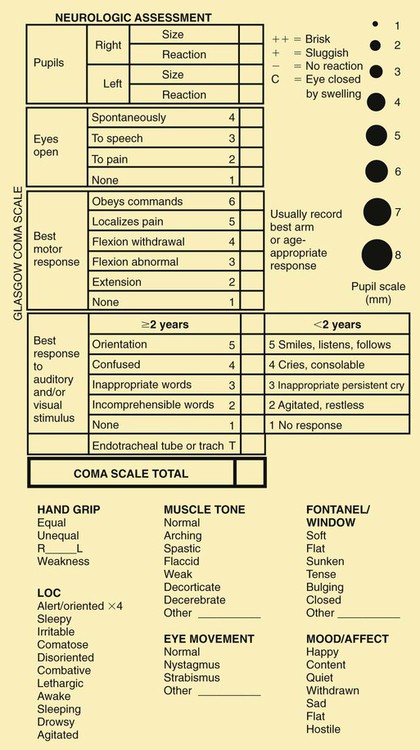
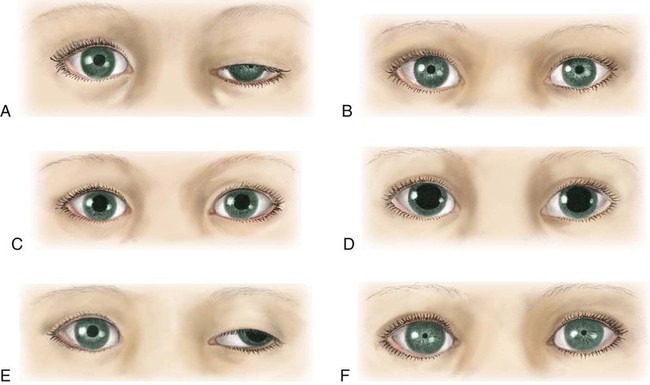
On completion of this chapter the reader will be able to: • Describe the various modalities for assessment of cerebral function. • Differentiate among the stages of consciousness. • Formulate a care plan for the unconscious child. • Distinguish among the types of head injuries and the serious complications. • Describe the nursing care of a child with a tumor of the central nervous system. • Outline a care plan for the child with bacterial meningitis. • Differentiate between the various types of seizure disorders. • Demonstrate an understanding of the manifestations of a seizure disorder and the management of a child with such a disorder. • Describe the preoperative and postoperative care of a child with hydrocephalus. http://evolve.elsevier.com/wong/essentials Animations—Blood Flow to Brain; Brain Anatomy; Brain Lobes; Cerebral Perfusion; Cervical Nerve Examination; Meningitis; Seizures; Subdural Hematoma; Ventriculoperitoneal Shunt Case Studies—Hydrocephalus with Myelomeningocele; Meningitis; Brain Tumor; Head Injury Nursing Care Plans—The Child with Bacterial Meningitis; The Child with Seizure Disorder; The Unconscious Child Most of the information about the status of the brain is obtained by indirect measurements. Some of these measurements are discussed elsewhere in relation to numerous aspects of child care (e.g., as part of assessments of health [Chapter 6], newborn status [Chapter 8], intellectual disability [Chapter 19], hypoxic injury [cerebral palsy, Chapter 32], and attainment of developmental milestones at each stage of development). Because increased intracranial pressure (ICP) and altered states of consciousness have such prominent places in neurologic dysfunction, they are described here followed by techniques for neurologic assessment and diagnostic tests. Early signs and symptoms of increased ICP are often subtle and assume many patterns (Box 28-1). As pressure increases, signs and symptoms become more pronounced, and the level of consciousness (LOC) deteriorates. Assessment of LOC remains the earliest indicator of improvement or deterioration in neurologic status. LOC is determined by observations of the child’s responses to the environment. When LOC is being assessed in young children, it is often useful to have a parent present to help elicit a desired response. An infant or child may not respond in an unfamiliar environment or to unfamiliar voices. Children older than 3 years of age should be able to give their name, although they may not be cognizant of place or time. Other diagnostic tests, such as motor activity, reflexes, and vital signs, are more variable and do not necessarily directly parallel the depth of the comatose state. The most consistently used terms are described in Box 28-2. Several scales have been devised in an attempt to standardize the description and interpretation of the degree of depressed consciousness. The most popular of these is the Glasgow Coma Scale (GCS), which consists of a three-part assessment: eye opening, verbal response, and motor response (Fig. 28-2). Numeric values of 1 through 5 are assigned to the levels of response in each category. The sum of these numeric values provides an objective measure of the patient’s LOC. A person with an unaltered LOC would score the highest, 15; a score of 8 or below is generally accepted as a definition of coma; and the lowest score, 3, indicates deep coma. A decrease in the GCS score indicates a deterioration of the patient’s condition. In 1987, major medical and legal societies developed specific guidelines for the determination of brain death among children of all ages (Mathur, Peterson, Stadtier, and others, 2008). General aspects of assessment that provide clues to the etiology of dysfunction include: Family history—Sometimes offers clues regarding possible genetic disorders with neurologic manifestations Health history—May provide valuable clues regarding the cause of dysfunction. Information should include Apgar scores, age of developmental milestones, trauma or injuries, acute and chronic illnesses, encounters with animals or insects, and ingestion or inhalation of neurotoxic substances. Physical evaluation of infants—Includes assessment of: • Size and shape of the head, including presence of fontanels • Motor function, including posture, tone, and muscle strength • Motility, including symmetry of movements and involuntary movements • Respirations, including signs of prolonged apnea, ataxic breathing, paradoxic chest movement, or hyperventilation • Behavioral cues, including consolability and habituation • Primitive and deep tendon reflexes Pupil size and reactivity are assessed (Fig. 28-3; see also Fig. 28-2). Pinpoint pupils are commonly observed in poisoning, such as opiate or barbiturate poisoning, and in brainstem dysfunction. Widely dilated and reactive pupils are often seen after seizures and may involve only one side. Dilated pupils may also be caused by eye trauma. Widely dilated and fixed pupils suggest paralysis of cranial nerve III secondary to pressure from herniation of the brain through the tentorium. A unilateral fixed pupil usually suggests a lesion on the same side. If pupils are fixed bilaterally for more than 5 minutes, brainstem damage is usually implied. Dilated and nonreactive pupils are also seen in hypothermia, anoxia, ischemia, poisoning with atropine-like substances, or prior instillation of mydriatic drugs. Special tests, usually performed by qualified persons, include: Doll’s head maneuver—Elicited by rotating the child’s head quickly to one side and then to the other. Conjugate (paired or working together) movement of the eyes in the direction opposite to the head rotation is normal. Absence of this response suggests dysfunction of the brainstem or oculomotor nerve (cranial nerve III). Caloric test, or oculovestibular response—Elicited with the child’s head up (head of bed is elevated 30 degrees) by irrigating the external auditory canal with 10 ml of ice water for 20 seconds, which normally causes conjugate movement of the eyes toward the side of stimulation. This movement is lost when the pontine centers are impaired, thus providing important information in assessment of the comatose patient. Funduscopic examination—Reveals additional clues. Papilledema will not be evident early in the course of unconsciousness because it takes 24 to 48 hours to develop, if it develops at all. Papilledema is characterized by optic disc swelling, indistinct optic disc margins, hemorrhage, tortuosity of vessels, and absence of venous pulsations. The presence of preretinal (subhyaloid) hemorrhages in children is almost invariably a result of acute trauma with intracranial bleeding, usually subarachnoid or subdural hemorrhage. Primitive postural reflexes emerge as cortical control over motor function is lost in brain dysfunction. These reflexes are evident in posturing and motor movements directly related to the area of the brain involved. Posturing reflects a balance between the lower exciting and the higher inhibiting influences and strong muscles overcoming weaker ones. Decorticate or flexion posturing (Fig. 28-4, A) is seen with severe dysfunction of the cerebral cortex or with lesions to corticospinal tracts above the brainstem. Typical posturing includes rigid flexion with the arms held tightly to the body; flexed elbows, wrists, and fingers; plantar flexed feet; legs extended and internally rotated; and possibly the presence of fine tremors or intense stiffness. Decerebrate posture or extension posturing (see Fig. 28-4, B) is a sign of dysfunction at the level of the midbrain or lesions to the brainstem. It is characterized by rigid extension and pronation of the arms and legs, flexed wrists and fingers, a clenched jaw, an extended neck, and possibly an arched back. Unilateral decerebrate posture is often caused by tentorial herniation. Testing of some reflexes may be of limited value. In general, the corneal, pupillary, muscle-stretch, superficial, and plantar reflexes tend to be absent in deep coma. The state of reflexes is variable in lighter grades of unconsciousness and depends on the underlying pathologic process and the location of the lesion. Absence of corneal reflexes and presence of a tonic neck reflex are associated with severe brain damage. The Babinski reflex (see Extremities, Chapter 6) may be of value if it is found to be present consistently in children older than 18 months. A positive Babinski reflex is significant in assessment of pyramidal tract lesions when it is unilateral and associated with other pyramidal signs. Highly sophisticated tests are carried out with specialized equipment. Two imaging techniques, computed tomography (CT) and magnetic resonance imaging (MRI), assist in diagnosis by scanning both soft tissues and solid matter. Most of these tests are outlined in Table 28-1. Because such tests can be threatening to children, the nurse needs to prepare patients for the tests and provide support and reassurance during the tests (see Preparation for Diagnostic and Therapeutic Procedures, Chapter 22). Children who are old enough to understand require careful explanation of the procedure, reason for the procedure, what they will experience, and how they can help. School-age children usually appreciate a more detailed description of why contrast material is injected. The importance of lying still for tests needs to be stressed. Children unfamiliar with the machines can be shown a picture beforehand. TABLE 28-1 NEUROLOGIC DIAGNOSTIC PROCEDURES The nurse should not expect cooperation from a young child. Sedation may be required. Many different agents are currently used for sedation of children undergoing neurologic diagnostic procedures. Chloral hydrate, pentobarbital, or benzodiazepines have been used for decades as short-term sedative agents and remain safe methods of pediatric outpatient sedation (Mason, 2008). Chloral hydrate and pentobarbital have no analgesic proprieties but can provide successful sedation for nonpainful procedures such as CT and MRI (Mason, 2008). In recent years, propofol has been used as a sedation agent for diagnostic procedures because of its short induction and recovery time, but this medication should be used with caution because it can cause respiratory depression and apnea with little warning (Machata, Willschke, Kabon, and others, 2008; Mason, 2008). (See Pain Management, Chapter 7.) Vital signs provide important information about the status of the unconscious child. Hypothalamic and brainstem disorders may affect the patient’s thermoregulation, so frequent monitoring is needed. The temperature is taken every 2 to 4 hours, depending on the patient’s condition. Hypothermia is defined as a core body temperature less than 35° C (95° F). EEG slowing is noted at 30° C, and loss of pupillary light reflex is lost at 28° C (Young, 2009). Hyperthermia is defined as a core body temperature greater than 38.5° C (101.3° F) and temperatures greater than 42° C can cause EEG slowing, seizures, and encephalopathy (Young, 2009). The neurologic examination is performed periodically and includes evaluating pupillary abnormalities, brainstem function, LOC, and motor response (Sharma, Kochar, Sankhyan, and other, 2010). Pupils are observed for their size, symmetry, and reaction to light. Signs of meningeal irritation such as nuchal rigidity are also assessed. The presence of the oculovestibular response, corneal (blink) response, and cough and gag reflexes are evaluated. Aspects of LOC assessment include response to vocal commands, resistance to care, and response to painful stimuli. Spontaneous movement, changes in muscle tone or strength, and body position are noted. Seizure activity is described according to the duration and body areas involved. Pain management for the comatose child requires astute nursing observation and management. Responses to pain include motor reactions such as increased agitation or posturing; facial changes such as grimaces; and physiological reactions such as tachycardia, tachypnea, diaphoresis, or hypertension (Schnakers and Zasler, 2007). Because these findings may not be specific for pain, the nurse should observe for their appearance during times of induced or suspected pain and their disappearance after the end of the inciting procedure or the administration of analgesia. A pain assessment record should be used to document indications of pain and the effectiveness of interventions (see Pain Assessment, Chapter 7). The use of opioids, such as morphine, to relieve pain is controversial because they may mask signs of altered consciousness or depress respirations. However, unrelieved pain activates the stress response, which can elevate ICP. To block the stress response, some authorities advocate the use of analgesics; sedatives; and, in some cases, paralyzing agents via continuous intravenous (IV) infusion. A frequently used combination is fentanyl, midazolam, and vecuronium (Norcuron). If there are concerns about assessing the LOC or respiratory depression, naloxone (Narcan) can be used to reverse the opioid effects. Regardless of which drugs are used, adequate dosage and regular administration are essential to provide optimal pain relief (see Pain Management, Chapter 7). An oral airway can be used for children who have a temporary loss of consciousness, such as after a contusion, seizure, or anesthesia. For children who remain unconscious for a longer time, a nasotracheal or orotracheal tube is inserted to maintain the open airway and facilitate removal of secretions. Endotracheal intubation should be considered in children with a GCS score of less than 8, evidence of herniation, apnea, or inability to maintain an airway (Sankhyan, Raju, Sharma, and other, 2010). A tracheostomy is performed in cases in which laryngoscopy for introduction of an endotracheal tube would be difficult or for a child who needs long-term ventilatory support. Suctioning is used only as needed to clear the airway, exerting care to prevent increasing ICP. Respiratory status is observed and evaluated regularly. Signs of respiratory distress may be an indication for ventilatory assistance. When the respiratory center is involved, mechanical ventilation is usually indicated (see Chapter 22). Blood gas analysis is performed regularly, and oxygen is administered as indicated. Moderately severe hypoxia and respiratory acidosis are often present but not always evident from clinical manifestations. Hyperventilation frequently accompanies unconsciousness and may lead to respiratory alkalosis, or it may represent the body’s attempt to compensate for metabolic acidosis. Therefore, blood gas and pH determinations are essential guides for therapy. Chest physiotherapy is carried out on a regular basis, and the child’s position is changed at least every 2 hours to prevent pulmonary complications. • GCS evaluation of less than 8 • Traumatic brain injury with an abnormal head CT scan • Subjective judgment regarding clinical appearance and response Four major types of ICP monitors are 1. Intraventricular catheter with fibroscopic sensors attached to a monitoring system 2. Subarachnoid bolt (Richmond screw) Direct ventricular pressure measurement with an intraventricular catheter remains the gold standard of ICP monitoring (Singhi and Tiwari, 2009). Subarachnoid and epidural monitoring can be used when a catheter cannot be cannulated in the ventricle, but they often must be replaced after several days because of measurement drift (Singhi and Tiwari, 2009). Transducers for both ventricular and subarachnoid monitoring should be set up without the use of a flush device. Intracranial pressure can be increased by instillation of solutions; therefore, antibiotics are administered systemically if a positive CSF culture is obtained. CSF is a body fluid; therefore, standard precautions are implemented according to hospital policy (see Infection Control, Chapter 22). For sustained ICP elevations greater than 20 to 25 mm Hg, several medical measures are available. Osmotic diuretics may provide rapid relief in emergency situations. Although their effect is transient, lasting only about 6 hours, they can be lifesaving in emergencies. These substances are rapidly excreted by the kidneys and carry with them large quantities of sodium and water. Mannitol (or sometimes urea) administered intravenously is the drug most frequently used for rapid reduction and can lower ICP in 1 to 5 minutes. The infusion is generally given slowly but may be pushed rapidly in cases of herniation or impending herniation. Hypertonic saline in concentrations of 3% to 23% have been shown to reduce ICP by its osmotic force and can be beneficial for hypovolemic and hypotensive patients by increasing intravascular volume and blood pressure (Singhi and Tiwari, 2009). Adrenocorticosteroids are not recommended for cerebral edema secondary to head trauma. PaCO2 should be maintained at 25 to 30 mm Hg to produce vasoconstriction, which reduces CSF, thereby decreasing ICP, but this effect is sustained only 11 to 20 hours because the CSF equilibrates to the new PaCO2 level (Singhi and Tiwari, 2009). It is important to avoid activities that may increase ICP by causing pain or emotional stress. Gentle range-of-motion exercises can be carried out but should not be performed vigorously. Nontherapeutic touch can cause an increase in ICP. Any disturbing procedures to be performed should be scheduled to take advantage of therapies that reduce ICP, such as osmotherapy and sedation. Efforts are taken to minimize or eliminate environmental noise. Assessment and intervention to relieve pain are important nursing functions to decrease ICP. Individualizing nursing activities and minimizing environmental stimuli by decreasing elective procedures help control ICP (Sankhyan, Raju, Sharma, and other, 2010). In the unconscious child, fluids and calories are supplied initially by the IV route (see Chapter 22). An IV infusion is started early, and the type of fluid administered is determined by the patient’s general condition. Fluid therapy requires careful monitoring and adjustment based on neurologic signs and electrolyte determinations. The goal of fluid therapy is euvolemia. Often, comatose children are unable to cope with the same amounts of fluid they could tolerate when they are healthy, and overhydration must be avoided to prevent fatal cerebral edema. When cerebral edema is a threat, fluids may be restricted to reduce the chance of fluid overload. Skin and mucous membranes are examined for signs of dehydration. Observation for signs of altered fluid balance related to abnormal pituitary secretions is a part of nursing care. An altered ability to handle fluid loads is attributed in part to the syndrome of inappropriate antidiuretic hormone secretion (SIADH) and diabetes insipidus (DI) resulting from hypothalamic dysfunction (see Chapter 29). SIADH frequently accompanies CNS diseases such as head injury, meningitis, encephalitis, brain abscess, brain tumor, and subarachnoid hemorrhage. In patients with SIADH, scant quantities of urine are excreted, electrolyte analysis reveals hyponatremia and hyposmolality, and manifestations of overhydration are evident. It is important to evaluate all parameters because the reduced urinary output might be erroneously interpreted as a sign of dehydration. The treatment of SIADH consists of restriction of fluids until serum electrolytes and osmolality return to normal levels. The cause of unconsciousness determines specific drug therapies. Children with infectious processes are given antibiotics appropriate to the disease and the infecting organism. Corticosteroids are prescribed for inflammatory conditions and edema. Cerebral edema is an indication for osmotherapy. Sedatives or antiepileptics are prescribed for seizure activity (see p. 960). Hyperthermia often accompanies cerebral dysfunction; if it is present, measures are implemented to reduce the temperature to prevent brain damage and to reduce metabolic demands generated by the increased body temperature. Antipyretic agents are usually ineffective with hyperthermia as a result of traumatic brain injury; therefore, external cooling should be used (Badjatia, 2009). External cooling consists of evaporation (sponge baths), conduction (ice packs, cooling blankets), convection (fans), and radiation (skin exposure) (Badjatia, 2009). Laboratory tests and other methods are used in an attempt to determine the cause of the hyperthermia.
The Child with Cerebral Dysfunction
Cerebral Dysfunction
Increased Intracranial Pressure
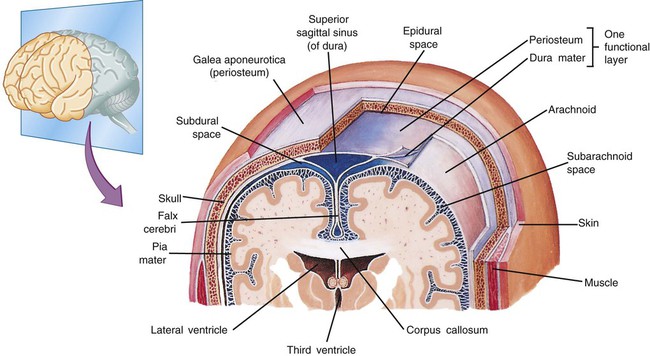
![]() The brain, tightly enclosed in the solid bony cranium, is well protected but highly vulnerable to pressure that may accumulate within the enclosure (Fig. 28-1). The cranium’s total volume—brain (80%), cerebrospinal fluid (CSF) (10%), and blood (10%)—must remain approximately the same at all times. A change in the proportional volume of one of these components (e.g., increase or decrease in intracranial blood) must be accompanied by a compensatory change in another. In this way, the volume and pressure normally remain constant. Examples of compensatory changes are reduction in blood volume, decrease in CSF production, increase in CSF absorption, or shrinkage of brain mass by displacement of intracellular and extracellular fluid. Children with open fontanels compensate by skull expansion and widened sutures. However, at any age, the capacity for spatial compensation is limited. An increase in ICP may be caused by tumors or other space-occupying lesions, accumulation of fluid within the ventricular system, bleeding, or edema of cerebral tissues. When compensation is exhausted, any further increase in the cranium’s volume will result in a rapid rise in ICP.
The brain, tightly enclosed in the solid bony cranium, is well protected but highly vulnerable to pressure that may accumulate within the enclosure (Fig. 28-1). The cranium’s total volume—brain (80%), cerebrospinal fluid (CSF) (10%), and blood (10%)—must remain approximately the same at all times. A change in the proportional volume of one of these components (e.g., increase or decrease in intracranial blood) must be accompanied by a compensatory change in another. In this way, the volume and pressure normally remain constant. Examples of compensatory changes are reduction in blood volume, decrease in CSF production, increase in CSF absorption, or shrinkage of brain mass by displacement of intracellular and extracellular fluid. Children with open fontanels compensate by skull expansion and widened sutures. However, at any age, the capacity for spatial compensation is limited. An increase in ICP may be caused by tumors or other space-occupying lesions, accumulation of fluid within the ventricular system, bleeding, or edema of cerebral tissues. When compensation is exhausted, any further increase in the cranium’s volume will result in a rapid rise in ICP.
![]() Animation—Brain Anatomy; Brain Lobes
Animation—Brain Anatomy; Brain Lobes
Altered States of Consciousness
Levels of Consciousness
Coma Assessment
General Aspects
Neurologic Examination
![]() Animation—Cervical Nerve Examination
Animation—Cervical Nerve Examination
Eyes
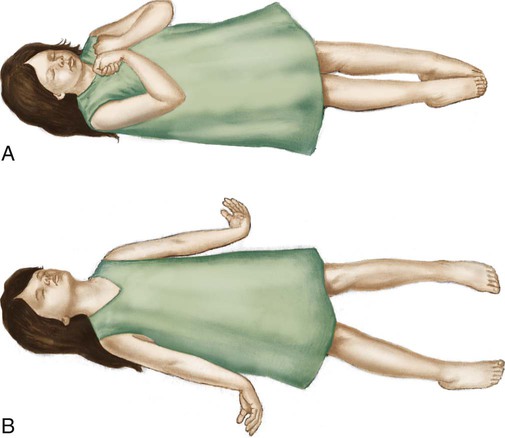
Posturing
Reflexes
Special Diagnostic Procedures
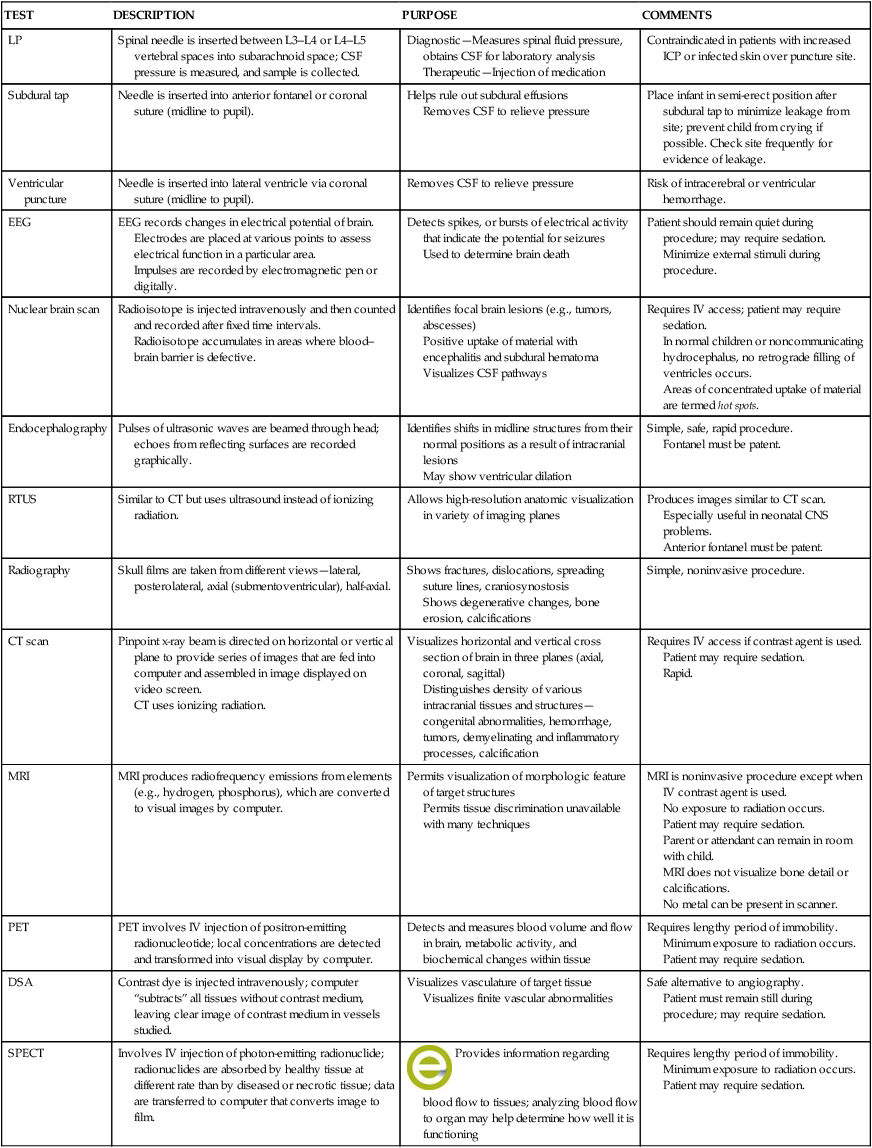
TEST
DESCRIPTION
PURPOSE
COMMENTS
LP
Spinal needle is inserted between L3–L4 or L4–L5 vertebral spaces into subarachnoid space; CSF pressure is measured, and sample is collected.
Diagnostic—Measures spinal fluid pressure, obtains CSF for laboratory analysis
Therapeutic—Injection of medication
Contraindicated in patients with increased ICP or infected skin over puncture site.
Subdural tap
Needle is inserted into anterior fontanel or coronal suture (midline to pupil).
Helps rule out subdural effusions
Removes CSF to relieve pressure
Place infant in semi-erect position after subdural tap to minimize leakage from site; prevent child from crying if possible. Check site frequently for evidence of leakage.
Ventricular puncture
Needle is inserted into lateral ventricle via coronal suture (midline to pupil).
Removes CSF to relieve pressure
Risk of intracerebral or ventricular hemorrhage.
EEG
EEG records changes in electrical potential of brain.
Electrodes are placed at various points to assess electrical function in a particular area.
Impulses are recorded by electromagnetic pen or digitally.
Detects spikes, or bursts of electrical activity that indicate the potential for seizures
Used to determine brain death
Patient should remain quiet during procedure; may require sedation.
Minimize external stimuli during procedure.
Nuclear brain scan
Radioisotope is injected intravenously and then counted and recorded after fixed time intervals.
Radioisotope accumulates in areas where blood–brain barrier is defective.
Identifies focal brain lesions (e.g., tumors, abscesses)
Positive uptake of material with encephalitis and subdural hematoma
Visualizes CSF pathways
Requires IV access; patient may require sedation.
In normal children or noncommunicating hydrocephalus, no retrograde filling of ventricles occurs.
Areas of concentrated uptake of material are termed hot spots.
Endocephalography
Pulses of ultrasonic waves are beamed through head; echoes from reflecting surfaces are recorded graphically.
Identifies shifts in midline structures from their normal positions as a result of intracranial lesions
May show ventricular dilation
Simple, safe, rapid procedure.
Fontanel must be patent.
RTUS
Similar to CT but uses ultrasound instead of ionizing radiation.
Allows high-resolution anatomic visualization in variety of imaging planes
Produces images similar to CT scan.
Especially useful in neonatal CNS problems.
Anterior fontanel must be patent.
Radiography
Skull films are taken from different views—lateral, posterolateral, axial (submentoventricular), half-axial.
Shows fractures, dislocations, spreading suture lines, craniosynostosis
Shows degenerative changes, bone erosion, calcifications
Simple, noninvasive procedure.
CT scan
Pinpoint x-ray beam is directed on horizontal or vertical plane to provide series of images that are fed into computer and assembled in image displayed on video screen.
CT uses ionizing radiation.
Visualizes horizontal and vertical cross section of brain in three planes (axial, coronal, sagittal)
Distinguishes density of various intracranial tissues and structures—congenital abnormalities, hemorrhage, tumors, demyelinating and inflammatory processes, calcification
Requires IV access if contrast agent is used.
Patient may require sedation.
Rapid.
MRI
MRI produces radiofrequency emissions from elements (e.g., hydrogen, phosphorus), which are converted to visual images by computer.
Permits visualization of morphologic feature of target structures
Permits tissue discrimination unavailable with many techniques
MRI is noninvasive procedure except when IV contrast agent is used.
No exposure to radiation occurs.
Patient may require sedation.
Parent or attendant can remain in room with child.
MRI does not visualize bone detail or calcifications.
No metal can be present in scanner.
PET
PET involves IV injection of positron-emitting radionucleotide; local concentrations are detected and transformed into visual display by computer.
Detects and measures blood volume and flow in brain, metabolic activity, and biochemical changes within tissue
Requires lengthy period of immobility.
Minimum exposure to radiation occurs.
Patient may require sedation.
DSA
Contrast dye is injected intravenously; computer “subtracts” all tissues without contrast medium, leaving clear image of contrast medium in vessels studied.
Visualizes vasculature of target tissue
Visualizes finite vascular abnormalities
Safe alternative to angiography.
Patient must remain still during procedure; may require sedation.
SPECT
Involves IV injection of photon-emitting radionuclide; radionuclides are absorbed by healthy tissue at different rate than by diseased or necrotic tissue; data are transferred to computer that converts image to film.
![]() Provides information regarding blood flow to tissues; analyzing blood flow to organ may help determine how well it is functioning
Provides information regarding blood flow to tissues; analyzing blood flow to organ may help determine how well it is functioning
Requires lengthy period of immobility.
Minimum exposure to radiation occurs.
Patient may require sedation.
![]() Animation—Blood Flow to the Brain
Animation—Blood Flow to the Brain
Nursing Care of the Unconscious Child
![]() Nursing Care Plan—The Unconscious Child
Nursing Care Plan—The Unconscious Child
Respiratory Management
Intracranial Pressure Monitoring
![]() An acute rise in ICP can cause secondary brain injury (Singhi and Tiwari, 2009), and management of the child with increased ICP is a complex and important task. ICP monitoring is used to guide therapy to reduce ICP and provides information on intracranial compliance, cerebrovascular status, and cerebral perfusion (Sankhyan, Raju, Sharma, and other, 2010). Nonetheless, ICP monitoring is an invasive procedure that has associated risks, including infection, hemorrhage, malfunction, and obstruction (Singhi and Tiwari, 2009). Indications for inserting an ICP monitor are as follows:
An acute rise in ICP can cause secondary brain injury (Singhi and Tiwari, 2009), and management of the child with increased ICP is a complex and important task. ICP monitoring is used to guide therapy to reduce ICP and provides information on intracranial compliance, cerebrovascular status, and cerebral perfusion (Sankhyan, Raju, Sharma, and other, 2010). Nonetheless, ICP monitoring is an invasive procedure that has associated risks, including infection, hemorrhage, malfunction, and obstruction (Singhi and Tiwari, 2009). Indications for inserting an ICP monitor are as follows:
Nursing Activities
Nutrition and Hydration
Altered Pituitary Secretion
Medications
Thermoregulation
The Child with Cerebral Dysfunction
Get Clinical Tree app for offline access