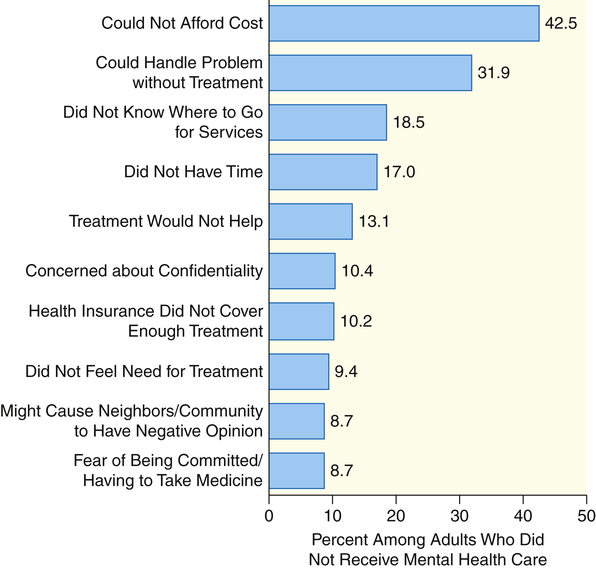
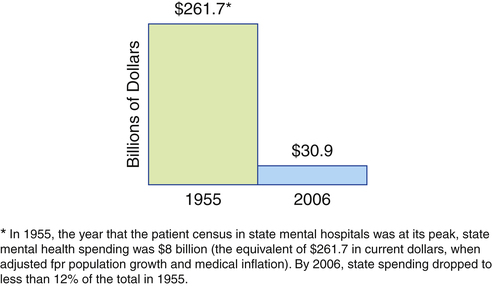
I do not want to talk about what you understand about this world. I want to know what you will do about it. I do not want to know what you hope. I want to know what you will work for. I do not want your sympathy for the needs of humanity. 1. Describe the need for mental health care from global and national perspectives. 2. Examine policy and legislation related to mental health and substance use services including access to care, parity, and protection of patients’ rights. 3. Evaluate areas for mental health advocacy. 4. Implement advocacy strategies to improve mental health care. Mental illnesses are significant worldwide health problems. The World Health Organization’s (WHO) global burden of disease study revealed that mental disorders are the second most disabling category of illnesses around the world (Murray & Lopez, 1996). The study compared a range of physical and mental disorders to determine their contribution to the overall burden of disease. The data showed the following: • Depression was the number one psychiatric cause of disability in the world. • Four other psychiatric disorders were among the top 10: alcohol abuse, bipolar disorder, schizophrenia, and obsessive-compulsive disorder. • Depression ranked second in the United States as a cause of disability. • Depression was projected to rank second in the world as a cause of disability by 2020. In 2009 there were an estimated 20%, or 45 million, adults ages 18 or older in the United States with any mental illness in the past year. The percentage having serious mental illness in the past year was about 5%, or 11 million adults (Substance Abuse and Mental Health Services Administration [SAMHSA], 2010). Unfortunately, many of these persons never receive treatment. Barriers to receiving mental health care are presented in Figure 9-1. For individuals with mental illness who received treatment, 20% quit before completing treatment recommendations (Olfson et al, 2009). Yet untreated and mistreated mental illness costs American business, government, and taxpayers an estimated $113 billion each year. Four important reports released in the United States are having an impact on the delivery of mental health care. The most recent is Healthy People 2020, which identifies a list of leading health indicators that reflect the major public health concerns in the United States (U.S. Department of Health and Human Services [USDHHS], 2010). Those related to mental health include tobacco use, substance abuse, responsible sexual behavior, mental health, injury and violence, and access to health care. For each of the leading health indicators, specific objectives derived from Healthy People 2020 have been identified. The objectives related to mental health are presented in Box 9-1, providing a snapshot of the mental health issues in the United States. The second national report is Improving the Quality of Health Care for Mental and Substance-Use Conditions (Institute of Medicine [IOM], 2006). This report describes a multifaceted and comprehensive strategy for ensuring access, improving quality, and expanding mental health and substance abuse treatment services. The third was the report from the New Freedom Commission on Mental Health (NFCMH), Achieving the Promise: Transforming Mental Health Care in America (NFCMH, 2003). The commission was formed to address the problems in the mental health service delivery system that allow Americans to fall through the system’s “cracks.” The commission found that the current system is unintentionally focused on managing disabilities associated with mental illness rather than promoting recovery. This is because of fragmentation, gaps in care, and uneven quality in mental health services. The commission thus recommended a focus on promoting recovery and building resilience—the ability to withstand stresses and life challenges (Chapters 12 and 14). Six goals and a series of recommendations for federal agencies, states, communities, and providers nationwide were identified. These are listed in Box 9-2. The fourth report, published in 1999, was the first issued by a U.S. surgeon general on the topic of mental health and mental illness, Mental Health: A Report of the Surgeon General (USDHHS, 1999). This landmark document concluded the following: • Mental health is fundamental to health. • Mental disorders are real health conditions that have an immense impact on individuals and families. • The efficacy of mental health treatments is well documented. • A range of treatments exists for most mental disorders. • People should seek help if they have a mental health problem or think that they have symptoms of a mental disorder. Currently, two thirds of the people who seek mental health care are treated by primary care providers (Chapter 34). However, many who need care do not receive it, from either a primary care or a specialty provider. The major reason for not receiving treatment is cost. Unmet needs for treatment are greatest in traditionally underserved groups, including the elderly, racial and ethnic minorities, those with low incomes, those without insurance, and residents of rural areas (Giled and Frank, 2009; Garfield et al, 2011). Some access problems apply to the entire health care system, such as the lack of providers in rural areas and the absence of care for people who lack health insurance. Other problems are unique to mental health care. These include the stigma associated with seeking care, the lack of knowledge about how to find the right clinician for a highly personal problem, and the shortage of general medical settings to adequately respond to mental health and substance use disorders. A significant barrier to access is the major decline in the states’ funding of mental health services (Figure 9-2). Persons with serious mental illness are more likely to be uninsured, and even insured persons often receive no treatment or inadequate mental health treatment because of policies and societal values that are discriminatory (Khaykin et al, 2010; Compton et al, 2011). Some policies and laws have been enacted that attempt to address these issues. • Mandated coverage for mental health care means that if an employer offers health insurance for employees, both physical illnesses and mental illnesses must be covered. However, these levels of coverage were not equal; that is, coverage for mental health care was extremely limited compared to the coverage for physical illness, hence the need for mental health parity policies. • Mental health parity policies help ensure that insurance coverage for mental illnesses is equal to that for physical illnesses. Mental health advocates who fought for appropriate and fair mental health treatment have long pursued mental health parity. It was only recently, in 2010, that this has become a reality.
Policy and Advocacy in Mental Health Care
A Compelling Need
The Global View
The National View
Policy and Legislation
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access