4 The patient journey within medical placements
Introduction
It is important to think about your practice learning pathways and how these can truly reflect the journey your patients are taking. Health care is changing rapidly and it is essential that you are knowledgeable and competent at the point of registration to care for a patient wherever they are within their healthcare journey. Practice learning opportunities should, where possible, reflect local and national care delivery approaches including care pathways (Nursing and Midwifery Council (NMC) 2010a). This might mean that while you are on placement you could move between the community, social care, voluntary sector, non-NHS sector and acute hospital to follow a patient though their journey. Or it could be for you to gain an understanding of the healthcare journey that some of your patients might experience.
The broad nature of medical learning pathways and their journey through the healthcare system
Stroke unit
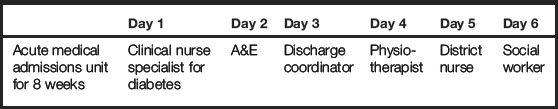
A patient who has suffered a stroke will come into contact with a number of the multidisciplinary team. The patient will spend some time in the acute phase of their condition and then some time rehabilitating. Personnel involved in their care might include a psychologist, speech and language therapist, physiotherapist, occupational therapist and doctors. There may also be voluntary groups for carers and patients that you could explore and spend time with. Table 4.1 provides an example of a typical week in the life of a patient following a stroke that you might experience on an 8-week placement.
Table 4.1 Example of an 8-week placement: the patient experience and interprofessional working (negotiated with the mentor)
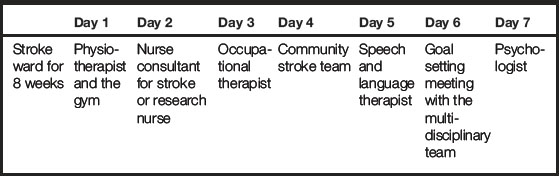
The learning opportunities within this 8-week placement are vast and really allow you to gain knowledge and understanding of the patient journey and experience. The bespoke 1-day placements with the the psychologist, etc., may already be arranged for you by your mentor or there may be an expectation that you, as an adult learner, will arrange these bespoke days. However, you can discuss this with your mentor during your initial meeting. To meet your learning outcomes in such a placement, you would need to negotiate and discuss with your mentor how you could evidence what you have learnt within all of your experiences, and when you would meet up for your midpoint and endpoint meetings to discuss your learning. The teams work closely together and there will be space within your record of achievement/practice curriculum documentation to allow for comments from other nurses and healthcare professionals to document what you have achieved and experienced within your 1-day and 8-week placements (NMC 2010a).
Acute medical admissions unit
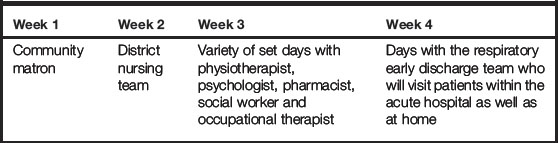
You could also be placed on an acute medical admissions unit which would look very different from a stroke unit, however the same principles might apply. Your patient may come in from the accident and emergency (A&E) department and you may find it helpful to spend some time there to understand how the department works and what your patient might have experienced. Your patients may be transferred to other departments and it will be helpful to discuss this with your mentor to determine where else you might need to spend some of your placement time. Some patients may be discharged home with a care package and others may go to a general medical ward or high-dependency unit. Other members of the multidisciplinary team will be involved and, again, you can find this out from your mentor. Table 4.2 gives an example of acute medical admissions unit placement opportunities.
Virtual ward
Virtual wards were discussed in Chapter 2 but here is a brief outline. Virtual wards provide support in the community for people with complex medical and social needs. People are cared for by a team of staff as they would be in hospital, however there is no physical building. The virtual ward aims to provide multidisciplinary case management, to prevent admission to secondary care (acute hospital wards) and to enhance the communication for all those involved in the care. The patient is at the centre of the care. There are different models for virtual wards with some being nurse led and others GP led. The patients that you will care for during your virtual ward placement will still require nursing care and interprofessional team working, which will be coordinated by a community matron. There will be liaison with the acute hospital and some teams will work across the acute and community journey of the patients.
For a 4-week learning pathway on a virtual ward, the weeks might be set out as in Table 4.3. For every practice learning pathway you will be provided with a mentor and, as can be seen in Table 4.3, there could be a variety of nurses who might be assigned as your mentor. It could be the community matron, the district nurse or one of the more specialist nurses.
During this placement your mentor can directly or indirectly supervise you (NMC 2008a) and how this will occur will be negotiated during your inital meeting. Within the virtual ward, teams of healthcare professionals will work closely together and a team approach may be taken to ensure that your mentor has all the evidence required to assess you. You should ensure, when you are working with another healthcare professional, that what you have experienced and achieved are documented. Other members of the healthcare team that you spend time with should have been suitably prepared to ensure they are familiar with your learning needs and their role in contributing to your assessment (NMC 2010a).
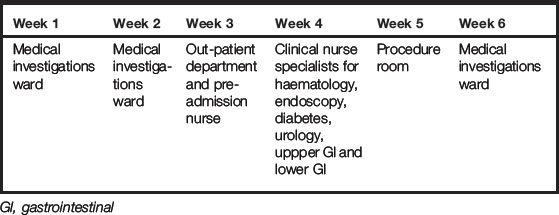
6-week medical investigations ward placement
As a student, after discussion with other students, you may consider that you feel disappointed about not going somewhere more acute and may feel disadvantaged. Do not worry – medical day care is a fabulous experience and you will be able to follow the patient journey from pre-admission to discharge. You will be able to experience the care of the patient pre-procedure, peri-procedure and post-procedure for a number of conditions. Medical day care is often multifaceted with several specialties running alongside each other. It may also be part of the journey for patients who are admitted to acute medical admissions, high-dependency and general wards. You may have the opportunity to follow them back to their ward base and be able to understand their journey. Other patients will be admitted from nursing homes, intermediate care and out-patient departments. Table 4.4 shows an example of how a 6-week placement could look in medical day care.
12-week placement on a general medical ward
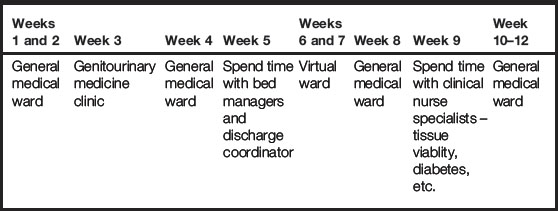
Of course, placements can be longer, and a 12–14 week placement is not uncommon within any year of your programme regardless of your field of practice. Longer placements can be really useful in allowing your learning to become much deeper and sustained. Table 4.5 shows an example of a 12-week placement. In this example, you could spend 6 weeks on a general medical ward and then spend 1 or 2 weeks within the specialist clinic environment linked to that ward or spend time with a variety of clincial nurse specialists that your patient may encounter during their journey.
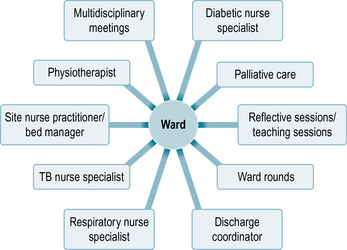
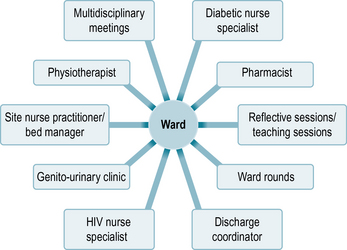
Some mentors may use the hub and spoke model of placing students, where the placement is considered the hub and all the spokes relate to who the patient might come into contact with and where during their stay in your placement. The spokes also represent learning opportunities and possible experiences that you as a student could benefit from. The examples given in Figures 4.1 and 4.2 look at some hub and spoke models for respiratory and HIV wards.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree