman is evaluated individually by her birth attendant to determine whether labor should be ended with an operative delivery or can continue safely (see Chapter 16). Nursing care to promote effective pushing helps the mother make each effort productive. Upright positions such as squatting add the force of gravity to her efforts. Semi-sitting, side-lying, and pushing while sitting on the toilet are other options. Regional analgesia methods may restrict possible maternal positions and may alter a woman’s spontaneous urge to push. Conversely, women who have regional pain management often feel an adequate urge to push that is not complicated by excess pain.
The woman who fears injury because of the sensations she feels when she pushes may respond to accurate information about the process of fetal descent. If she understands that sensations of tearing often accompany fetal descent but that her tissues can expand to accommodate the baby, she may be more willing to push with contractions.
The woman who is exhausted may push more effectively if she is encouraged to rest until she feels the urge. Encouraging her to push with intermittent contractions, such as every other contraction, also allows her to maintain adequate pushing effort. Oral or IV fluids provide energy for the strenuous work of second-stage labor. Reassuring the woman if there is no apparent fetal or maternal harm to a prolonged second stage may encourage her. Remind her that there is progress as the baby moves down through the pelvis although the mother is not pushing for a period of time.
Problems with the Passenger
Fetal problems associated with dysfunctional labor are those related to:
These variations may cause mechanical problems and contribute to ineffective contractions.
Fetal Size
Macrosomia
The macrosomic infant weighs more than 4000 g (8 lb, 13 oz) at birth, although some authorities define it as a weight of 4500 g (9 lb, 15 oz) or greater. The head or shoulders may not be able to adapt to the pelvis, known as cephalopelvic, or fetopelvic, disproportion (CPD). In addition, distention of the uterus by the large fetus reduces the strength of contractions both during and after birth.
Size is relative, however. The woman with a small pelvis or one that is abnormally shaped may not be able to deliver an average-size or small infant. A woman with a large pelvis may easily give birth to an infant heavier than 4000 g. Fetal position as the baby descends through the pelvis is another important factor in terms of fetal size and maternal pelvic size.
Shoulder Dystocia
Delayed or difficult birth of the shoulders may occur as they become impacted above the maternal symphysis pubis. As soon as the head is born, it retracts against the perineum, much like a turtle’s head drawing into its shell (“turtle sign”). Failure of the shoulders to complete external rotation is another sign (see Figure 16-12). Nursing interventions to help rotate the fetal head and promote descent also may help prevent a shoulder dystocia (Simpson, 2008).
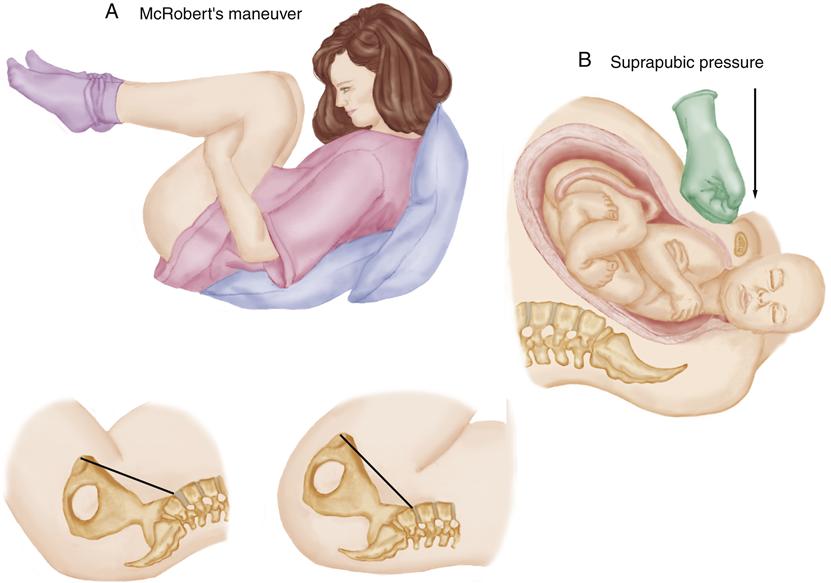
Shoulder dystocia is unpredictable and can occur in a baby of any weight. This complication requires urgent intervention by available physicians, midwives, nurses, anesthesia personnel, and neonatology staff because the umbilical cord is compressed, but chest compression within the vagina prevents respirations. Any of several methods may be used to relieve the impacted fetal shoulders quickly (Figure 27-1). The infant’s clavicles should be checked for crepitus, deformity, or bruising, each of which suggests fracture. Nerve injury to the brachial plexus, or Erb’s palsy, may cause flaccid muscle tone on the affected side. Most cases of Erb’s palsy resolve in a few weeks, but exercises and physical therapy may be started in the immediate postbirth period (American College of Obstetricians and Gynecologists [ACOG], 2010c; Cunningham et al., 2010; Gherman, 2011).
Abnormal Fetal Presentation or Position
An unfavorable fetal presentation or position may interfere with cervical dilation or fetal descent.
Rotation Abnormalities
Persistence of the fetus in the occiput posterior (OP) or occiput transverse (OT) position can contribute to dysfunctional labor and possible shoulder dystocia. These positions delay fetal descent and other mechanisms of labor (cardinal movements). Most fetuses in an OP position during early labor rotate spontaneously to an occiput anterior position while descending through the pelvis, promoting normal extension and expulsion of the head. Some women with a large pelvis relative to the fetal size may be able to deliver their fetus in the OP position.
Labor is usually longer and more uncomfortable when the fetus is in the OP or OT position. Intense back or leg pain that is poorly relieved with analgesics makes it difficult for the woman to cope with labor. “Back labor” aptly describes the sensations a woman feels when her fetus is in an OP position.
Maternal position changes promote fetal head rotation to an occiput anterior position and fetal descent (see Chapter 16). Examples are:
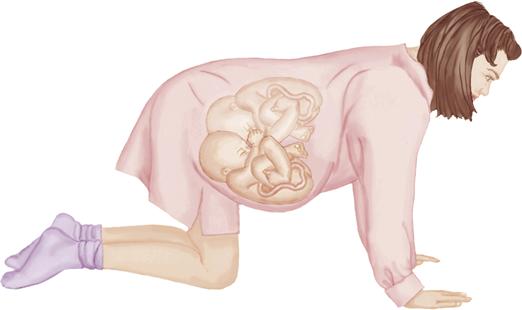
• Hands and knees. Rocking the pelvis back and forth while on hands and knees encourages rotation.
• Squatting (for second-stage labor).
Using a birthing ball—a large plastic ball capable of supporting an adult’s weight—helps support the woman when in the hands-and-knees position. She can also sit on it, providing many of the benefits of squatting. In addition, the woman tends to move her hips back and forth, favoring fetal descent.
Upright maternal positions promote descent, which is usually accompanied by fetal head rotation. The hands-and-knees and the side-lying positions promote rotation because the mother’s abdomen is dependent in relation to her spine. The convex surface of the fetal back tends to rotate toward the convex anterior uterus, similar to nesting two spoons together (Figure 27-2). Moreover, these positions decrease the mother’s discomfort by reducing fetal head pressure on her sacrum. A side-lying position has a similar effect.
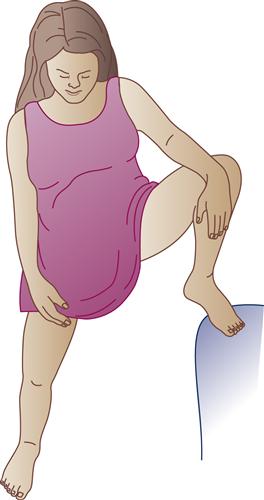
The lunge widens the side of the pelvis toward which the woman lunges. If the fetal position is known, she lunges toward the side where the occiput is located (Figure 27-3). If the fetal position is not known, the woman can lunge toward the side that gives her greater comfort.
All variations of the squatting position aid rotation and fetal descent by straightening the pelvic curve and enlarging the pelvic outlet. They also add gravity to the force of maternal pushing.
