The Child with an Infectious Disease
Learning Objectives
After studying this chapter, you should be able to:
• Analyze the infectious process.
• Compare the modes of transmission of infectious diseases.
• Use the nursing process to describe the nursing care of a child with an infectious disease.
![]()
http://evolve.elsevier.com/McKinney/mat-ch
Clinical Reference
Review of Disease Transmission
Microorganisms exist throughout the environment. Most are harmless residents and a normal part of human flora. An organism that invades body tissue, causing tissue damage and disease, however, is a pathogen. For pathogens to invade a host, they must breach the normal host defenses, by either attaching to or penetrating the host. The power of these pathogens, known as their virulence, depends on their ability to overcome the host defense mechanisms. Thus a highly virulent organism can cause disease with relative ease.
Microorganisms that cause infectious disease are classified into five types: bacteria, viruses and rickettsiae, fungi, protozoa, and helminths.
Exogenous pathogens are transmitted from outside the body to the host by various mechanisms. Exogenous organisms exist in contaminated air, food, water, and body fluids and on objects contaminated by these substances. Endogenous pathogens are found within the human body. Microorganisms (normal flora) exist on the skin and in the nose, mouth, gastrointestinal tract, and urogenital tract. For example, Staphylococcus epidermidis inhabits the skin, and Escherichia coli are found in the intestines. These microorganisms are beneficial and play an important role in the body’s defenses. They help prevent virulent pathogens from colonizing by maintaining an acidic pH environment to discourage pathogen attachment, taking up epithelial space to prevent growth of pathogens, and stimulating the immune system. However, situations may arise in which these normally benign organisms become virulent and harmful to the host.
Chain of Infection
For a pathogen to maintain its infectious state, it must be transmitted to another host. Certain factors and conditions must be present for a disease (infection) to begin. These components and their relations are often referred to as a chain of infection. The major variables in the chain of infection include the agent (organism), reservoir (environment in which the agent exists and multiplies), portal of exit (route by which the agent leaves the host), transmission mode, portal of entry (route by which the agent enters the new host), and host susceptibility (internal and external environmental factors that increase or decrease the likelihood the host will develop disease). Changes in any one variable result in a change in the presence, intensity, and frequency of the entire infectious disease process.
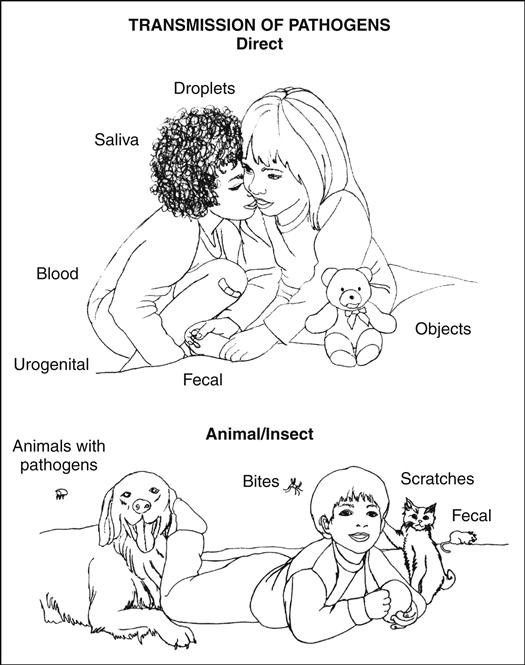
Transmission of Pathogens
Infection transmission occurs through several modes, or routes. For example, pathogens from the respiratory tract are shed through sneezing, coughing, and talking. If the pathogens survive in the air, they can infect others who inhale them (airborne route). Because this mode of transmission is relatively uncontrollable, infections can easily be spread in crowded conditions.
Pathogens may also be shed through fecal matter. When personal hygiene is poor and hand hygiene is not routinely practiced, pathogens have ample opportunities to enter through the mouth (fecal-oral transmission). Unclean hands can also contaminate food, which is then ingested.
Sexual activity involving direct mucosal contact is the most common means of transmission of sexually transmitted diseases (STDs) (direct contact transmission). If the mother’s birth canal is infected, newborn infants can be infected by direct contact during birth. Saliva is another avenue of transmission, as is direct contact with infected skin. Pathogens can also be present in breast milk and can infect a nursing infant.
A tick, mosquito, mite, or animal can inject pathogens into the skin and blood of the host. Organisms carried in this way are considered to be vector borne. For example, a certain species of mosquito carries the malaria parasite; likewise, certain bats carry the rabies microorganism.
Contamination by blood of an infected host can occur through transfusions, blood products, and the use of contaminated needles (direct inoculation). A pregnant woman can transmit such pathogens through the placenta. Other modes of transmission also exist, such as through spores found in soil (e.g., tetanus).
Epidemiologic Investigations
Epidemiology is the study of the distribution of health and illness within a population and the factors that determine the population’s health status. Nurses may not realize that they are contributing to this process when they gather patient history information as part of the nursing assessment process. The data nurses collect help the entire health care team identify, treat, and prevent disease processes as well as promote health. Moreover, the specific steps of the epidemiologic process mirror the steps in the nursing process and include defining the condition; determining the condition’s natural history; identifying critical control points; and designing, implementing, and evaluating control strategies.
Infection and Host Defenses
The first stage of infection begins with colonization of the host by the pathogen. Microorganisms invade either by adhering to tissues or by invading cells. Initially, replication of the pathogen does not cause tissue damage, and colonization can occur without development of a clinical infection. As the host “recognizes” the invasion, the defense system—the immune response—is activated. The two components of the immune response are the innate, nonspecific immune response and the adaptive, specific immune response: cell mediated and humoral (see Chapter 42).
The first lines of defense in the innate immune system are the skin and intact mucous membranes. The skin serves as a barrier, preventing colonization of most pathogens. The acid secreted in sweat and by sebaceous glands inhibits pathogenic invasion. Smooth muscle contraction and ciliary actions, such as those seen in bladder and bowel emptying and coughing and sneezing, remove pathogens mechanically. Physical and chemical barriers are provided through mucus production by goblet cells in mucous membranes. Nevertheless, the innate system may be unable to prevent the invasion. Phagocytosis, the process by which phagocytes digest and thereby destroy foreign microorganisms, can be overwhelmed. Large numbers of pathogens or their toxins can inhibit phagocytosis. When this process occurs, the adaptive immune system is activated. This system “recognizes” and responds to pathogens by destroying them. The adaptive immune system “imprints” on these pathogens so that if the body encounters them again, the response will be rapid and specific.
Immunity
Immunity is the body’s resistance to the effects of harmful agents. It occurs as an antigen-antibody reaction that takes place whenever a foreign agent or its toxins enter the bloodstream. Immunity can be either active or passive. Active immunity occurs as a result of immune system stimulation from exposure to antigens, either naturally or through vaccine administration. Passive immunity is a form of infection protection acquired through the administration of serum containing antibodies.
Some childhood diseases have been significantly reduced and some nearly eliminated through the administration of vaccines producing active or passive immunity. A variety of preparations of disease-specific vaccines and preparations can artificially accomplish active or passive immunity (see Chapter 5).
Infectious diseases are a major reason health care is sought for infants and children. Although most infections are not life threatening, fatal complications can develop, especially in infants or children with an immature or compromised immune system. Moreover, a child’s illness directly affects the family and caregivers. Absence from work for the parent of a sick child can jeopardize job security, and the accompanying missed income can be devastating for both single- and two-income families.
Nurses play a major role in preventing pediatric infectious diseases and decreasing the incidence of disability and death in both community and hospital settings. Regardless of their clinical setting, nurses must be able to confidently recognize the sometimes subtle signs and symptoms of infectious diseases in children and initiate appropriate treatment and nursing care. Nurses must also provide education about accessing appropriate community resources and limiting exposure of other children and community members.
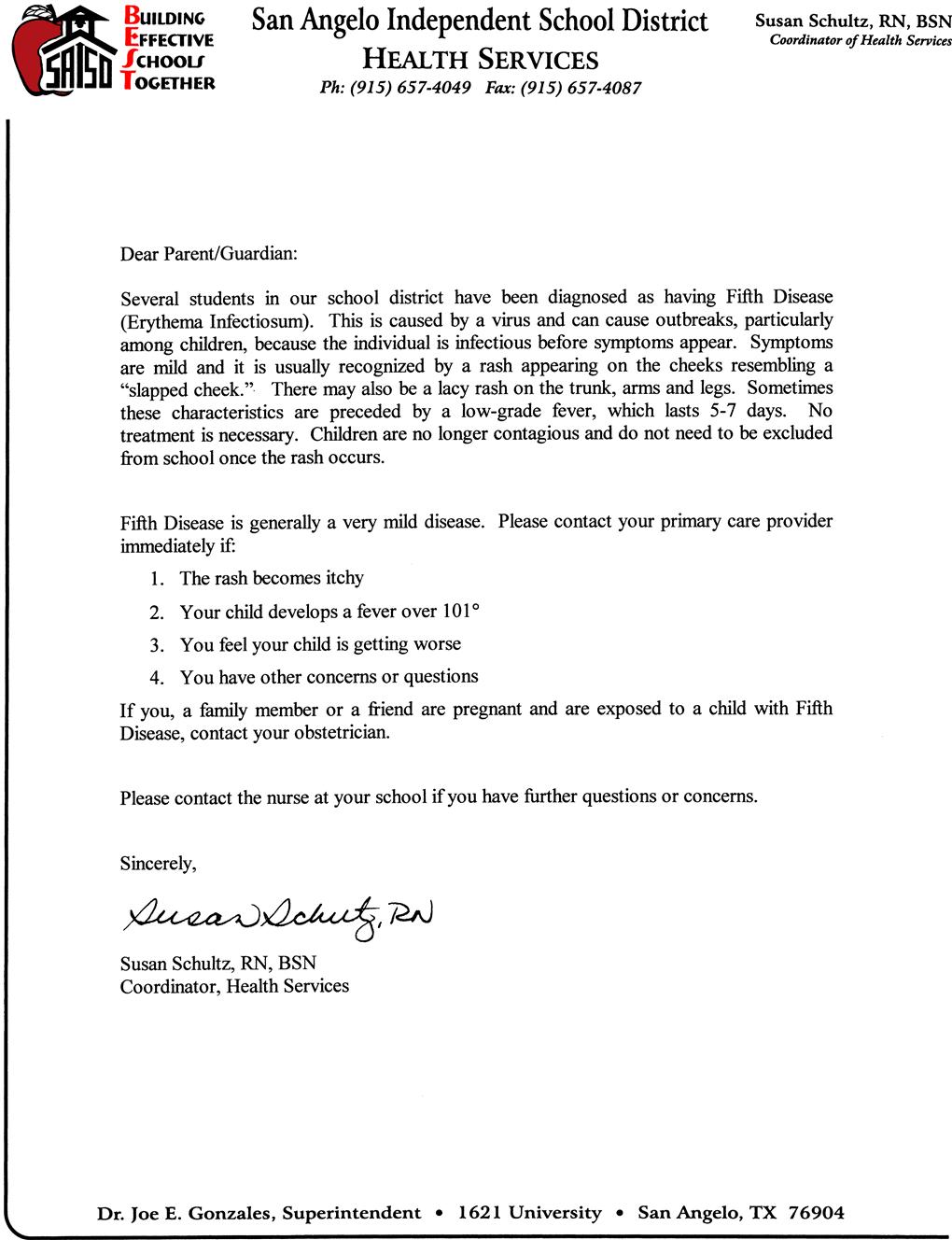
In addition, because of the growing number of uninsured and underserved children in the United States, nurses may be the first and sometimes only health care professionals to evaluate and treat children in community-based settings. School nurses are frequently required to notify parents and caregivers when their children have been exposed to infectious diseases. Figure 41-1 illustrates an example of a notification letter from a school nurse written to inform parents and caregivers about an exposure to erythema infectiosum (fifth disease). Regardless of the particular type of infection, underlying principles of nursing care are similar.
Viral Exanthems
Viruses are small parasitic organisms with unique characteristics that cause them to be quite different from other organisms. They contain only one type of nucleic acid—either deoxyribonucleic acid (DNA) or ribonucleic acid (RNA). This prevents them from reproducing on their own. Instead, a host cell is needed to allow the virus to replicate.
The replication process begins with the virus first attaching itself to a host cell. After the initial attachment, a virus must invade the interior of the cell. Replication of the virus’s nucleic material begins after the envelope and capsule (capsid) are shed and the nucleic material of the virus is released into the cell; the host cell then assists in the formation of the necessary nucleic material. New capsules are then formed and released into the host’s cells. The infected host cell can respond to the viral invasion by cell death (lysis) and destruction, or the infected cells can remain alive and continue to function while new viral particles are slowly released. This slow release occurs in an asymptomatic person who is a carrier of the virus. Some viruses are selective about the cells to which they attach. For example, the human immunodeficiency virus (HIV) prefers to attach to the T cell (see Chapter 42).
A virus can also invade a host and remain dormant until a trigger stimulates the virus to begin replicating. Many triggering factors are not fully understood. However, some triggers have been identified. An example of this triggering effect is the effect of stress in herpes simplex (a viral disease), resulting in the formation of cold sores.
Nursing Considerations for the Child with a Viral Exanthem Infection
An exanthem is an eruption or rash on the skin. Several childhood infectious diseases are characterized by rashes with distinctive characteristics. Nurses need to be aware that rashes have more than one characteristic and should obtain a detailed history of the characteristics of the rash, including its onset, initial location, and progression, as well as any associated physical signs or symptoms. Specific characteristics of the rash should be documented, including color, elevation, pattern or shape, size (in centimeters), location and distribution on the body, and any drainage. Vital signs, including temperature, should be taken and recorded. Also record the child’s general state of health, recent exposures to illnesses, and any prescribed or over-the-counter medications and treatments taken and their results. Perform a general physical assessment to look for associated signs of inflammation, which may include abnormal enlargement or tenderness of the spleen, liver, or lymph nodes.
Children with typical uncomplicated viral exanthems are usually cared for at home. Hospitalization is indicated when complications occur or the exanthema is known to be associated with severe disease. Nurses who care for hospitalized children with an infectious disease should not also care for high-risk (immunosuppressed) children to prevent any possible cross transmission by the nurse.
Whether the child is cared for in the hospital or at home, any specific isolation measures will be determined by the child’s specific infectious disease process.
Rubeola (Measles)
| Causative agent: | RNA virus |
| Incubation period: | 8 to 12 days from exposure to onset of symptoms |
| Infectious period: | Ranges from 3 to 5 days before the appearance of the rash to 4 days after appearance of the rash |
| Transmission: | Transmitted between individuals by direct contact with infectious droplets or less frequently by airborne spread |
| Immunity: | Natural disease or live attenuated vaccine |
| Season: | Late winter and spring |
Manifestations
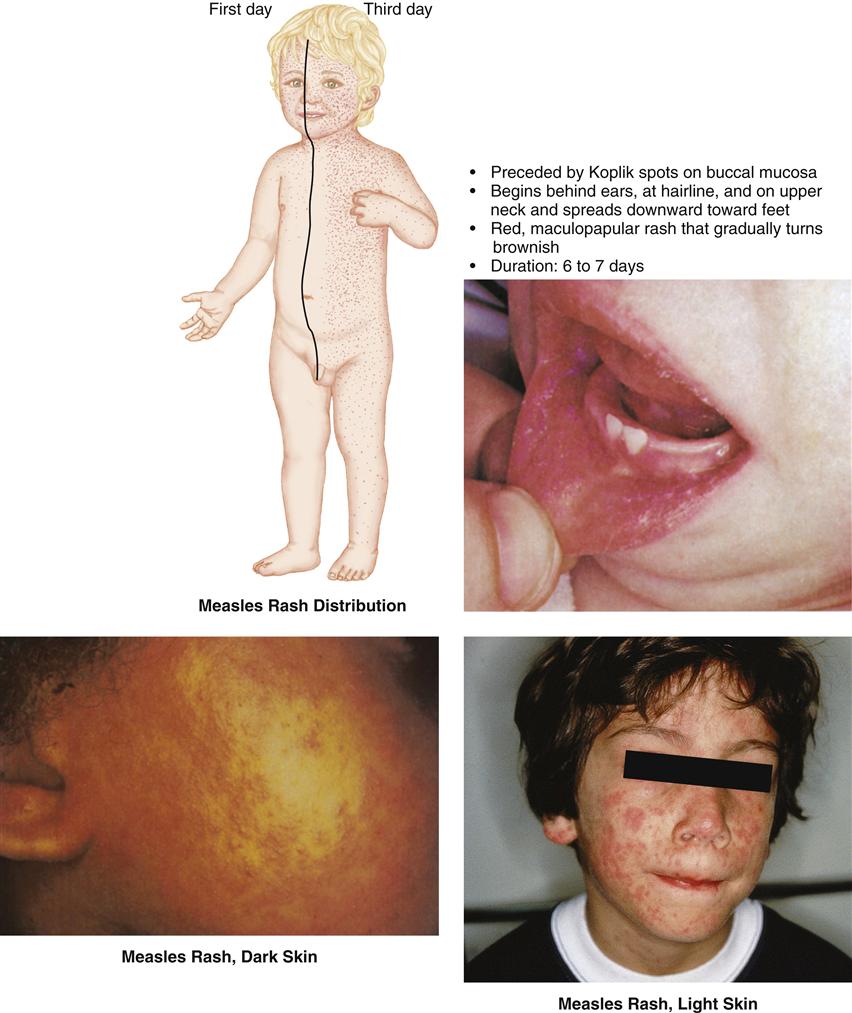
The measles virus enters the body and slowly spreads. Respiratory symptoms appear after an average of 10 days. Typically, children have a prodrome period with fever that rises gradually and the “three Cs” (coryza [profuse runny nose], cough, and conjunctivitis) that lasts between 1 and 4 days. Children are usually quite ill during this time. Koplik spots appear approximately 2 days before the appearance of the rash (Figure 41-2 on page 1014). Koplik spots are small, blue-white spots with a red base that cluster near the molars on the buccal mucosa. These spots last approximately 3 days,
after which they slough off. As prodromal symptoms reach a peak, the exanthem appears and is characterized by a deep-red, macular rash that usually begins on the face and neck and spreads down the trunk and extremities to the feet. The rash blanches easily with pressure and will gradually turn a brownish color. The duration of the rash is approximately 6 to 7 days.
A partially immune child, such as an infant younger than 9 months who has passively acquired maternal antibodies or a child given immune gamma globulin, may contract modified measles. The prodromal period is shorter and the symptoms are minimal, with few to no Koplik spots. The rash progression follows the pattern of regular measles.
Complications
Although considered a relatively rare disease since vaccine became available, approximately 10 million cases of measles occur each year, and 197,000 children die each year from the measles (Centers for Disease Control and Prevention [CDC], 2009b). Because of respiratory involvement, secondary infections such as otitis media, bronchopneumonia, and laryngotracheobronchitis (croup) can occur, especially in infants and younger children. Rarely, central nervous system (CNS) complications such as encephalitis develop during the prodromal period and can lead to long-term sequelae such as brain death. Measles can cause premature birth and miscarriage in pregnant women (Cherry, 2009c).
Therapeutic Management
The treatment of measles is symptomatic, whether the child is hospitalized or remains at home. If hospitalized, the child will require airborne isolation precautions. During the febrile period, the child should be restricted to quiet activities and bed rest. Fluids are encouraged, and humidification and antitussives are used to relieve the cough (Cherry, 2009c).
Low levels of vitamin A are associated with many measles cases and an increase in measles severity. Vitamin A deficiency is rare in the United States but is common in developing countries, causing the American Academy of Pediatrics (AAP) to recommend vitamin A supplementation in certain more severe cases of measles (Cherry, 2009c).
Children can be protected against measles and other vaccine-preventable diseases by receiving all their immunizations during their routine well-child checkups. Two doses of measles, mumps, and rubella (MMR) vaccine are required to be fully protected. The first MMR is recommended routinely at 1 year of age. The second dose of MMR is recommended at 4 to 6 years but may be administered during any visit if at least 4 weeks has elapsed since the first dose, and both doses are administered beginning at or after 12 months of age. Children who have not previously received their second MMR dose should complete the schedule no later than their 11- to 12-year health maintenance visit (CDC, 2008a).
In 2005, the U.S. Food and Drug Administration (FDA) licensed a combination measles-mumps-rubella-varicella vaccine. Recent studies reveal that there is a very slight increased risk of fever and febrile seizures 7 to 10 days after vaccination in children age 12 to 24 months compared to the separate MMR and varicella vaccines. Nurses should educate parents about the risk before vaccination (Klein, Fireman, Yih, et al., 2010).
Rubella (German Measles, 3-Day Measles)
| Causative agent: | RNA virus |
| Incubation period: | 14 to 21 days |
| Infectious period: | Ranges from 7 days before onset of symptoms to 14 days after appearance of the rash |
| Transmission: | Airborne particles or direct contact with infectious droplets, transplacental transmission; small number of infants with congenital rubella continue to shed the virus for months after birth |
| Immunity: | Natural disease or live attenuated vaccine |
| Season: | Late winter and early spring |
Manifestations
Rubella is usually a mild disease for children and adults. The virus enters the host, producing a rash after approximately 14 to 16 days. Young children are often asymptomatic until the appearance of the rash. Older children may report profuse nasal drainage, diarrhea, malaise, sore throat, headache, low-grade fever, polyarthritis, eye pain, aches, chills, anorexia, and nausea. Children of all ages usually have impressive posterior cervical, posterior auricular, and occipital lymphadenopathy.
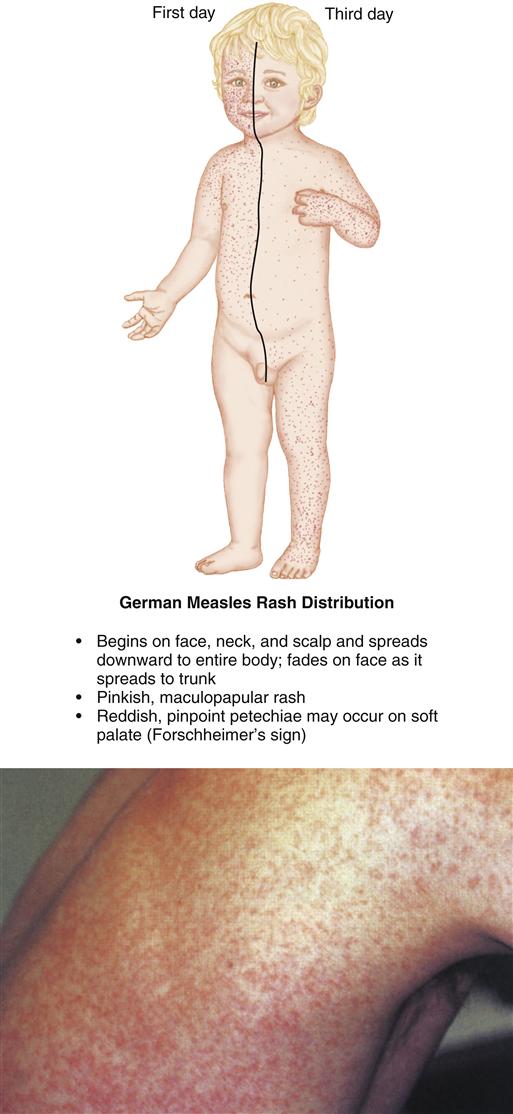
The rash manifests as a pinkish rose maculopapular exanthem that begins on the face, scalp, and neck (Figure 41-3). It spreads downward to include the entire body within 1 to 3 days. As the rash spreads to the trunk, the rash on the face begins to fade. Petechiae (spots), which are red or purple color and pinpoint in size, may occur on the soft palate. Their appearance is sometimes referred to as Forchheimer’s sign.
Complications
The availability of rubella vaccine has effectively eliminated rubella in the United States (CDC, 2010d). Rubella has relatively few complications. The most common are arthritis and arthralgia, which occur more often in adult women than in children or adolescents. Mild thrombocytopenia may also occur but is usually self-limiting and of short duration. A rare complication is encephalitis, which is usually less severe than measles-related encephalitis.
The importance of recognizing and respecting this viral illness is not the morbidity of the disease itself but rather the consequences that can occur to a fetus during maternal infection. The most devastating form of rubella is congenital rubella that occurs after maternal infection, usually during the first 12 weeks of pregnancy. One of the most common manifestations of congenital rubella is intrauterine growth retardation. These infants typically weigh less than 2500 g and continue to have failure to thrive in infancy. Mortality is highest during the first year. Common causes of death include pneumonia, heart defects, encephalitis, and immune deficiency (Cherry, 2009g).
Therapeutic Management
Treatment is generally supportive and symptomatic, with the disease being self-limiting. Recommendation for exclusion of affected children from school or child care is 7 days after the rash begins. Infants with congenital rubella are presumed contagious until age 1 year or nasopharyngeal and urine cultures for the rubella virus are repeatedly negative. Primary prevention of rubella can be accomplished through administration of the rubella vaccine in combination with measles and mumps vaccine (MMR), as previously discussed.
Erythema Infectiosum (Fifth Disease, Parvovirus B19)
| Causative agent: | Parvovirus B19 |
| Incubation period: | 4 to 14 days but can be up to 21 days |
| Infectious period: | Shedding of virus occurs between days 5 and 12 of the infection; usually from the prodromal period until the rash appears |
| Transmission: | Airborne particles, respiratory droplets, blood, blood products, transplacental transmission |
| Immunity: | Natural disease is thought to provide antibodies for immunity |
| Season: | Winter and spring |
This disease is most common in children ages 5 to 14 years but may also occur in adults.
Manifestations
Fifth disease is a relatively mild systemic disease. Typically the child may appear well but has an intense, fiery red, edematous rash on the cheeks, which gives a “slapped cheek” appearance (Figure 41-4), or a history of a rash that “comes and goes.” Before the appearance of the rash, many children are asymptomatic or have nonspecific symptoms such as headache, runny nose, malaise, and mild fever. Approximately 1 to 4 days after the facial rash appears, an erythematous, maculopapular rash appears on the trunk and extremities. The rash fades with a central clearing area, resulting in a lacy appearance. The rash may last 2 to 39 days and reappear when aggravated by environmental factors, such as heat, exercise, warm baths, rubbing of the skin, and stress.
Complications
Because the disease is mild, complications are not usually reported, especially in children. Patients with sickle cell disease or beta-thalassemia are at risk for anemia and aplastic crisis. Patients with a poor immune system are also at risk for anemia. Because pregnant women are at risk for intrauterine infection, the nurse should obtain a careful history, with an emphasis on identifying any pregnant family members, teachers, or friends to prevent intrauterine infection and fetal death. Many school districts notify pregnant staff if they have been exposed to a child with fifth disease and recommend that they contact their health care provider. Parvovirus B19 occurs in approximately 1 in 400 pregnancies. There is a 15% increase in the risk of miscarriage if infected in the first 20 weeks of pregnancy (Duncan, 2008).
Therapeutic Management
The disease is generally benign and self-limiting. Treatment is symptomatic and supportive.
Roseola Infantum (Exanthem Subitum)
| Causative agent: | Human herpesvirus 6 (HHV-6) |
| Incubation period: | Unknown but estimated to be 9 to 10 days |
| Infectious period: | Unknown but thought to extend from the febrile stage to the time the rash first appears |
| Transmission: | Most likely by contact with secretions (saliva, cerebrospinal fluid [CSF]) of asymptomatic close contacts |
| Season: | Throughout the year without a distinctive seasonal pattern |
Manifestations
HHV-6 appears to be the major causative agent, although other viruses have been implicated as well. Most clinical cases of roseola occur in children 6 to 18 months old. The child has a sudden high fever (103° F to 106° F [39.4° C to 41.1° C]), malaise, and irritability but may remain active and alert. An intermittent or constant fever may persist for 3 to 5 days. The child may also have a mild cough, runny nose, abdominal pain, headache, vomiting, and diarrhea (Shelov, 2010). After 3 to 5 days, the fever subsides, and within several hours to 2 days, a rash appears. The rash consists of rose-pink maculopapules or macules that blanch with pressure (Figure 41-5). The rash occurs predominantly on the neck and trunk and may be surrounded by a whitish ring. It normally persists for 24 to 48 hours before fading.
Complications
Complications associated with roseola are uncommon. Febrile seizures (see Chapter 52) may occur.
Therapeutic Management
Treatment is symptomatic. Family members should be taught about fever control and management.
Antipyretic medications, decreased clothing, cooler environmental temperatures, and increased fluid intake all assist with fever control. Temperature monitoring, medication administration (prescription and over-the-counter medications), and other comfort measures should be discussed. The nurse verifies that the child’s family has access to a thermometer and knows how to use it. In addition, parents should be given information regarding the absolute avoidance of any form of aspirin (including over-the-counter medications containing salicylates) because of the potential risk of developing Reye’s syndrome (see Chapter 52). Anticipatory guidance should include alerting the parent to the possibility of febrile seizures and teaching about seizure precautions (especially if the child has a history of previous febrile seizures).
Parents’ understanding of the care necessary for their child is important, particularly measures to control and prevent the spread of infection. Teach the parents how to recognize the signs and symptoms of complications so they can seek medical treatment when warranted. Providing parents with written instructions that they can refer to at home may prove helpful.
Enterovirus (Nonpolio) Infections (Coxsackieviruses, Group A and Group B), Echoviruses, and Enteroviruses
| Causative agents: | RNA viruses including 23 group A coxsackieviruses (types A1 to A24, except type A23), six group B coxsackieviruses (types B1 to B6), 31 echoviruses (types 1 to 33, except types 10 and 28), and four enteroviruses (types 68 to 71) |
| Incubation period: | Usually 3 to 6 days |
| Infectious period: | Unknown, but fecal viral excretion and transmission can continue for several weeks after the onset of infection |
| Transmission: | Spread by fecal-oral and possibly by oral-oral (respiratory) routes |
| Season: | In temperate climates infections are most common in the summer and fall, but no seasonal pattern is evident in the tropics |
Manifestations
Common presentations in both infants and children include nonspecific febrile illnesses with a wide variety of respiratory, gastrointestinal, cardiac, neurologic, skin, oral, and eye signs and symptoms.
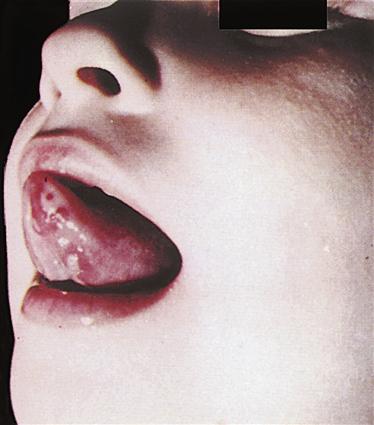
A frequently seen pattern of illness in young children is hand-foot-and-mouth disease, caused by coxsackievirus A16 or other enteroviruses. Inflammation and lesions in the mouth (Figure 41-6), on the palms of the hands, and on the soles of the feet are the hallmarks of this syndrome, along with mild fever; some children experience small lesions on the buttocks (Schmitt, 2010). Lesions become vesicular over the course of several days and usually resolve by 1 week. If lesions are particularly widespread in the oropharynx, the child may refuse to eat or drink; the potential for dehydration exists in very young children.
Complications
Although each of these groups of symptoms can be associated with different enteroviruses, complications can occur from specific strains. Young infants with a history of prematurity are at higher risks for complications and death. Serious complications such as myocarditis, hepatitis, and encephalitis are often the cause. Mortality rates are highest for coxsackievirus B and lowest for coxsackievirus A (Cherry, 2009b).
Therapeutic Management
Currently, no specific therapy exists for enteroviral infections, but clinical trials are evaluating the effectiveness of pleconaril for neonates with severe disease (Cherry, 2009b). However, enteric Contact Precautions are indicated for any affected hospitalized infant or child. Parents and caregivers should be given educational information regarding the importance of hand hygiene and personal hygiene, especially after diaper changes and trips to the bathroom.
Management of hand-foot-and-mouth disease is symptomatic. The parent can provide comfort and pain relief with acetaminophen and frequent administration of cool liquids. Milk-based ice cream is especially palatable. Extensive oropharyngeal lesions that prevent adequate oral intake can be treated with a salt and water mouth rinse or a topical solution of equal parts lidocaine gel, diphenhydramine liquid, and a liquid antacid (mixed by prescription) either applied directly to lesions or used as a mouthwash.
Nursing Considerations
The nurse needs to obtain a detailed history of the onset of symptoms with a focused assessment on the particular body systems involved. Children with an enterovirus infection can be challenging because of the wide variety and degree of signs and symptoms. Supportive care is similar to that of any child with a viral exanthem. Parents and caregivers should be given educational information about disease transmission, school or daycare attendance policies, and any available community resources (sick-child care).
Varicella-Zoster Infections (Chickenpox, Shingles)
| Causative agent: | Varicella-zoster virus |
| Incubation period: | 10 to 21 days |
| Infectious period: | 1 to 2 days before the onset of rash until all lesions are dried (crusted over), usually 5 to 7 days |
| Transmission: | Direct contact, droplet, airborne particles |
| Immunity: | Natural disease of varicella; same virus causes zoster, and child may contract zoster at a later time; varicella vaccine |
| Season: | Late winter through early spring |
Primary infection with the varicella-zoster virus causes chickenpox. Prior to 1995, when the vaccine became available, chickenpox was one of the most common childhood diseases in children 5 to 9 years old. Approximately 4 million cases of varicella and 100 deaths occurred each year in the United States (Freed, 2009). Zoster (shingles), which is the reactivation of the latent varicella-zoster virus, occurs most frequently in the elderly population but can occur in children as well, especially adolescents and young adults. Generally varicella and zoster in children are not life threatening.
Manifestations
Varicella
During the 24 to 48 hours before the appearance of lesions, symptoms may include a slightly elevated body temperature, malaise, and anorexia. A rash generally first appears on the trunk and scalp (Figure 41-7), followed by the appearance of lesions, which quickly become teardrop vesicles with an erythematous base. The vesicles then become pustular, after which they begin to dry and develop a crust. The lesions appear in crops over the course of usually 3 to 4 days and can be seen to be in different stages of development. The number of lesions varies from child to child, but children in the household with secondary cases generally have more extensive rashes than does the child with the primary case. The lesions may appear on the mucous membranes in the mouth, genital area, and rectum. Second attacks are rare and are more common in immunocompromised children. Breakthrough attacks in immunized children are also rare, and the disease presentation is mild, with few lesions (Martin, Güris, Chaves, et al., 2007).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree