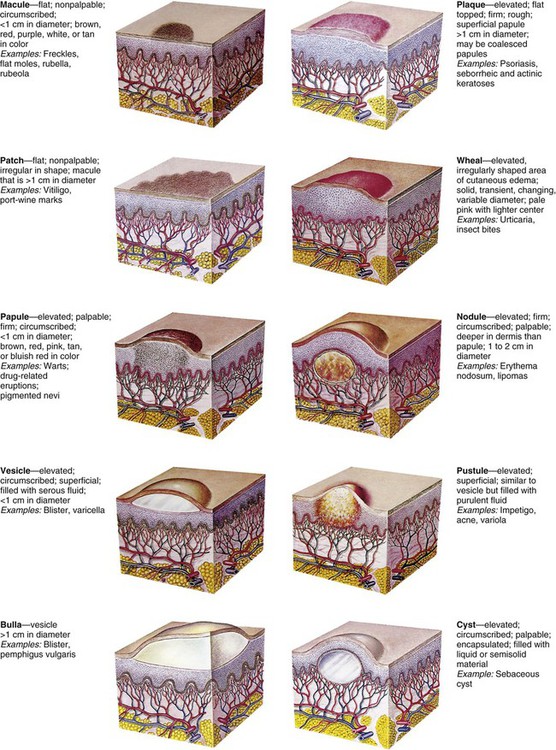
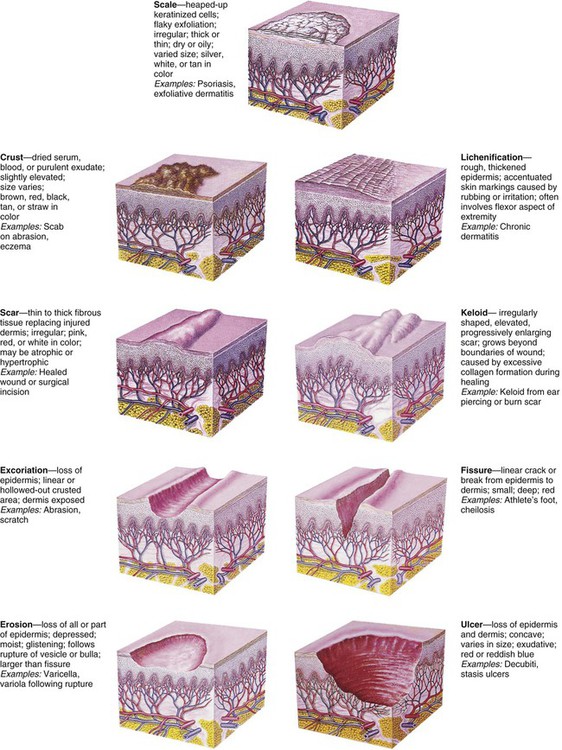
On completion of this chapter the reader will be able to: • Describe the distribution and configuration of various skin lesions. • List the benefits of a moist environment for wound healing. • Discuss the nursing care related to therapies for skin disorders. • Contrast the manifestations of and therapies for bacterial, viral, and fungal infections of the skin. • Compare the skin manifestations related to age in children. • Outline a care plan to prevent and treat diaper dermatitis. • Outline a care plan for a child with atopic dermatitis. • Formulate a teaching plan for an adolescent with acne. • Describe the methods for assessing a burn wound. • Discuss the physical and emotional care of a child with a severe burn wound. http://evolve.elsevier.com/wong/essentials Animations—Burns in Children; Tick Paralysis Case Studies—Acne Vulgaris; Burns; Impetigo; Poison Ivy; Tinea Capitis Nursing Care Plan—The Child with Burns: Management and Rehabilitative Stages Erythema—A reddened area caused by increased amounts of oxygenated blood in the dermal vasculature Ecchymoses (bruises)—Localized red or purple discolorations caused by extravasation of blood into dermis and subcutaneous tissues Petechiae—Pinpoint, tiny, and sharp circumscribed spots in the superficial layers of the epidermis Primary lesions—Skin changes produced by a causative factor; common primary lesions in pediatric skin disorders are macules, papules, and vesicles (Fig. 30-1) Secondary lesions—Changes that result from alteration in the primary lesions, such as those caused by rubbing, scratching, medication, or involution and healing (Fig. 30-2) Distribution pattern—The pattern in which lesions are distributed over the body, whether local or generalized, and the specific areas associated with the lesions Configuration and arrangement—The size, shape, and arrangement of a lesion or groups of lesions (e.g., discrete, clustered, diffuse, or confluent) When the skin is injured, its normal protective barrier function is broken. In a healthy immunocompetent individual, acute traumatic abrasions, lacerations, and superficial skin and soft tissue injuries heal spontaneously without complications. The process of tissue healing involves complex cellular interactions and biochemical reactions. The healing process is segregated into four phases that are characterized by the particular cells involved and the chemicals produced. The four stages of wound healing are hemostasis, inflammation, proliferation, and remodeling (Krasner, Rodeheaver, and Sibbald, 2007). Some authorities combine the first two phases. Numerous factors can delay healing (Table 30-1). For example, traditional practices, such as the use of antiseptics (hydrogen peroxide and povidone–iodine [Betadine] solutions), which were once thought to prevent infection, are now known to have a cytotoxic effect on healthy cells and minimal effect on controlling infections. Povidone–iodine may also be absorbed through the skin in neonates and young children. TABLE 30-1 FACTORS THAT DELAY WOUND HEALING DNA, Deoxyribonucleic acid; RBC, red blood cell; WBC, white blood cell. Some skin disorders demand aggressive therapy, but by and large, the major aim of treatment is to prevent further damage, eliminate the cause, prevent complications, and provide relief from discomfort while tissues undergo healing (McCord and Levy, 2006). Factors that contribute to the development of dermatitis and that prolong the course of the disease should be eliminated when possible. The most common causative agents of dermatitis in infants, children, and adolescents are environmental factors (soaps, bubble baths, shampoos, rough or tight clothing, wet diapers, blankets, and toys) and the natural elements (e.g., dirt, sand, heat, cold, moisture, and wind). Dermatitis may also result from home remedies and medications.
The Child with Integumentary Dysfunction
Integumentary Dysfunction
Skin Lesions
Diagnostic Evaluation
Types of Lesions
Wounds
Process of Wound Healing
Factors That Influence Healing
FACTOR
EFFECT ON HEALING
Dry wound environment
Allows epithelial cells to dry out and die; impairs migration of epithelial cells across wound surface
Nutritional deficiencies
Vitamin A
Results in inadequate inflammatory response
Vitamin B1
Results in decreased collagen formation
Vitamin C
Inhibits formation of collagen fibers and capillary development
Protein
Reduces supply of amino acids for tissue repair
Zinc
Impairs epithelialization
Immunocompromise
Results in inadequate or delayed inflammatory response
Impaired circulation
Inhibits inflammatory response and removal of debris from wound area
Reduces supply of nutrients to wound area
Stress (pain, poor sleep)
Releases catecholamines that cause vasoconstriction
Antiseptics
Hydrogen peroxide
Toxic to fibroblasts; can cause subcutaneous gas formation (mimics gas-forming infection)
Povidone–iodine
Toxic to WBCs, RBCs, and fibroblasts
Chlorhexidine
Toxic to WBCs
Medications
Corticosteroids
Impair phagocytosis
Inhibit fibroblast proliferation
Depress formation of granulation tissue
Inhibit wound contraction
Chemotherapy
Interrupts the cell cycle; damages DNA or prevents DNA repair
Antiinflammatory drugs
Decrease the inflammatory phase
Foreign bodies
Increase inflammatory response
Inhibit wound closure
Infection
Increases inflammatory response
Increases tissue destruction
Mechanical friction
Damages or destroys granulation tissue
Fluid accumulation
Accumulation in area inhibits tissues from approximating
Radiation
Inhibits fibroblastic activity and capillary formation
May cause tissue necrosis
Diseases
Diabetes mellitus
Inhibits collagen synthesis
Impairs circulation and capillary growth
Hyperglycemia impairs phagocytosis
Anemia
Reduces oxygen supply to tissues
Peripheral vascular disease
Reduces oxygen supply to wounds
Uremia
Decreases collagen and granulation tissue
General Therapeutic Management