If spontaneous rotation does not occur, the physician may assist rotation and descent of the head with a vacuum extractor or forceps. Some types of vacuum extractors cannot be applied to the fetal head when it remains in an OP position. Cesarean birth may be needed if forceps or vacuum extractor use is not successful.
Deflexion Abnormalities
The poorly flexed fetal head presents a larger diameter to the pelvis than if flexed with the chin on the chest (see Figure 16-8). In the face presentation, the head diameter is similar to that of the vertex presentation, but the maternal pelvis can be traversed only if the fetal chin (mentum) is anterior.
Breech Presentation
Cervical dilation and effacement are often slower when the fetus is in a breech presentation because the buttocks or feet do not form a smooth, round dilating wedge like the head. The greatest fetal risk is that the head—the largest fetal part—is last to be born. By the time the lower body is born, the umbilical cord is well into the pelvis and may be compressed. The shoulders, arms, and head must be delivered quickly so that the infant can breathe.
A breech presentation is common well before term, but only 3% to 4% of term fetuses remain in this presentation. Most breech births in North America are by cesarean, but a surgical birth does not eliminate all problems associated with breech birth, which may include:
• Fetal injury, particularly with a difficult vaginal birth
• Fetal anomalies contributing to the breech presentation, such as hydrocephalus
External cephalic version (ECV) may be attempted to change the fetus in a breech presentation or transverse lie to a cephalic presentation (see Chapter 19). If the fetus remains in the abnormal presentation, cesarean birth is recommended to avoid complications of a difficult vaginal birth if the woman is not in active labor. A woman who first enters the labor unit in advanced active labor may have a fetus remaining in a breech presentation and perhaps a very immature fetus. In this case, ECV is not always possible and vaginal birth may be necessary simply because labor ends very quickly.
Multifetal Pregnancy
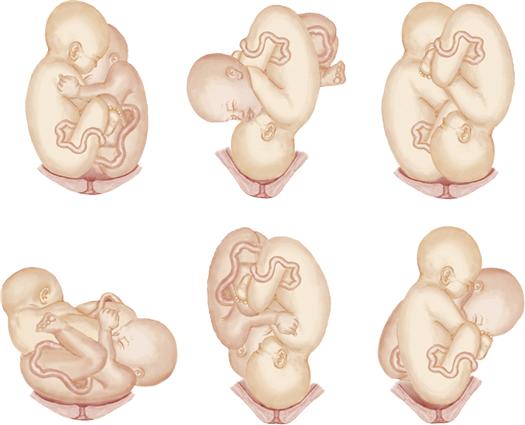
Multifetal pregnancy, also known as multiple gestation, may result in dysfunctional labor because of uterine overdistention, which contributes to hypotonic dysfunction, and abnormal presentation of one or both fetuses (Figure 27-4). In addition, the potential for fetal hypoxia during labor is greater. The risk for postpartum hemorrhage resulting from uterine atony because of uterine overdistention is greater.
Because of these problems, birth for a woman with a twin pregnancy is often cesarean, although it is also common for birth to be vaginal. Multifetal pregnancies with more than twins are most often delivered by cesarean if the gestation is viable. The physician considers fetal presentations, maternal pelvic size, and the presence of other complications, such as hypertension, as well as the multiple fetuses.
During labor, each twin’s FHR is monitored separately. When in bed, the woman should remain in a lateral position to promote adequate placental blood flow. After vaginal birth of the first twin, assessment of the second twin’s FHR continues until birth. The nurse observes for signs of hypotonic dysfunction throughout labor and for uterine atony, often related to the overdistended uterus, after birth.
Whether the birth is vaginal or cesarean, the intrapartum staff must be prepared for the care and possible resuscitation of multiple infants as with the birth of a single infant. Cord clamps, bulb syringes, radiant warmers, and resuscitation equipment must be prepared for each infant. A team of neonatal care providers such as neonatal nurses, a neonatal nurse practitioner, and a pediatrician or a neonatologist should be available to care for each infant. Another nurse should be free to care for the mother.
Fetal Anomalies
Fetal anomalies such as hydrocephalus or a large fetal tumor may prevent normal descent of the fetus. Abnormal presentations, such as breech or transverse lie, are also associated with fetal anomalies. These abnormalities may be discovered by ultrasound examination before labor. A cesarean birth is scheduled if vaginal birth is not possible or if it is inadvisable.
Problems of the Passage
Dysfunctional labor may occur because of variations in the maternal bony pelvis or because of soft tissue problems that inhibit fetal descent.
Pelvis
A small (contracted) or abnormally shaped pelvis may retard labor and obstruct fetal passage. The woman may experience poor contractions, slow dilation, slow fetal descent, and a long labor. The danger of uterine rupture (tear in the uterine wall) is greater with thinning of the lower uterine segment, especially if contractions remain strong.
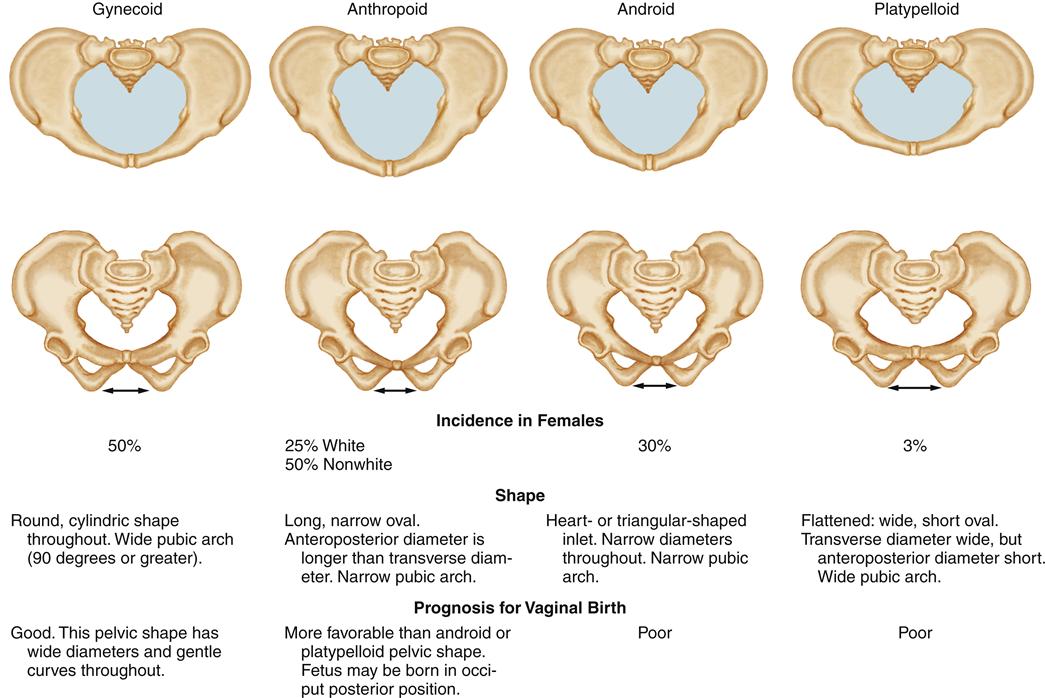
There are four basic pelvic shapes, each with different implications for labor and birth (Figure 27-5). Most women have mixed characteristics from two or more types.
Maternal Soft Tissue Obstructions
During labor, a full bladder is a common soft tissue obstruction. Bladder distention reduces available space in the pelvis and intensifies maternal discomfort. The woman should be assessed for bladder distention regularly and encouraged to void every 1 to 2 hours. Catheterization may be needed if she cannot urinate or if she receives regional block analgesia (see Chapter 18).
Problems of the Psyche
A perceived threat caused by pain, fear, nonsupport, or one’s personal situation can result in great maternal stress and interfere with normal labor progress. The woman’s perception of stress is more important than the actual existence of a threat.
The body responds to stress, preparing itself for fight or flight. Responses to excessive or prolonged stress, however, interfere with labor in several ways:
Helping the woman relax helps her body work more effectively with the forces of labor and promotes normal progress. General nursing measures involve:
• Establishing a trusting relationship with the woman and her family
• Making the environment comfortable by adjusting temperature and light
• Promoting physical comfort, such as cleanliness
• Providing accurate information
• Implementing nonpharmacologic and pharmacologic pain management
Chapters 16 and 18 describe additional methods to encourage relaxation and promote comfort, including individual and family cultural values that are part of childbirth.
Abnormal Labor Duration
An unusually long or short labor may result in maternal, fetal, or neonatal problems.
Prolonged Labor
Prolonged labor is a type of dysfunctional labor that results from problems with any of the factors in the birth process. After the woman reaches the active phase of labor, cervical dilation should proceed at a minimum rate of 1.2 cm per hour in the nullipara and 1.5 cm per hour in the parous woman. Descent of the fetal presenting part is expected to occur at a minimum rate of 1 cm per hour in the nullipara and 2 cm per hour in the parous woman (Cunningham et al., 2010; Gee, 2011; Thorp, 2009). If all previous births were by cesarean before much cervical dilation occurred, the criteria that apply to a nullipara may be applied to a multipara who is laboring.
Potential maternal and fetal problems in prolonged labor include:
• Maternal infection, intrapartum or postpartum
• Neonatal infection, which may be severe or fatal
• Higher levels of anxiety and fear during a subsequent labor
Maternal and neonatal infections are more likely if the membranes have been ruptured for a prolonged time, because organisms ascend from the vagina. The mother is more likely to have an intrapartum infection, a postpartum infection, or both.
Nursing measures for the woman who has prolonged labor include promotion of comfort, conservation of energy, emotional support, position changes that favor normal progress, and assessment for infection. Nursing care for the fetus includes observation for signs of intrauterine infection and for compromised fetal oxygenation (see Chapter 17).
Precipitate Labor
Precipitate labor is a rapid birth that occurs within 3 hours of labor onset. There is often an abrupt onset of intense contractions rather than the more gradual increase in frequency, duration, and intensity that typifies most spontaneous labors. The mother or her fetus or newborn may be affected by several conditions that can be associated with the precipitate labor. These conditions may include abruptio placentae, fetal meconium, maternal cocaine use (also may be associated with abruptio placentae in any labor), postpartum hemorrhage, or low Apgar scores for the infant (Cunningham et al., 2010).
Precipitate labor is not the same as a precipitate birth. A precipitate birth occurs after a labor of any length, in or out of the hospital or birth center, when a trained attendant is not present to assist. A woman in precipitate labor may also have a precipitate birth. The nurse should simply wear gloves while supporting the baby as it emerges. The mother’s legs should not be forced together or the fetal head held back to delay birth. Such actions can result in fetal hypoxia or other injury.
If the maternal pelvis is adequate and the soft tissues yield easily to fetal descent, little maternal injury is likely. However, trauma, such as uterine rupture, cervical lacerations, or hematoma of the vagina or vulva may occur.
The fetus may suffer direct trauma, such as intracranial hemorrhage or nerve damage, during a precipitate labor. The fetus may become hypoxic because intense contractions with a short relaxation period reduce time available for gas exchange in the placenta.
Priority nursing care of the woman in precipitate labor includes promotion of fetal oxygenation and maternal comfort. The woman should remain in a side-lying position to enhance placental blood flow and reduce the effects of aortocaval compression. An added benefit of the side-lying position is to slow the rapid fetal descent and minimize perineal tears. Additional measures to enhance fetal oxygenation include administering oxygen to the mother and maintaining adequate blood volume with nonadditive IV fluids. If oxytocin is being used, it should be stopped. A tocolytic drug is often ordered.
Promoting comfort is difficult in a precipitate labor because intense contractions give the woman little time to prepare and to use coping skills, such as breathing techniques. Pharmacologic measures (opioid analgesia or regional block) may not be useful because rapid labor progression may not allow time for them to become effective. Also possible newborn respiratory depression must be considered when opioids are given near birth. The nurse helps the woman focus on techniques to cope with pain one contraction at a time. The nurse must remain with her, to provide support and to assist with an emergency birth if it occurs.
Nursing Care
The Woman in Dysfunctional Labor
Several nursing diagnoses and collaborative problems may be appropriate in dysfunctional labor. Observing for fetal compromise should be part of all intrapartum management (see Chapter 17). Pain management is often more difficult, and the woman may find that practiced coping skills are inadequate if labor is not normal. Anxiety or fear is often higher with abnormal labor, which also may reduce the effectiveness of pharmacologic or regional block (e.g., epidural block) pain control methods. Maternal or newborn injury sometimes becomes apparent after the birth.
In addition to these problems, nursing care in this section is directed toward two other concerns: possible intrauterine infection and maternal exhaustion.
Intrauterine Infection
Assessment
Infection can occur with both normal and dysfunctional labors. Assess the FHR and maternal vital signs for evidence of infection:
Assess amniotic fluid for normal clear color and mild odor. Small flecks of white vernix are normal. Yellow or cloudy fluid or fluid with a foul or strong odor suggests infection, and vernix may be stained by discolored fluid. The strong odor may be noted before birth or afterward on the infant’s skin.
Nursing Diagnosis and Planning
For the woman without signs of infection but with risk factors, the nursing diagnosis selected is:
Expected Outcomes
Maternal temperature will remain less than 38° C (100.4° F). The electronic fetal monitoring (EFM) pattern will maintain a reassuring pattern near the baseline and below 160 bpm. The amniotic fluid will remain clear and without a foul or strong odor.
Interventions
Reducing the Risk for Infection
Nurses should wash their hands before and after each contact with the woman and her infant to reduce transmission of organisms. Use gloves and other protective wear to prevent contact with potentially infectious secretions.
Limit vaginal examinations to reduce transmission of vaginal organisms into the uterine cavity, and maintain aseptic technique during essential vaginal examinations. Keep underpads as dry as possible to reduce the moist, warm environment that favors bacterial growth. Periodically clean excessive secretions from the vaginal area in a front-to-back motion to limit fecal contamination and promote the mother’s comfort.
Identifying Infection
Assess the woman and fetus for signs of infection. Increase the frequency of assessments if labor is prolonged. If signs of infection are noted, report them to the birth attendant for definitive treatment. Note the time at which the membranes ruptured to identify prolonged rupture, which adds to the risk for infection.
The birth attendant may collect specimens after birth from the uterine cavity or placenta for culture to identify infectious organisms and determine antibiotic sensitivity. Both aerobic and anaerobic culture specimens may be collected. Transport specimens to the laboratory promptly because living organisms are required for culture and sensitivity study.
Inform the newborn staff if maternal risk factors for infection exist and if signs of infection are noted. If available, specialized caregivers such as neonatal nurse practitioners should be notified of an increased risk for newborn infection and resuscitation. Specimens of infants’ secretions may be obtained for testing after birth. Prophylactic antibiotics to prevent neonatal sepsis are often given. See Chapter 30 for additional information about neonatal infection.
Evaluation
• Did the woman’s temperature remain less than 38° C (100.4° F)?
• Did the amniotic fluid have normal characteristics?
• Did the EFM tracing have a reassuring pattern, without tachycardia?
The woman remains at higher risk for postpartum infection and should continue to be observed for signs and symptoms of infection.
Maternal Exhaustion
Assessment
Many women begin labor with a sleep deficit because of fetal movement, frequent urination, and shortness of breath associated with advanced pregnancy. As labor drags on, the mother’s reserves are further depleted.
Assess the mother for signs and symptoms of exhaustion:
Nursing Diagnosis and Planning
The intense energy demands of a dysfunctional labor may exceed a woman’s physical and psychological ability to meet them. For this reason, an appropriate nursing diagnosis is:
Expected Outcomes
The woman will rest between contractions with her muscles relaxed. She will use coping skills, such as breathing and relaxation techniques.
Interventions
Conserving Maternal Energy
Reduce factors that interfere with the woman’s ability to relax. Lower the light level and turn off overhead lights. Reduce noise by closing the door or masking it with soft music or other comforting sounds. Silence the EFM if she prefers. Maintain a comfortable maternal temperature with blankets or a fan. If there is no contraindication, a warm shower or bath is soothing.
Position the woman to encourage comfort, promote fetal descent, and enhance fetal oxygenation. Support her with pillows to reduce muscle strain and added fatigue. Help her change positions regularly (about every 30 minutes) to reduce muscle tension from constant pressure. Regular position changes also promote maternal comfort by maintaining an even distribution of regional analgesia such as an epidural block.
Even though an epidural block is a common pain relief for birth, a woman may become tense in the upper body areas that are not affected by epidural effects, such as the shoulders and upper or middle back. Several pain management methods are options for women regardless of whether they choose any medical pain relief for labor. A soothing back rub may reduce muscle tension, which increases fatigue. Firm sacral pressure or assuming some of the positions that are helpful for fetal OP positions may reduce back pain. Using the birthing ball can relax and support the woman in some positions. Warmth to her back can reduce back pain. However, the mother’s skin sensation of warm applications may be reduced by a regional block, and they should be avoided in those areas. Warm applications to areas unaffected by the block may be comforting. Maintain IV fluids at the rate ordered to provide fluid and electrolytes, and occasionally glucose. Assess intake and output to identify dehydration, which may accompany prolonged labor and may cause maternal fever, often preceded by fetal tachycardia. If there is no contraindication, provide juice, lollipops, Popsicles, or other liquids to moisten the woman’s mouth and replenish her energy.
Promoting Coping Skills
When medical therapy or position changes are used to enhance labor, explain their purpose and expected benefits. Encourage the woman to visualize her baby passing downward smoothly through her pelvis as a result of her efforts. Provide her with mental images that allow her to “see” herself giving birth.
Generous praise and encouragement of the woman’s use of skills, such as breathing techniques, motivate her to continue them even when she is discouraged. As with any laboring woman, tell her when she is making progress. Tell her that FHRs and patterns are reassuring if this is true. Knowing that her efforts are having the desired results and that her fetus is doing well gives the woman courage to continue.
Evaluation
Premature Rupture of the Membranes
Rupture of the amniotic sac before the onset of true labor, regardless of length of gestation, is called premature rupture of the membranes (PROM). A related term, preterm premature rupture of the membranes (often abbreviated PPROM or pPROM), describes membranes ruptured earlier than the end of the 37th week of gestation, with or without contractions. PROM may be a normal occurrence that precedes term birth at 38 weeks or later, even if labor induction is needed to initiate labor. However, PPROM is often associated with preterm labor (PTL), with the greatest risks from preterm birth occurring before completing 34 weeks of gestation (ACOG, 2007b; Mercer, 2009b; Svigos, Dodd, & Robinson, 2011a). However, brief delays of an inevitable preterm birth from PPROM may enable interventions to reduce these risks.
Etiology
Several conditions have been found when a woman’s membranes rupture early, but the exact cause is not always identified. Most cases of PPROM have no identifiable cause. Possible causes are (ACOG, 2007b; Mercer, 2009b):
Complications
Both mother and newborn are at risk for infection during the intrapartum and postpartum periods. Chorioamnionitis, or intraamniotic infection, can be both a cause and a result of PPROM. The mother is at higher risk for postpartum infection. The newborn is at greater risk for sepsis after birth, with the most immature preterm infants having the greatest risk for the systemic infection.
Chorioamnionitis, characterized by maternal fever and uterine tenderness, is most likely to precede preterm birth in the infant born before 34 weeks of gestation. Preterm infants with the lowest maturity, such as 23 weeks of gestation, have a greater risk for infection than a preterm infant who is even a few weeks more mature. The exact time at which infection occurs cannot be predicted for either term or preterm infants.
Membranes ruptured well before term may form a seal, stopping the fluid leak and allowing the amniotic fluid cushion to become reestablished. However, membranes may continue to leak, prolonging the loss of the amniotic fluid cushion (oligohydramnios) for the fetus. Umbilical cord compression, reduced lung volume, and deformities resulting from compression may occur, particularly in the fetus impacted at the earliest gestation.
Therapeutic Management
Management of PROM depends on the gestation and whether there is evidence of infection or other fetal or maternal compromise. If infection is present, further management also depends on the type of infection. For a woman at term, PROM may herald the imminent onset of true labor. Usually, the cervix is soft with some dilation and effacement, and the fetal head is at or near zero station. Labor induction or cesarean birth may be reasonable if the fetus is 34 to 36 weeks of gestation or more because the negative impact of an active infection may be greater than a late preterm birth. Studies to determine fetal lung maturity are often done.
If the pregnancy is earlier than 34 weeks of gestation, therapeutic management is more complex. The risk for infection or preterm birth is weighed against the hazards of actively promoting birth, whether vaginally or by cesarean. Accurate gestational age and evaluation of fetal lung maturity are important and may not be well defined in women with little or no prenatal care.
Determining True Membrane Rupture
The first step is to determine whether the membranes are truly ruptured. Urinary incontinence, increased vaginal discharge, or loss of the mucous plug can cause a woman to believe her membranes have ruptured when they have not. A vaginal examination is avoided if the gestation is preterm and there is no evidence of labor. Instead, the physician or nurse-midwife performs a sterile speculum examination to look for a pool of fluid near the cervix and to estimate cervical dilation and effacement. A pH test or fern test (see Chapter 16) may verify that the vaginal fluid is amniotic fluid, although blood, semen, or vaginal infections may alter tests. Tests to assess fetal lung maturity and identify infection may be done. A transvaginal ultrasound may be done to measure cervical length to identify the short cervix (≤25 mm) that is more likely to continue effacement and dilation.
Gestation Near Term
If labor does not begin spontaneously, the woman’s pregnancy is at or near term, and her cervix is favorable, labor may be induced (see Chapter 19). If the cervix is not favorable and no infection is present, induction may be delayed 24 hours or longer to allow cervical softening and administration of drugs to combat infection associated with early membrane rupture. If induction is unsuccessful or if infection or other complications develop, a cesarean birth is most common. The nurse should remember, however, that cesarean birth also increases the risk for any mother’s infection after birth.
Preterm Gestation
If the fetus is less than 34 weeks of gestation, the physician weighs the risks of infection against the infant’s risk for complications of prematurity. Cesarean birth is more common if delivery at the earlier gestation is needed. The physician considers factors such as gestational age, amount of amniotic fluid remaining, and fetal lung maturity in addition to possible infection of mother and infant.
Maternal Antibiotics
Maternal antibiotics may stop the infection that caused or will occur with the rupture, thus delaying the onset of labor and allowing the fetus to mature. Drugs to stop infection if early membrane rupture occurs may include ampicillin, erythromycin, amoxicillin, and azithromycin. The current recommendations are for 48 hours of IV antibiotics followed by 5 days of oral antibiotics to treat or prevent infections associated with PPROM. GBS is also treated if indicated (see Chapter 26) (ACOG, 2007b).
Nursing Considerations
The woman may remain hospitalized until birth, or she may return home after a few days of hospital observation and usually 48 hours of IV antibiotics. If she is hospitalized, the nurse observes for signs of infection. Preparation for home management includes teaching the woman to:
Preterm Labor
Preterm labor (PTL) begins after the 20th week but before the end of the 37th week of pregnancy. The physical risks to the mother are no greater than labor at term unless complications, such as infection, hemorrhage, or the need for a cesarean delivery, also exist. PTL, however, may result in the birth of an infant who is ill equipped for extrauterine life, particularly if earlier than 32 weeks of gestation. Preterm births have increased from 10.6% of births in 1990, to 12.2% of births in 2009—a dramatic increase over only 19 years. One in eight babies are now born prematurely. Almost 60% of infant deaths in 2007 were to the 2% of infants born at less than 32 weeks of gestation. Infant mortality for late preterm infants (34 through 36 weeks of gestation) was three times the mortality for term infants (37 to 41 weeks of gestation) in 2007 (Cunningham et al., 2010; Hamilton, Martin, & Ventura, 2010; Iams, Romero, & Creasy, 2009; Mathews & MacDorman, 2011; Svigos, Dodd, & Robinson, 2011a).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree