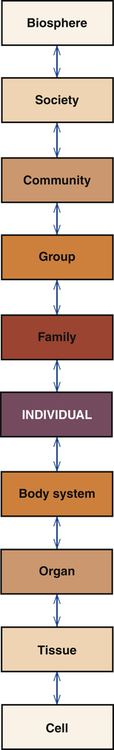
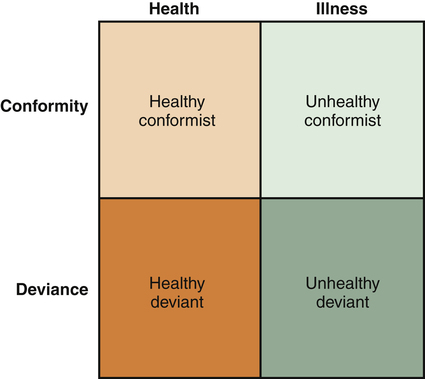
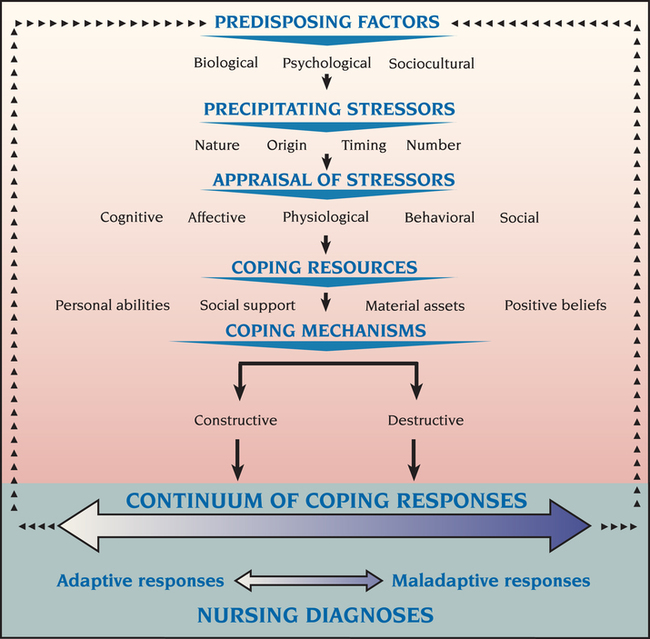
1. Discuss the theoretical assumptions underlying the Stuart Stress Adaptation Model of psychiatric nursing care. 2. Describe dimensions of mental health and mental illness in the United States. 3. Analyze the biopsychosocial components of the Stuart Stress Adaptation Model of psychiatric nursing care. 4. Compare coping responses, nursing diagnoses, health problems, and medical diagnoses. 5. Evaluate nursing activities appropriate to the various stages of psychiatric treatment. The first assumption of the Stuart Stress Adaptation Model is that nature is ordered as a social hierarchy from the simplest unit to the most complex (Figure 3-1). Each level of this hierarchy is an organized whole. Each level also is a part of all of the other levels, so nothing exists in isolation. Thus the individual is a part of the family, group, community, society, and the larger biosphere. Material and information flow across levels, and each level is influenced by all the others. The most basic level of nursing intervention is the individual. However, in working with the individual, the nurse also must consider how the individual relates to the whole. The second assumption of the model is that nursing care is provided within a biological, psychological, sociocultural, legal, ethical, policy and advocacy context. Each of these aspects of care is described in detail in Chapters 5 through 9. The nurse must understand each of them in order to provide competent, holistic psychiatric nursing care. The theoretical basis for psychiatric nursing practice is derived from nursing science as well as from the behavioral, social, and biological sciences. The range of theories used by psychiatric nurses includes nursing, developmental psychology, neurobiology, pharmacology, psychopathology, learning, sociocultural, cognitive, behavioral, economic, organizational, political, legal, ethical, interpersonal, group, family, and milieu. • The health/illness continuum comes from a medical world view. • The adaptation/maladaptation continuum comes from a nursing world view. This means that a person with a medically diagnosed illness may be adapting well to it. An example is the adaptive coping responses used by some people who have chronic physical or psychiatric illnesses. In contrast, a person without a medically diagnosed illness may have many maladaptive coping responses. This can be seen in the adolescent whose problematic behaviors reflect poor coping responses to the many issues that must be resolved during adolescence. These two continuums thus reflect the complementary nature of the nursing and medical models of practice. The fifth assumption of the Stuart Stress Adaptation Model is that it is based on the use of the nursing process and the standards of care and professional performance for psychiatric nurses (Chapter 11). Psychiatric nursing care is provided through assessment, diagnosis, outcome identification, planning, implementation, and evaluation. Each step of the process is important, and the nurse assumes full responsibility for all nursing actions implemented and the enactment of a professional nursing role. The assumptions of the Stuart Stress Adaptation Model are summarized in Box 3-1. The standards of mental health are less clear than those of mental illness. It is dangerous to assume that an unusual lifestyle is a sign of illness or abnormality. This can be avoided if one thinks of health/illness and conformity/deviance as separate concepts. Combining them creates four patterns: the healthy conformist, the healthy deviant, the unhealthy conformist, and the unhealthy deviant (Figure 3-2). Psychiatric nurses must carefully consider the meaning of an individual’s behavior and its context, because it reflects an adaptation to issues in the individual’s life and one’s social and cultural environment. The following six criteria are indicators of mental health: Growth, self-actualization and resilience mean that the individual seeks new experiences to more fully explore aspects of oneself. Maslow (1958) and Rogers (1961) developed theories on the realization of the human potential. Maslow describes the concept of self-actualization, and Rogers emphasizes the fully functioning person. Both theories focus on the entire range of human adjustment. They describe a self as always seeking new growth, development, and challenges. These theories focus on the total person and whether the person has the following characteristics: • Is in touch with one’s self and able to use the available resources • Has access to personal feelings and can integrate them with thoughts and behaviors • Can interact freely and openly with the environment • Can share with other people and grow from such experiences This criterion includes the concept of resilience, which is the ability to achieve, retain, or regain a level of physical or emotional health after a tragedy, trauma, adversity or significant stressor. It is the idea that some people “bounce back” after a problem, and proposes that humans must weather periods of stress and change throughout life. Successfully weathering each period of disruption and reintegration leaves the person better able to deal with the next life change (Wagnild and Collins, 2009; Resnick and Inguito, 2011). Mental disorders are a major contributor to the burden of illness in the United States (Kessler et al, 2005a,b). • Nearly 50% of all people ages 18 years and older have had a psychiatric or substance abuse disorder in their lifetimes. • Half of all these lifetime cases start by age 14 and three-fourths start by age 24. The seriousness and persistence of some disorders cause great strain on affected individuals, their families, communities, and the larger health care system. In addition, there is a substantial increased risk of premature death from natural and unnatural causes for people with common mental disorders (Druss and Bornemann, 2010). The Substance Abuse and Mental Health Services Administration (SAMHSA) has thus identified four important messages: • Behavioral health is an essential part of all health. • People recover from mental health and substance use disorders. Box 3-2 presents other key facts about mental illness (SAMHSA, 2011). In 1996 the Global Burden of Disease Study examined the disabling outcomes of 107 diseases around the world. Of the 15 specific leading causes of disability in developed countries, five are mental health problems: (1) major depressive disorder, (2) alcohol use, (3) schizophrenia, (4) self-inflicted injuries, and (5) bipolar disorder (Murray and Lopez, 1996). Depressive disorders as a single diagnostic category were the leading cause of disability worldwide. Further, by the year 2020, mental disorders are projected to increase, and major depression is predicted to become the second leading cause in disease burden worldwide. The Stuart Stress Adaptation Model of psychiatric nursing care views human behavior from a holistic perspective that integrates biological, psychological, and sociocultural aspects of care. For instance, a man who has had a myocardial infarction also may be severely depressed because he fears he will lose his ability to work and to satisfy his wife sexually. He also may have a family history of depression. Likewise, patients who seek treatment for major depression also may have gastric ulcers that are exacerbated by their depression. The holistic nature of psychiatric nursing practice examines all aspects of the individual, family, community and the environment. The specific biopsychosocial components of the Stuart Stress Adaptation Model are shown in Figure 3-3. • Biological predisposing risk factors include genetic background, nutritional status, biological sensitivities, general health, and exposure to toxins. • Psychological predisposing risk factors include intelligence, verbal skills, morale, personality, past experiences, self-concept and motivation, psychological defenses, and locus of control, or a sense of control over one’s own fate. • Sociocultural predisposing risk factors include age, gender, education, income, occupation, social position, cultural background, religious upbringing and beliefs, political affiliation, socialization experiences, and level of social integration or relatedness.
The Stuart Stress Adaptation Model of Psychiatric Nursing Care
Theoretical Assumptions
Describing Mental Health and Illness
Defining Mental Health
Criteria of Mental Health.
Defining Mental Illness
Biopsychosocial Components
Predisposing Factors
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


The Stuart Stress Adaptation Model of Psychiatric Nursing Care
Get Clinical Tree app for offline access