10 Medicines management
• To provide an overview of policy and procedure associated with medicines management
• To provide an Introduction to the commonest medicines used for patients in medical placements
• To consider how to assess the effect of the medicines administered
• To identify opportunities to develop knowledge and skills in medicines management throughout the patient journey
Introduction
Regardless of your field of nursing or year of training, you will have learning outcomes that focus on medicines management because it is one of the Nursing and Midwifery Council (NMC) Essential Skills Clusters (NMC 2010) from year 1 to entry to the register. Box 10.1 provides some examples of the Essential Skills Cluster – Medicines Management (NMC 2010).
Box 10.1 Examples of the Essential Skills Cluster – Medicines Management
By the end of the third year, many skills are identified such as the following:
 Drug pathways and how they act.
Drug pathways and how they act.
 Related anatomy and physiology.
Related anatomy and physiology.
 Effects of medicines and other treatment options.
Effects of medicines and other treatment options.
(NMC 2010)
Read the NMC Standards for Medicines Management (2008a), your university and placement guidelines, and then discuss your role in medicines management with your mentor.
An example of the guidelines you might read about are:
Nurse prescribing and patient group directives
Within your medical placements you may be exposed to a range of nurses who have completed an advanced course in nurse prescribing. Only those who have undergone appropriate training and are registered with the NMC as an independent prescriber can prescribe (NMC 2006). It must also be judged that it is part of the nurse’s role. Some clinical nurse specialists, advanced nurse practitioners, practice nurses, district nurses, health visitors and community matrons will have completed this course and will have undergone intensive supervision and academic assessment to meet the competencies required (Kaufman 2010).
Self-administration
In some of your medical placements, patients may be self-administering their medication and there should be a policy within the organisation that supports this practice. Nurses must assess that the patient is willing to do this, has the knowledge and is not forgetful or confused before self-administering their medication. It can work very effectively for patients as they do not need to wait for a nurse to administer their medication and they are able to have control over this aspect of their care. Within the essential skills clusters, there is an expectation that student nurses will ‘involve people and carers in administration and self-administration of medicines’ (NMC 2010) and from your second year this will be one of your learning outcomes under the supervision and guidance of your mentor.
• Blister packs: the medication is packaged with the days of the week highlighted.
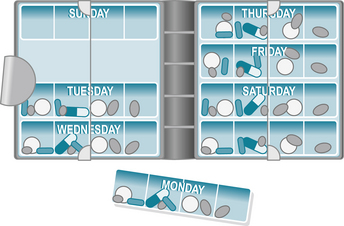
• Dosette boxes: the medication will be placed in a box with separate compartments for days and times by a nurse to ensure that the patient does not get muddled about which medication to take and when. This is very helpful when a patient has multiple medications to take every day (Fig. 10.1).
Covert administration
Covert administration of medicines means administering medicines to your patient without their knowledge, for example disguising it in food or drink. This is not considered good practice (NMC 2008a). If your patient is refusing their medicines, it is important that you first establish why they do not want to take them. Often it will be because they don’t know what they are or why they need to take them. Spending some time explaining the medicines and reassuring your patient may be all that is needed for your patient to agree to take their prescribed medicines.
It may be that your patient does not understand the importance of the medicines and the potential side effects of not taking them. In this case, the team looking after the patient will need to determine if the patient has capacity to decide whether to take the medicines (see Ch. 6 for a discussion on capacity). Within the Essential Skills Clusters (NMC 2010) there is an expectation that ‘people can trust the newly registered graduate nurse to work within the legal and ethical frameworks that underpin safe and effective medicines management’.
Medicines management for controlled drugs
Since the fourth report of The Shipman Inquiry (2004) there has been tighter legislation in relation to controlled drugs, and nurses need to familiarise themselves with the latest NMC, Department of Health and local trust and university policies. As a student, you will be placed in a variety of placements – community, independent sector and acute sector trusts – and will need to make sure that you are aware of the placement policies regarding controlled drugs. The NMC (2008a) emphasises that student nurses must be involved in the administration of all medicines when they are deemed competent by a registrant and also feel confident and competent themselves. One of the essential skill outcomes states that ‘people can trust the newly registered graduate nurse to safely order, receive, store and dispose of medicines (including controlled drugs) in any setting’ (NMC 2010).
The national guidance for drugs considered to be controlled drugs can be found here:
Quiz: management of controlled drugs
Here is a quiz to help you with the above activity.
10.1. Are student nurses allowed to give any medication without supervision?
10.2. Which of these policies do student nurses need to read and understand prior to taking part in drug administration?
10.3. A staff nurse checks paracetamol with you in the clinical room and then asks you to take the medication to Mrs Smith in bed 8. Would you say yes or no? Explain your answer.
10.4. Mrs Patel is confused and refusing her antibiotic which she really needs. The staff nurse crushes the tablet and disguises it in a spoon of porridge and asks you to give this to the patient. Would you agree to this? Explain your answer.
10.5. Your patient requires a subcutaneous injection of insulin which the staff nurse allows you to draw up under his/her supervision. The staff nurse then takes you to the patient and allows you to administer the injection. Would you agree to do this? Explain your answer.
10.6. You have just undertaken a blood glucose measurement which is 10 mmol. The patient is on an insulin infusion which is currently running at 1 mL/hour. The prescription states that the infusion should run at 2 mL/hour if the blood glucose is 10 mmol. You inform the staff nurse and she tells you to increase the rate on the pump. Would you agree to do this? Explain your answer.
10.7. What is a controlled drug?
10.8. Who would need to be present when preparing and administering a controlled drug?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree