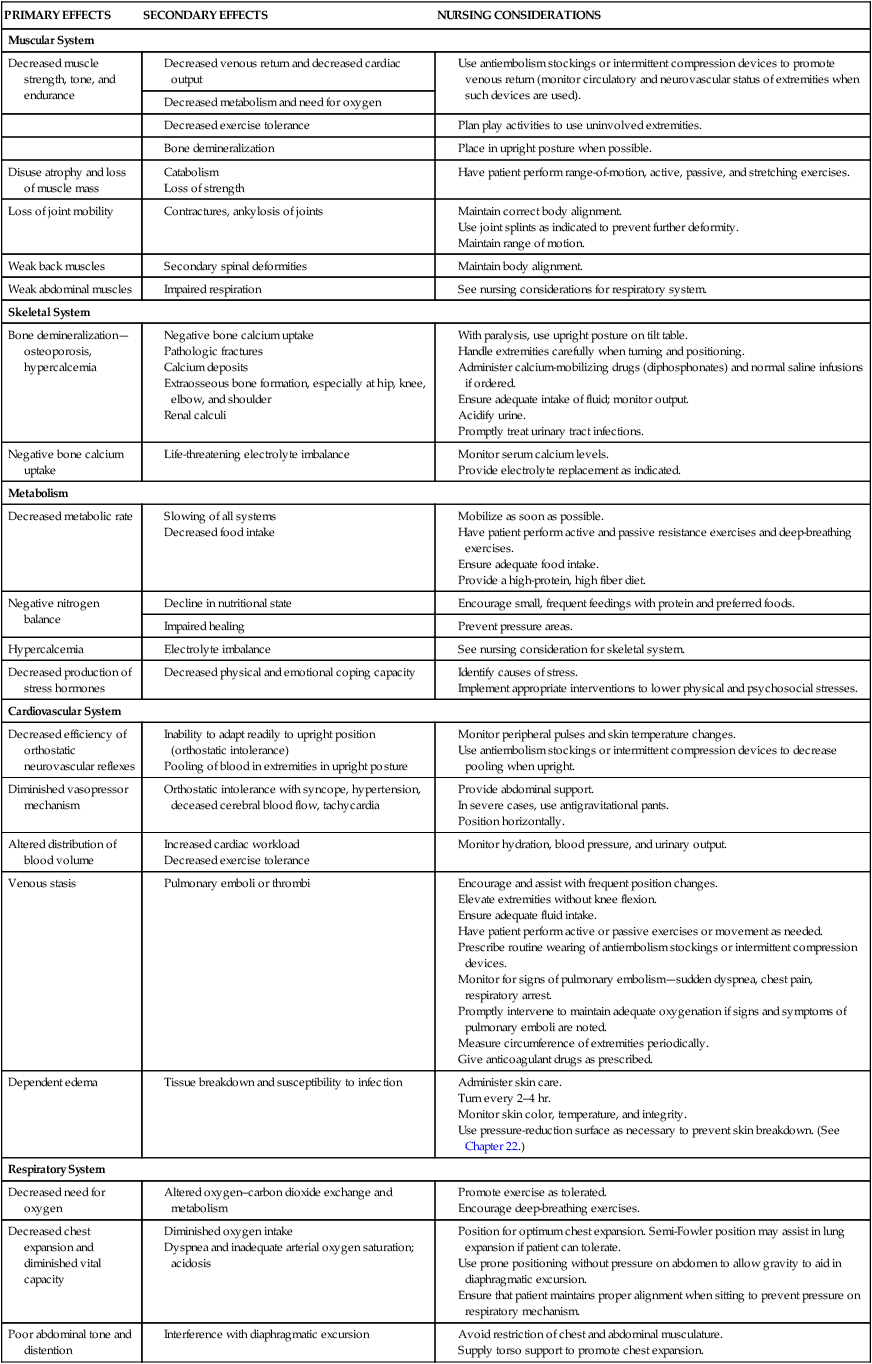
On completion of this chapter the reader will be able to: • Outline a plan of care for a child immobilized with an injury or a degenerative disease. • Develop a teaching plan for the parents of a child in a cast. • Explain the functions of the various types of traction. • Devise a nursing care plan for a child in traction. • Differentiate among the various congenital skeletal defects. • Design a teaching plan for the parents of a child with a congenital skeletal deformity. • Describe the therapies and nursing care of a child with idiopathic scoliosis. • Outline a care plan for a child with osteomyelitis. • Differentiate between osteosarcoma and Ewing sarcoma. • Describe the nursing care of a child with juvenile idiopathic arthritis. • Demonstrate an understanding of the management of a child with systemic lupus erythematosus. http://evolve.elsevier.com/wong/essentials Animations—Bone Fractures; Osteomyelitis; Spine Structure Case Studies—Developmental Dysplasia of the Hip; Fractures; Legg-Calvé-Perthes Disease; Osteomyelitis; Scoliosis Nursing Care Plans—The Child with a Fracture; The Child with Arthritis (Juvenile Idiopathic Arthritis) The major effects of immobilization are outlined briefly in Table 31-1 and are related directly or indirectly to decreased muscle activity, which produces numerous primary changes in the musculoskeletal system with secondary alterations in the cardiovascular, respiratory, skeletal, metabolic, and renal systems. The musculoskeletal changes that occur during disuse are a result of alterations in the effect of gravity and stress on the muscles, joints, and bones. Muscle disuse leads to tissue breakdown and loss of muscle mass (atrophy). Muscle atrophy causes decreased strength and endurance, which may take weeks or months to restore. TABLE 31-1 SUMMARY OF PHYSICAL EFFECTS OF IMMOBILIZATION WITH NURSING INTERVENTIONS* Encourage and assist with frequent position changes. Elevate extremities without knee flexion. Have patient perform active or passive exercises or movement as needed. Prescribe routine wearing of antiembolism stockings or intermittent compression devices. Monitor for signs of pulmonary embolism—sudden dyspnea, chest pain, respiratory arrest. Promptly intervene to maintain adequate oxygenation if signs and symptoms of pulmonary emboli are noted. Measure circumference of extremities periodically. Position for optimum chest expansion. Semi-Fowler position may assist in lung expansion if patient can tolerate. Use prone positioning without pressure on abdomen to allow gravity to aid in diaphragmatic excursion. Ensure that patient maintains proper alignment when sitting to prevent pressure on respiratory mechanism. *Individualize care according to child’s needs; interventions may vary in different institutions. The major musculoskeletal consequences of immobilization are: • Significant decrease in muscle size, strength, and endurance • Bone demineralization leading to osteoporosis Children may react to immobility by active protest, anger, and aggressive behavior, or they may become quiet, passive, and submissive. They may believe the immobilization is a justified punishment for misbehavior. Children should be allowed to display their anger, but it should be within the limits of safety to their self-esteem and not damaging to the integrity of others (see Providing Opportunities for Play and Expressive Activities, Chapter 21). When children are unable to express anger, aggression is often displayed inappropriately through regressive behavior and outbursts of crying or temper tantrums. Even brief periods of immobilization may disrupt family function, and catastrophic illness or disability may severely tax a family’s resources and coping abilities. The family’s needs often must be met by the services of a multidisciplinary team, and nurses play a key role in anticipating the services they will need and in coordinating conferences to plan care. In preparation for discharge, home management is frequently planned before discharge, including special considerations for addressing cultural, economic, physical, and psychological needs. A child with a severe disability is very dependent, and caregivers need respite to revitalize themselves. Individual and group counseling is beneficial for solving problems in advance and provides an emotional support system. Parent groups are also helpful and often allow nonthreatening social contact. The families of children with permanent disabilities need long-term resources because some of the most difficult problems arise as they try to sustain high-quality care for many years (see Chapter 20). Children who require prolonged total immobility and are unable to move themselves in bed should be placed on a pressure-reduction mattress to prevent skin breakdown. Frequent position changes also help prevent dependent edema and stimulate circulation, respiratory function, gastrointestinal motility, and neurologic sensation. Children at greater risk for skin breakdown include those with prolonged immobilization; mechanical ventilation; orthotic and prosthetic devices, including wheelchairs; and casts. Additional risk factors include poor nutrition, friction (from bed linen with traction), and moist skin (from urine or perspiration). Nursing care of children at risk includes strategies for preventing skin breakdown when such conditions are present. The Braden Q Scale is a reliable, objective tool that may be used in the assessment for pressure ulcer development in children who are acutely ill or who are at risk for skin breakdown from neurologic conditions and immobilization (Noonan, Quigley, and Curley, 2011). Whenever possible, transporting the child outside the confines of the room increases environmental stimuli and allows social contact with others. Specially designed wheelchairs for increased mobility and independence are available. While hospitalized, children benefit from same-age visitors, computers, books, interactive video games, and other items brought from their own room at home, all of which help them to function in a more normal way. While hospitalized, they also benefit from frequent visitors, accessibility of clocks and calendars, and a program of diversional therapy to help them function more normally. A child life specialist should be consulted for recreational planning. An activity center or slanting tray can be helpful for the child with limited mobility to use for drawing, coloring, writing, and playing with small toys such as trucks and cars. Children are able to express frustration, displeasure, and anger through play activities (see Chapter 21), which is helpful in the child’s recovery. Hospitalized children should be allowed to wear their own clothes (street clothes, especially for preadolescent and adolescent girls) and resume school and preinjury activities. A parent or siblings should be allowed to stay overnight and room in with the hospitalized child to prevent the effects of family disruption from hospitalization. All efforts should be made to minimize family disruption resulting from the hospitalization. Although most of the suggestions discussed relate to hospital care, the same consultations (physical therapist, occupational therapist, child life specialist, speech therapist) and environment may be considered in the home as well to help the child and family achieve independence and normalization (see Chapter 20).
The Child with Musculoskeletal or Articular Dysfunction
The Immobilized Child
Immobilization
Physiologic Effects of Immobilization
PRIMARY EFFECTS
SECONDARY EFFECTS
NURSING CONSIDERATIONS
Muscular System
Decreased muscle strength, tone, and endurance
Disuse atrophy and loss of muscle mass
Loss of joint mobility
Weak back muscles
Weak abdominal muscles
Skeletal System
Bone demineralization—osteoporosis, hypercalcemia
Negative bone calcium uptake
Metabolism
Decreased metabolic rate
Negative nitrogen balance
Hypercalcemia
Decreased production of stress hormones
Cardiovascular System
Decreased efficiency of orthostatic neurovascular reflexes
Diminished vasopressor mechanism
Altered distribution of blood volume
Venous stasis
Dependent edema
Respiratory System
Decreased need for oxygen
Decreased chest expansion and diminished vital capacity
Poor abdominal tone and distention
Mechanical or biochemical secretion retention
Loss of respiratory muscle strength
Gastrointestinal System
Distention caused by poor abdominal muscle tone
No specific primary effect
Urinary System
Alteration of gravitational force
Impaired ureteral peristalsis
Integumentary System
Altered tissue integrity
Psychologic Effects of Immobilization
Effect on Families
Nursing Care Management
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


The Child with Musculoskeletal or Articular Dysfunction
Get Clinical Tree app for offline access
