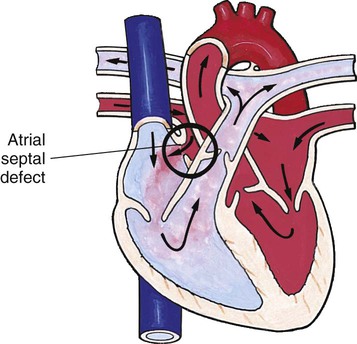
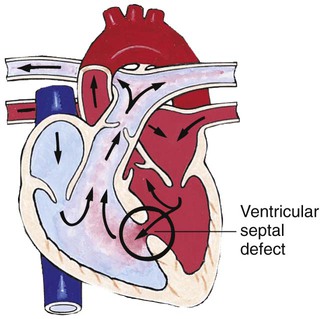
On completion of this chapter the reader will be able to: • Design a plan for assisting children during cardiac diagnostic procedures. • Demonstrate an understanding of the hemodynamics, distinctive manifestations, and therapeutic management of congenital heart disease. • Outline a care plan for an infant or child with heart failure. • Describe the care for a child who has hypoxia. • Describe the care for an infant or a child with a congenital heart defect and its surgical repair. • Discuss the nurse’s role in helping the child and family cope with congenital heart disease. • Differentiate between rheumatic fever and rheumatic heart disease. • List the criteria for selected cholesterol screening of children. • Discuss the assessment and management of hypertension in children and adolescents. • Outline a care plan for a child with Kawasaki disease. • Describe the emergency treatment for shock, including anaphylaxis. http://evolve.elsevier.com/wong/essentials Animations—Cardiac Tamponade, Infant; Catheter Placement, Umbilical Vein; Fetal Circulation; Heart Sounds; Hypoxia; Structure of the Heart; Subaortic Stenosis Case Study—Patent Ductus Arteriosus Nursing Care Plans—The Child with Heart Failure; The Child in Shock (Cardiovascular Failure) The physical assessment of suspected cardiac disease begins with observation of general appearance and then proceeds with more specific observations. The following are supplementary to the general assessment techniques described for physical examination of the chest and heart in Chapter 6: Nutritional state—Failure to thrive or poor weight gain is associated with heart disease. Color—Cyanosis is a common feature of CHD, and pallor is associated with poor perfusion. Chest deformities—An enlarged heart sometimes distorts the chest configuration. Unusual pulsations—Visible pulsations of the neck veins are seen in some patients. Respiratory excursion—This refers to the ease or difficulty of respiration (e.g., tachypnea, dyspnea, expiratory grunt). A variety of invasive and noninvasive tests may be used in the diagnosis of heart disease (Table 25-1). Some of the more common diagnostic tools that require nursing assessment and intervention are described here. TABLE 25-1 PROCEDURES FOR CARDIAC DIAGNOSIS Diagnostic catheterizations—These studies are used to diagnose congenital cardiac defects, particularly in symptomatic infants and before surgical repair. They are divided into right-sided catheterizations, in which the catheter is introduced through a vein (usually the femoral vein) and threaded to the right atrium (most common), and left-sided catheterizations, in which the catheter is threaded through an artery into the aorta and into the heart. Interventional catheterizations (therapeutic catheterizations)—A balloon catheter or other device is used to alter the cardiac anatomy. Examples include dilating stenotic valves or vessels or closing abnormal connections (Table 25-2). TABLE 25-2 CURRENT INTERVENTIONAL CARDIAC CATHETERIZATION PROCEDURES IN CHILDREN Data from Allen HD, Beekman RH 3rd, Garson A Jr, and others: Pediatric therapeutic cardiac catheterization: AHA scientific statement, Circulation 97:609–625, 1998; updated from Rome J, Kreutzer J: Pediatric interventional catheterization: reasonable expectations and outcomes, Pediatr Clin North Am 51:1589–1610, 2004. Electrophysiology studies—Catheters with tiny electrodes that record the impulses of the heart directly from the conduction system are used to evaluate dysrhythmias and sometimes destroy accessory pathways that cause some tachydysrhythmias. Cardiac catheterization has become a routine diagnostic procedure and may be done on an outpatient basis. However, it is not without risks, especially in neonates and seriously ill infants and children. Possible complications include acute hemorrhage from the entry site (more likely with interventional procedures because larger catheters are used), low-grade fever, nausea, vomiting, loss of pulse in the catheterized extremity (usually transient, resulting from a clot, hematoma, or intimal tear), and transient dysrhythmias (generally catheter induced) (Uzark, 2001). Rare risks include stroke, seizures, tamponade, and death. Preparing the child and family for the procedure is the joint responsibility of the patient care team. School-age children and adolescents benefit from a description of the catheterization laboratory and a chronologic explanation of the procedure, emphasizing what they will see, feel, and hear. Older children and adolescents may bring earphones and favorite music so they can listen during the catheterization procedure. Preparation materials such as picture books, videotapes, or tours of the catheterization laboratory may be helpful. Preparation should be geared to the child’s developmental level. The child’s caregivers often benefit from the same explanations. Additional information, such as the expected length of the catheterization, description of the child’s appearance after catheterization, and usual postprocedure care, should be outlined. (See also Prepare the Child and Family for Invasive Procedures, p. 845.) Methods of sedation vary among institutions and may include oral or intravenous (IV) medications (see Chapter 22). The child’s age, heart defect, clinical status, and type of catheterization procedure planned are considered when sedation is determined. General anesthesia may be needed for some interventional procedures. Children are allowed nothing by mouth (NPO) for 4 to 6 hours or more before the procedure according to institutional guidelines. Infants and patients with polycythemia may need IV fluids to prevent dehydration and hypoglycemia. • Pulses, especially below the catheterization site, for equality and symmetry (Pulse distal to the site may be weaker for the first few hours after catheterization but should gradually increase in strength.) • Temperature and color of the affected extremity because coolness or blanching may indicate arterial obstruction • Vital signs, which are taken as frequently as every 15 minutes, with special emphasis on heart rate, which is counted for 1 full minute for evidence of dysrhythmias or bradycardia • Blood pressure (BP), especially for hypotension, which may indicate hemorrhage from cardiac perforation or bleeding at the site of initial catheterization • Dressing, for evidence of bleeding or hematoma formation in the femoral or antecubital area • Fluid intake, both IV and oral, to ensure adequate hydration (Blood loss in the catheterization laboratory, the child’s NPO status, and diuretic actions of dyes used during the procedure put children at risk for hypovolemia and dehydration.) • Blood glucose levels for hypoglycemia, especially in infants, who should receive dextrose-containing IV fluids The incidence of CHD in children is approximately 5 to 8 per 1000 live births (Park, 2008). About 2 or 3 in 1000 infants will be symptomatic during the first year of life with significant heart disease that requires treatment (Hoffman and Kaplan, 2002). CHD is the major cause of death (other than prematurity) in the first year of life. Although there are more than 35 well-recognized cardiac defects, the most common heart anomaly is ventricular septal defect (VSD). Before birth, the high pulmonary vascular resistance created by the collapsed fetal lung causes greater pressures in the right side of the heart and the pulmonary arteries. At the same time, the free-flowing placental circulation and the ductus arteriosus produce a low vascular resistance in the remainder of the fetal vascular system. With the cessation of placental blood flow from clamping of the umbilical cord and the expansion of the lungs at birth, the hemodynamics of the fetal vascular system undergo pronounced and abrupt changes (Fig. 25-2, B). A more useful classification system is based on hemodynamic characteristics (blood flow patterns within the heart). These blood flow patterns are (1) increased pulmonary blood flow; (2) decreased pulmonary blood flow; (3) obstruction to blood flow out of the heart; and (4) mixed blood flow, in which saturated and desaturated blood mix within the heart or great arteries. As a comparison, Figure 25-3 outlines both classification systems. With the hemodynamic classification system, the clinical manifestations of each group are more uniform and predictable. Defects that allow blood flow from the higher pressure left side of the heart to the lower pressure right side (left-to-right shunt) result in increased pulmonary blood flow and cause heart failure (HF). Obstructive defects impede blood flow out of the ventricles; whereas obstruction on the left side of the heart results in HF, severe obstruction on the right side causes cyanosis. Defects that cause decreased pulmonary blood flow result in cyanosis. Mixed lesions present a variable clinical picture based on the degree of mixing and amount of pulmonary blood flow; hypoxemia (with or without cyanosis) and HF usually occur together. Using this classification system, the clinical presentation and management of the most common defects are outlined in the following sections and Box 25-1.
The Child with Cardiovascular Dysfunction
Cardiovascular Dysfunction
![]() Animation—Structure of the Heart
Animation—Structure of the Heart
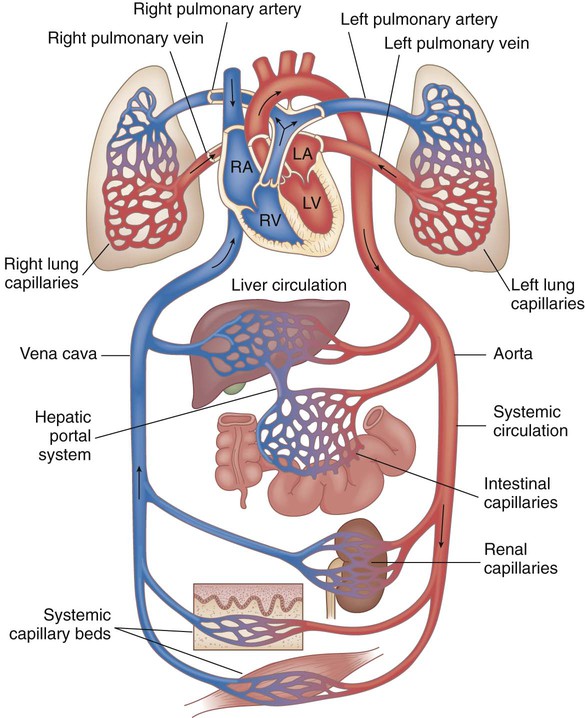
![]() Cardiovascular disorders in children are divided into two major groups, congenital heart disease and acquired heart disorders. Congenital heart disease (CHD) includes primarily anatomic abnormalities present at birth that result in abnormal cardiac function. The clinical consequences of congenital heart defects fall into two broad categories, heart failure (HF) and hypoxemia. Acquired cardiac disorders are disease processes or abnormalities that occur after birth and can be seen in the normal heart or in the presence of congenital heart defects. They result from various factors, including infection, autoimmune responses, environmental factors, and familial tendencies. The pathophysiology review found in Figure 25-1 describes the flow of blood through the heart.
Cardiovascular disorders in children are divided into two major groups, congenital heart disease and acquired heart disorders. Congenital heart disease (CHD) includes primarily anatomic abnormalities present at birth that result in abnormal cardiac function. The clinical consequences of congenital heart defects fall into two broad categories, heart failure (HF) and hypoxemia. Acquired cardiac disorders are disease processes or abnormalities that occur after birth and can be seen in the normal heart or in the presence of congenital heart defects. They result from various factors, including infection, autoimmune responses, environmental factors, and familial tendencies. The pathophysiology review found in Figure 25-1 describes the flow of blood through the heart.
History and Physical Examination
Inspection
Diagnostic Evaluation
PROCEDURE
DESCRIPTION
Chest radiography (x-ray)
Provides information on heart size and pulmonary blood flow patterns
ECG
Graphic measure of electrical activity of heart
Holter monitor
24-hour continuous ECG recording used to assess dysrhythmias
Echocardiography
Use of high-frequency sound waves obtained by a transducer to produce an image of cardiac structures
Transthoracic
Done with transducer on chest
M-mode
One-dimensional graphic view used to estimate ventricular size and function
Two-dimensional
Real-time, cross-sectional views of heart used to identify cardiac structures and cardiac anatomy
Doppler
Identifies blood flow patterns and pressure gradients across structures
Fetal
Imaging fetal heart in utero
TEE
Transducer placed in esophagus behind heart to obtain images of posterior heart structures or in patients with poor images from chest approach
Cardiac catheterization
Imaging study using radiopaque catheters placed in a peripheral blood vessel and advanced into heart to measure pressures and oxygen levels in heart chambers and visualize heart structures and blood flow patterns
Hemodynamics
Measures pressures and oxygen saturations in heart chambers
Angiography
Use of contrast material to illuminate heart structures and blood flow patterns
Biopsy
Use of special catheter to remove tiny samples of heart muscle for microscopic evaluation; used in assessing infection, inflammation, or muscle dysfunction disorders; also to evaluate for rejection after heart transplant
EPS
Special catheters with electrodes employed to record electrical activity from within heart; used to diagnose rhythm disturbances
Exercise stress test
Monitoring of heart rate, blood pressure, ECG, and oxygen consumption at rest and during progressive exercise on a treadmill or bicycle
Cardiac MRI
Noninvasive imaging technique; used in evaluation of vascular anatomy outside of heart (e.g., COA, vascular rings), estimates of ventricular mass and volume; uses for MRI are expanding
Cardiac Catheterization
![]() Animation—Catheter Placement, Umbilical Vein
Animation—Catheter Placement, Umbilical Vein
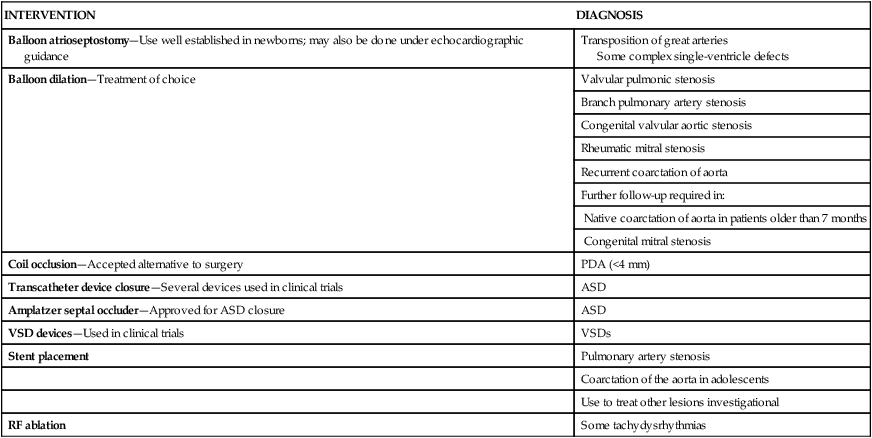
INTERVENTION
DIAGNOSIS
Balloon atrioseptostomy—Use well established in newborns; may also be done under echocardiographic guidance
Transposition of great arteries
Some complex single-ventricle defects
Balloon dilation—Treatment of choice
Valvular pulmonic stenosis
Branch pulmonary artery stenosis
Congenital valvular aortic stenosis
Rheumatic mitral stenosis
Recurrent coarctation of aorta
Further follow-up required in:
Native coarctation of aorta in patients older than 7 months
Congenital mitral stenosis
Coil occlusion—Accepted alternative to surgery
PDA (<4 mm)
Transcatheter device closure—Several devices used in clinical trials
ASD
Amplatzer septal occluder—Approved for ASD closure
ASD
VSD devices—Used in clinical trials
VSDs
Stent placement
Pulmonary artery stenosis
Coarctation of the aorta in adolescents
Use to treat other lesions investigational
RF ablation
Some tachydysrhythmias
Nursing Care Management
Preprocedural Care
Postprocedural Care
Congenital Heart Disease
Circulatory Changes at Birth
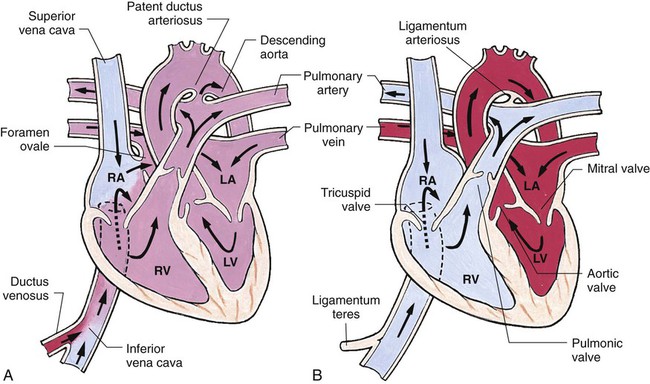
![]() Blood carrying oxygen and nutritive materials from the placenta enters the fetal system through the umbilicus via the large umbilical vein. The blood then travels to the liver, where it divides. Part of the blood enters the portal and hepatic circulation of the liver, and the remainder travels directly to the inferior vena cava (IVC) by way of the ductus venosus. Oxygenated blood enters the heart by way of the IVC. Because of the higher pressure of blood entering the right atrium, it is directed posteriorly in a straight pathway across the right atrium and through the foramen ovale to the left atrium. In this way, the better-oxygenated blood enters the left atrium and ventricle to be pumped through the aorta to the head and upper extremities. Blood from the head and upper extremities entering the right atrium from the superior vena cava is directed downward through the tricuspid valve into the right ventricle. From there it is pumped through the pulmonary artery, where the major portion is shunted to the descending aorta via the ductus arteriosus. Only a small amount flows to and from the nonfunctioning fetal lungs (Fig. 25-2, A).
Blood carrying oxygen and nutritive materials from the placenta enters the fetal system through the umbilicus via the large umbilical vein. The blood then travels to the liver, where it divides. Part of the blood enters the portal and hepatic circulation of the liver, and the remainder travels directly to the inferior vena cava (IVC) by way of the ductus venosus. Oxygenated blood enters the heart by way of the IVC. Because of the higher pressure of blood entering the right atrium, it is directed posteriorly in a straight pathway across the right atrium and through the foramen ovale to the left atrium. In this way, the better-oxygenated blood enters the left atrium and ventricle to be pumped through the aorta to the head and upper extremities. Blood from the head and upper extremities entering the right atrium from the superior vena cava is directed downward through the tricuspid valve into the right ventricle. From there it is pumped through the pulmonary artery, where the major portion is shunted to the descending aorta via the ductus arteriosus. Only a small amount flows to and from the nonfunctioning fetal lungs (Fig. 25-2, A).
Classification of Defects