The Child with a Musculoskeletal Alteration
Learning Objectives
After studying this chapter, you should be able to:
• Identify characteristic assessments that indicate alterations in musculoskeletal function.
• State appropriate nursing diagnoses for children with an alteration in musculoskeletal function.
• Summarize the treatment modalities used to manage the child with a musculoskeletal alteration.
![]()
http://evolve.elsevier.com/McKinney/mat-ch
Clinical Reference
Review of the Musculoskeletal System
The nursing care for a child with a musculoskeletal alteration requires an understanding of the structure and function of the musculoskeletal system, comprehension of growth and development, and an awareness of the differences of the musculoskeletal system of infants and children as compared to adults.
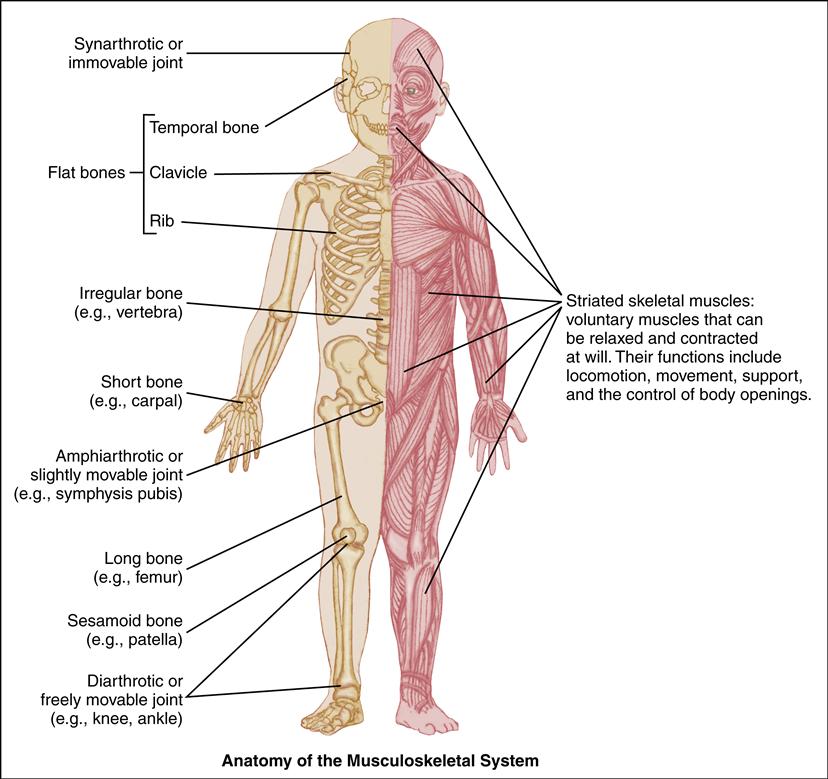
Skeletal System
The musculoskeletal system is composed of bones attached to joints, joints connected by ligaments, muscles supported by tendons, and cartilaginous tissues. The function of this system is to provide a skeletal framework to support the body, protect vital organs, and provide movement. It also supplies a storage space for the blood cell production and minerals responsible for regulating resorption and reformation of itself, as well as regulation of mineral and hormonal imbalances in the body (Porth, 2011).
Newborns are born with more bones than adults have, because cranial bones and other small bones, such as bones in the coccyx or sacrum, fuse during infancy and childhood, resulting in the adult complement of 206. The newborn’s skeletal structure is mostly cartilaginous at birth, then evolves and
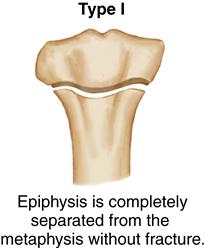
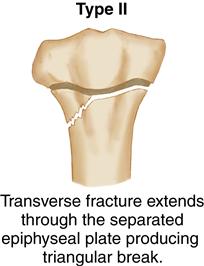
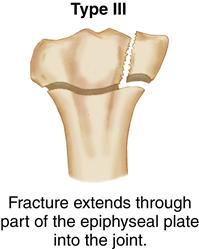
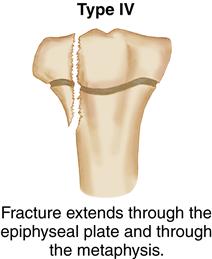
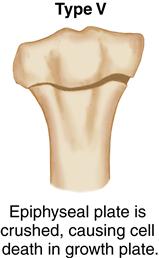
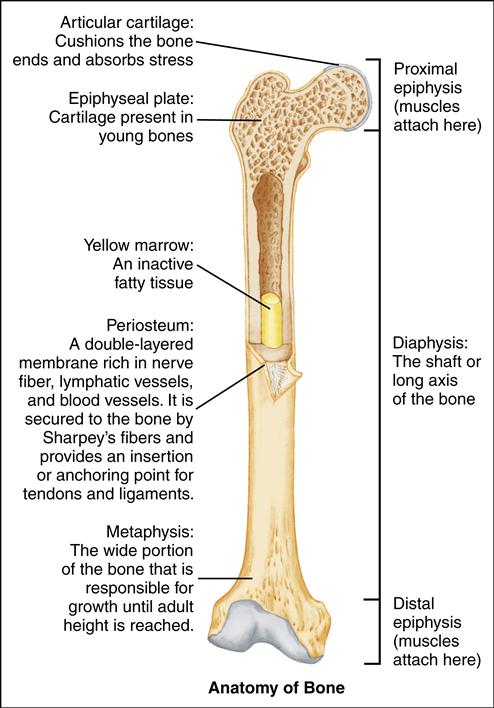
ossifies through osteogenesis. There are two distinct types of ossification: intramembranous and endochondral ossification. Intramembranous ossification is the process in which osteoblasts form bone without the cartilaginous stage (Staheli, 2008). Endochondral ossification occurs when the mesenchyme differentiates to cartilage, and cartilage then transforms into bone within primary and secondary ossification centers. Primary ossification occurs in the diaphysis (center of the bone), whereas secondary ossification occurs at the epiphysis (end of the bones). The physis, or growth plate, is formed between the primary and secondary ossification center and allows for longitudinal growth of long bones (Staheli, 2008; Texas Scottish Rite Hospital for Children [TSRHC], 2008). The growth plate absorbs shock and protects the joint surfaces from serious fractures. The metaphysis (above the growth plate) is composed mostly of cartilage and is the area that grows between the diaphysis and epiphysis to form solid bone in adulthood. It is imperative to know the location and the function of these sites of the bone, as these are often the primary sites where infection, neoplasm, fractures, and metabolic and endocrine disorders are identified (Staheli, 2008).
The periosteum is a vascular connective tissue that lines the outer surface of all bones. It has receptor nerve endings, making it sensitive to manipulation (TSRHC, 2008). The periosteum contributes to bone development by appositional bone growth and has the capability to heal fractures and regenerate bone rapidly in children.
There are five classifications of bones: long bones, such as the femur; short bones, such as the carpals; irregular bones, such as the vertebrae; flat bones, such as the ribs; and sesamoid (sometimes classified as short) bones, such as the patella. There are also two major divisions to the skeletal system: the axial skeleton, which forms longitudinally and includes the vertebral column and the skull; and the appendicular system, which is attached to the axial and encompasses the pelvis, pectoral girdle, and upper and lower extremities (Porth, 2011).
Articular System
Joints, which are composed of connective tissue and cartilage, connect two or more bones to one another and enable movement. Joints are classified by structure, function, and movement. In general, joints are identified as synarthrotic or immovable (e.g., the skull), or synovial (diarthrotic), which are freely movable (e.g., the hip) (Porth, 2011).
Alterations in joint movement and swelling require further evaluation. Defective joints are often seen in children with
neuromuscular disorders, such as spina bifida and arthrogryposis (Staheli, 2008; TSRHC, 2008). Alterations in joint movement and swelling can also be indicative of trauma, infection, or arthritis.
Muscular System
Muscles help stabilize joints and maintain contact between articular surfaces. Skeletal muscles are attached by tendons to bones. Ligaments bind one bone firmly to another, and the joints are further stabilized by the overlying tendons and muscles. The shape of the two ends of each muscle and of the joint determines the extent of movement or articulation. Skeletal muscles, which are composed of elongated fibers, function voluntarily and produce movement by contraction. Muscle disease in children presents as muscle weakness, spasticity, myoclonus, and myalgia (Staheli, 2008).
Cartilage
Cartilage is dense connective tissue that develops at the epiphysis and is capable of withstanding considerable tension. During early fetal development, the skeletal structure is composed mostly of cartilage. In time it will largely convert to bone by ossification. Connective tissue is made up of collagen and proteoglycans (Staheli, 2008). Deficiencies in connective tissues are associated with Marfan syndrome and osteogenesis imperfecta (TSRHC, 2008).
Growth and Development
Knowledge of normal growth and development is essential when assessing, caring for, and evaluating the pediatric patient’s musculoskeletal system. Infants experience the greatest growth rate. During childhood, growth slows and then increases rapidly again in adolescence with peak height velocity. Peak height velocity is the maximum growth that occurs during puberty. Growth in the length of the long bones continues at the epiphysis until adult height is reached (see Chapter 9).
Children should be weighed and measured for length or stature with each visit. The results of these measurements should consistently and correctly be plotted on appropriate growth and development graphs in order to be aware of any variations in height or weight (see Chapter 33). Extreme variations in height and weight can impact the child’s overall state of health. Childhood obesity, for example, can have a direct effect on children with musculoskeletal problems, such as tibia vara, Blount disease, and slipped capital femoral epiphysis (TSRHC, 2008).
A basic understanding of when children meet their major developmental milestones, especially for gross motor development, is crucial when assessing and treating the child with an alteration of the musculoskeletal system. Failure to meet these milestones in a timely manner may be indicative of hypotonia, cerebral palsy (hemiplegic), or a neuromuscular disorder. See Chapters 6 through 9 for developmental milestones in children of various developmental levels.
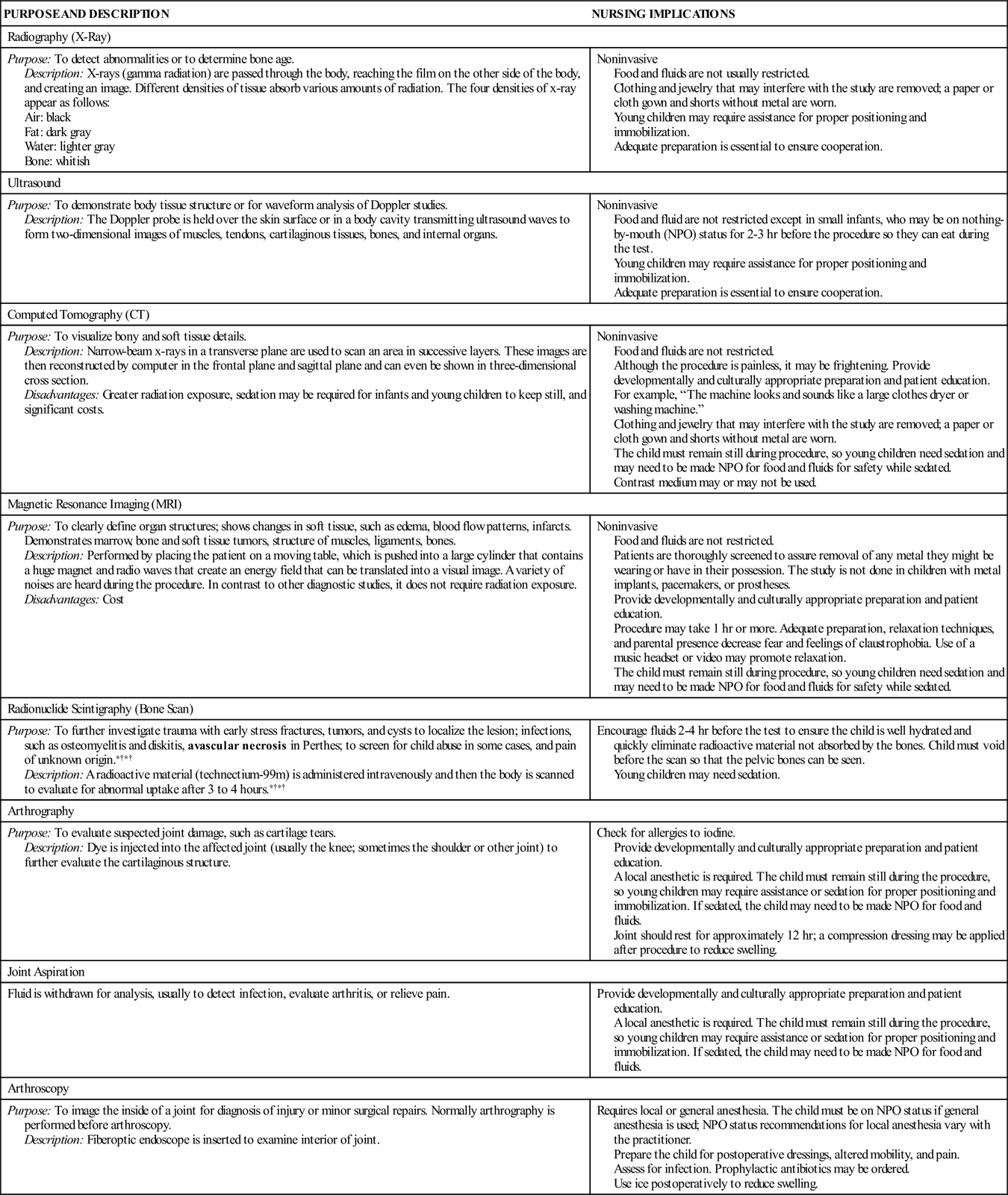
Diagnostic and Laboratory Tests
Radiographs are the mainstay of an orthopedic evaluation. They provide important diagnostic evaluation after a clinical assessment when there is concern of a musculoskeletal abnormality. Studies have shown risks of cancer with radiation exposure in a growing child (Brody, Frush, Huda, et al., 2007; Gacca, 2008). Several recommendations have been formulated to protect the child. Radiologists and technicians are to use the least and most diagnostically effective radiation exposure on children. In addition, care needs to be taken to shield the gonads, make sure the patient is placed in the correct anatomic position, avoid routine opposite-side radiographs, take single radiographs instead of multiple views, and consult as needed with the provider ordering the x-rays (Brody et al., 2007; Gacca, 2008). It is important to note the pediatric differences in plain films as compared to adults, because the differences can lead to misinterpretation and over- or undertreatment. For example, children have open growth plates at the proximal and distal aspects of the long bones that can easily be confused for fractures. Furthermore, a periosteal reaction in the diaphysis after trauma or infection can be misinterpreted as normal (Staheli, 2008).
COMMON DIAGNOSTIC PROCEDURES FOR MUSCULOSKELETAL DISORDERS IN CHILDREN
| PURPOSE AND DESCRIPTION | NURSING IMPLICATIONS |
| Radiography (X-Ray) | |
| Purpose: To detect abnormalities or to determine bone age. Description: X-rays (gamma radiation) are passed through the body, reaching the film on the other side of the body, and creating an image. Different densities of tissue absorb various amounts of radiation. The four densities of x-ray appear as follows: | Noninvasive Food and fluids are not usually restricted. Clothing and jewelry that may interfere with the study are removed; a paper or cloth gown and shorts without metal are worn. Young children may require assistance for proper positioning and immobilization. Adequate preparation is essential to ensure cooperation. |
| Ultrasound | |
| Purpose: To demonstrate body tissue structure or for waveform analysis of Doppler studies. Description: The Doppler probe is held over the skin surface or in a body cavity transmitting ultrasound waves to form two-dimensional images of muscles, tendons, cartilaginous tissues, bones, and internal organs. | Noninvasive Food and fluid are not restricted except in small infants, who may be on nothing-by-mouth (NPO) status for 2-3 hr before the procedure so they can eat during the test. Young children may require assistance for proper positioning and immobilization. Adequate preparation is essential to ensure cooperation. |
| Computed Tomography (CT) | |
| Purpose: To visualize bony and soft tissue details. Description: Narrow-beam x-rays in a transverse plane are used to scan an area in successive layers. These images are then reconstructed by computer in the frontal plane and sagittal plane and can even be shown in three-dimensional cross section. Disadvantages: Greater radiation exposure, sedation may be required for infants and young children to keep still, and significant costs. | Noninvasive Food and fluids are not restricted. Although the procedure is painless, it may be frightening. Provide developmentally and culturally appropriate preparation and patient education. For example, “The machine looks and sounds like a large clothes dryer or washing machine.” Clothing and jewelry that may interfere with the study are removed; a paper or cloth gown and shorts without metal are worn. The child must remain still during procedure, so young children need sedation and may need to be made NPO for food and fluids for safety while sedated. Contrast medium may or may not be used. |
| Magnetic Resonance Imaging (MRI) | |
| Purpose: To clearly define organ structures; shows changes in soft tissue, such as edema, blood flow patterns, infarcts. Demonstrates marrow, bone and soft tissue tumors, structure of muscles, ligaments, bones. Description: Performed by placing the patient on a moving table, which is pushed into a large cylinder that contains a huge magnet and radio waves that create an energy field that can be translated into a visual image. A variety of noises are heard during the procedure. In contrast to other diagnostic studies, it does not require radiation exposure. Disadvantages: Cost | Noninvasive Food and fluids are not restricted. Patients are thoroughly screened to assure removal of any metal they might be wearing or have in their possession. The study is not done in children with metal implants, pacemakers, or prostheses. Provide developmentally and culturally appropriate preparation and patient education. Procedure may take 1 hr or more. Adequate preparation, relaxation techniques, and parental presence decrease fear and feelings of claustrophobia. Use of a music headset or video may promote relaxation. The child must remain still during procedure, so young children need sedation and may need to be made NPO for food and fluids for safety while sedated. |
| Radionuclide Scintigraphy (Bone Scan) | |
| Purpose: To further investigate trauma with early stress fractures, tumors, and cysts to localize the lesion; infections, such as osteomyelitis and diskitis, avascular necrosis in Perthes; to screen for child abuse in some cases, and pain of unknown origin.∗† Description: A radioactive material (technectium-99m) is administered intravenously and then the body is scanned to evaluate for abnormal uptake after 3 to 4 hours.∗† | Encourage fluids 2-4 hr before the test to ensure the child is well hydrated and quickly eliminate radioactive material not absorbed by the bones. Child must void before the scan so that the pelvic bones can be seen. Young children may need sedation. |
| Arthrography | |
| Purpose: To evaluate suspected joint damage, such as cartilage tears. Description: Dye is injected into the affected joint (usually the knee; sometimes the shoulder or other joint) to further evaluate the cartilaginous structure. | Check for allergies to iodine. Provide developmentally and culturally appropriate preparation and patient education. A local anesthetic is required. The child must remain still during the procedure, so young children may require assistance or sedation for proper positioning and immobilization. If sedated, the child may need to be made NPO for food and fluids. Joint should rest for approximately 12 hr; a compression dressing may be applied after procedure to reduce swelling. |
| Joint Aspiration | |
| Fluid is withdrawn for analysis, usually to detect infection, evaluate arthritis, or relieve pain. | Provide developmentally and culturally appropriate preparation and patient education. A local anesthetic is required. The child must remain still during the procedure, so young children may require assistance or sedation for proper positioning and immobilization. If sedated, the child may need to be made NPO for food and fluids. |
| Arthroscopy | |
| Purpose: To image the inside of a joint for diagnosis of injury or minor surgical repairs. Normally arthrography is performed before arthroscopy. Description: Fiberoptic endoscope is inserted to examine interior of joint. | Requires local or general anesthesia. The child must be on NPO status if general anesthesia is used; NPO status recommendations for local anesthesia vary with the practitioner. Prepare the child for postoperative dressings, altered mobility, and pain. Assess for infection. Prophylactic antibiotics may be ordered. Use ice postoperatively to reduce swelling. |
Clinical laboratory tests are also useful in evaluating the patient with a suspected musculoskeletal alteration. Nurses must have a baseline comprehension of what the normal laboratory values are for each study to inform and educate the family about the results. Fasting is not required for these studies.
The hematology workup in orthopedics includes a complete blood count with a differential, C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR) for musculoskeletal conditions such as growing pains, bone pain, stress fractures, hip pain, back pain, and infection (Staheli, 2008; TSRHC, 2008). CRP is a protein that appears in blood during an inflammatory process and is not seen in healthy people. The measurement is nonspecific, merely indicating the presence of inflammation. ESR is the rate at which erythrocytes settle out of unclotted blood, measured in millimeters per hour. Inflammation and necrotic problems cause an elevation in ESR levels.
Chemistry labs assist in the evaluation for metabolic conditions, such as rickets (TSRHC, 2008). These labs include studies of calcium, alkaline phosphatase (ALP), and phosphorus. ALP is an enzyme found mainly in bone, liver, placenta, and kidney. Levels may be elevated in bone disease, fractures, trauma, or liver disease and during periods of rapid growth. Determinations may be ordered to differentiate between bone and liver problems.
Enzyme studies such as creatine phosphokinase (CPK) may be ordered. CPK is an enzyme found in heart and skeletal muscle; the CPK assay is a specific test for assessing cardiac and muscle damage. Levels are elevated in trauma, myocardial infarction, and muscular dystrophy. Determinations may be ordered to differentiate between cardiac (MB) and skeletal (MM) CPK.
Rheumatoid factor (RF) and a hematology workup are used to evaluate juvenile idiopathic arthritis (Staheli, 2008). RFs are antibodies that may be responsible for the destructive changes associated with rheumatoid arthritis. A positive RF with an elevated CRP and ESR can be indicative of arthritis in children; however, RF is positive in only 5% of these cases (Staheli, 2008).
Musculoskeletal problems affect muscles, bones, joints, and tendons, all of which are necessary for movement and therefore are critical to a child’s development. Many musculoskeletal problems occur because of vigorous motor activities that are part of a child’s daily life, but the rapid growth of the skeletal system also plays a significant role. Most musculoskeletal problems are short term, but a number of chronic musculoskeletal conditions require long-term treatment and nursing assistance.
The child with a musculoskeletal alteration presents a unique opportunity for nursing care. A general knowledge of the structure and function of the system is required to understand the rationale for the alteration. An awareness of normal versus abnormal growth and development patterns is necessary in order to recognize delays, variations, and medical conditions. An appreciation of the musculoskeletal differences exhibited in the pediatric patient in comparison to the adult is also essential. Nurses should be familiar with the various diagnostic imaging procedures used to assist in the evaluation of patients with musculoskeletal alterations in order to implement nursing considerations. Knowledge of normal laboratory values commonly ordered for patients with musculoskeletal conditions is vital for providing prudent, good-quality, and effective nursing care.
Casts, Traction, and Other Immobilizing Devices
Immobilizing a bone or joint helps achieve and maintain a more functional position or rests and protects an affected area during bone healing. Because many musculoskeletal problems require the application of an immobilizing device, the nurse needs to understand general principles of care.
Splints
Splints are used to stabilize and protect or rest an affected area, increase range of motion and function, and decrease pain (TSRHC, 2008). Splints are fabricated of fiberglass, plaster of Paris, metal, or thermoplastic polymers. Splint materials are chosen for drapability, durability, softness, setup time, thickness, capacity for remolding, and color. Splinting may be a safe, effective, and cost-saving alternative to casting for some conditions (Firmin & Crouch, 2009).
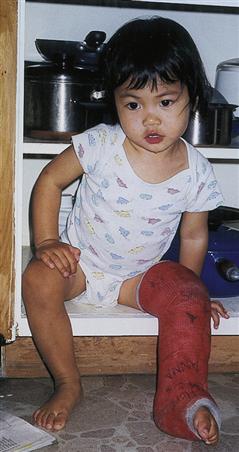
Casts
A cast provides support and maintains anatomic position for bone healing or aids in correction of a deformity. Casts may also be used to ensure adherence to treatment protocols or to protect a wound. The age and size of the child, fracture or injury, type of surgery, and amount of weight bearing the extremity can tolerate dictate the type and size of the cast.
Casts are made of synthetic materials, such as fiberglass, semirigid nonfiberglass (soft cast), or plaster of Paris (Bakody, 2009). Casting material comes in varied colors and patterns; casts can be wrapped and decorated to appeal to young children. The following equipment is needed for cast application:
• Tubular gauze/stockinette (optional)
• Waterproof lining (optional)
• Cotton under-cast padding material (e.g., Webril)
• Casting material, fiberglass and/or plaster of Paris (rolls and/or strips/splints)
• Water (clarify water temperature with professional applying cast)
• Moleskin
• Scissors
Cast application is usually done by the physician and another trained person, one to hold the extremity in correct alignment and one to apply the cast. It is very important not to move the affected area to be casted while applying the cast. Waterproof liner or stockinette is applied if desired. Waterproof linings for casts have been shown to be as effective as cotton lining for immobilization (Robert, Jiang, & Khoury, 2011). A thin layer of Webril is then applied over the initial lining. The material is rolled in a spiral fashion around the affected area, overlapping each layer by approximately 50%. Additional padding may be placed over bony prominences, making sure there are no wrinkles in any layer. Any wrinkles in the cast padding or cast material become “set” into the cast and may cause skin breakdown. Next, the casting material is dipped in water and applied over the cotton padding, making sure to leave a cotton edge at the top and bottom of the cast for patient comfort and to maintain skin integrity. A chemical reaction between casting material and water makes it feel warm and causes it to harden. The cast should not be covered while warm to prevent a possible burn.
Rough edges of casts must be trimmed to prevent injury. Petaling of cast edges with moleskin or latex-free tape decreases irritation and breakdown of adjacent skin and protects the edges of the cast from excessive wear.
Fiberglass casts dry quickly, usually set within 30 minutes of application. Fiberglass should be rolled on the affected body part without stretching the fiberglass. Fiberglass is less forgiving when swelling is expected, and if the fiberglass is pulled “tight” or stretched during application, neurovascular status may be compromised (TSRHC, 2008).
Fiberglass casts are lighter weight and more durable than plaster (TSRHC, 2008) (Figure 50-1). Fiberglass casts are water-resistant, so the hard outer shell will not break down in water; however, the padding underneath the cast material is likely cotton and will absorb and hold water. Therefore, if a fiberglass cast becomes wet, inadequate airflow under the cast will prevent thorough drying of the padding and skin. Damp skin is more susceptible to skin breakdown and infection.
Plaster casts may be used when the physician wants to “mold” the cast to apply corrective forces to a body part, such as in the treatment of a clubfoot or early onset scoliosis (TSRHC, 2008). Plaster casts will set within 10 to 15 minutes, but will not fully dry for 24 to 48 hours. Plaster is not water resistant and will break down if it gets wet.
Traction
Effective immobilization may also be achieved with traction. Traction is a pull or force exerted on one part of the body. Traction can be applied to the skin or the bone. For treatment, traction may be applied to the spine, pelvis, or long bones of the upper and lower extremities. The angle formed by the placement of the pulley and the angle of the involved joint determine the direction of the pull or force. Once the direction of the pull or force has been determined, the traction is directed along the long axis of the bone.
An opposing pull or force (countertraction) must be provided at the same time if the traction is to be effective. Countertraction results in a two-way pull that maintains alignment of the affected extremity. The child’s weight is usually sufficient to provide the countertraction. If body weight is not sufficient, additional weights may be used. Depending on the age of the child, restraining devices may be needed to maintain countertraction. Some forms of traction, such as halo traction used for cervical spine injury, exert a force without the use of weights.
If traction is being applied while the child is in bed, the part of the bed that holds the traction apparatus is tilted or elevated, thereby assisting with countertraction. For example, if the leg were being placed in traction, the foot of the bed would be elevated. Otherwise, the child would slide in the direction of the traction, disrupting the alignment of the extremity and reducing the effectiveness of treatment. Also, the mattress should be firm, and a foot board or foot plate may be necessary to keep the extremity in the correct position.
Traction can be described as either continuous or intermittent. Continuous traction exerts a constant pull and is used for fractures and dislocations. Intermittent traction provides a periodic pull or force and is used for contractures, low back pain, or muscle spasm. The nurse should always assume that traction is continuous unless the physician states otherwise. The removal of traction intended to be continuous could prove harmful to the child. If the force of the traction is altered, the muscles contract and fracture alignment could be disrupted. The tissues around the fracture could also be injured, resulting in poor healing. The nursing care plan should always reflect the frequency and amount of time intermittent traction may be removed. When removing the traction apparatus, the nurse must maintain manual traction and pull on the body part.
The disadvantages of traction include prolonged immobility and the potential need for hospitalization. Currently, early casting and percutaneous pinning are replacing the use of traction for some musculoskeletal conditions (Gosselin, Heitto, & Zirkle, 2009; Hsu, Diaz, Penaranda, et al., 2009).
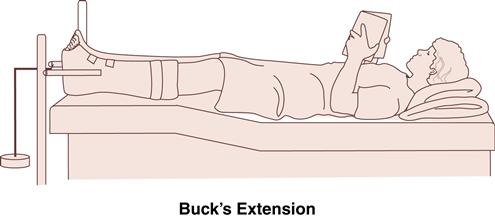
Skin Traction
Skin traction (Box 50-1) is noninvasive and well tolerated, and application does not require anesthesia (TSRHC, 2008). Skin traction is most effective with children who weigh less than 15 kg (33 lb) or are younger than 2 to 3 years. It can be applied to the pelvis, spine, or extremities (usually the long bones). Skin traction is preferred for conditions in which invasive procedures are contraindicated, such as hemarthrosis (collection of blood in the joint) as a result of hemophilia. Foam rubber straps, adhesive moleskin, elastic bandages, or cloth belts are applied to the skin and then attached to the weights and pulleys. If skin traction to the lower leg is needed, a foam rubber or fabric boot may be used; the fit should be secure.
Skin traction is not appropriate if the child has a skin infection, an open wound, or extensive tissue damage. Skin breakdown may develop as a result of skin traction. Applying tincture of benzoin to the intact skin before the traction is applied may protect against skin irritation.
If the traction has not been set up correctly, neurovascular impairment may occur. Therefore, skin traction is not appropriate for patients with abnormal sensation in the lower extremities (TSRHC, 2008). Hyperextension of the knee and elastic bandages that have been wrapped too tightly are the most common causes of traction-related neurovascular impairment. A thorough assessment of the traction apparatus and the extremity should be conducted at least once each shift.
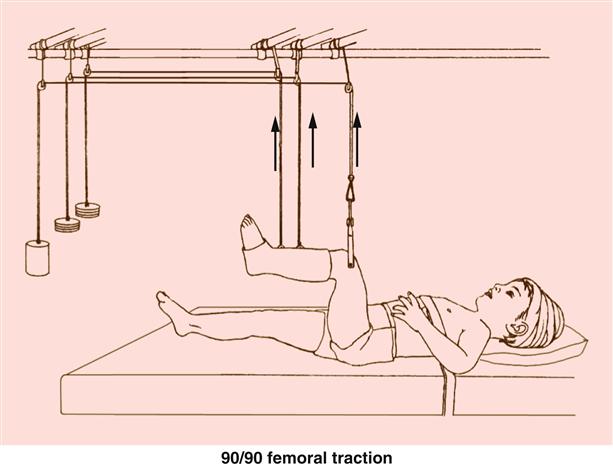
Skeletal Traction
Skeletal traction (Box 50-2 and Figure 50-2) exerts greater force than skin traction and can be physiologically tolerated for longer periods. Skeletal traction helps maintain correct alignment of the bony fragments and assists in proper healing. Traction is maintained by a metal device inserted into the bone. The fracture site determines the insertion site of the stainless steel wires, pins, or tongs. Common sites for skeletal traction include the skull, the proximal end of the ulna, and the distal end of the femur, as well as the tibia and heel. General anesthesia is necessary for skeletal traction placement and removal.
The most serious complication associated with skeletal traction is osteomyelitis, an infection involving the bone. Organisms gain access to the bone systemically or through the opening created by the metal pins or wires used for traction. Clinical manifestations include localized pain, swelling, warmth, tenderness, unusual odor, fever, and irritability or lethargy in young children. To decrease the risk of infection, pin site care is required at least once per day. Pin care protocols involve inspecting each site for signs of infection (e.g., tenting or pulling around the pin, redness at the site, purulent drainage) and cleaning the skin around pin sites with one of various cleansing solutions (e.g., chlorhexidine gluconate, plain normal saline, soap and water), A recent evidence-based practice review of pin site care protocols was inconclusive as to the best method for preventing infection at pin sites (Lethaby, Temple, & Santy, 2008).
External Fixation Devices
External fixation devices may also be used in the treatment of complex fractures, to lengthen bones, and to correct angular deformities that involve bone and soft tissue. These devices provide distraction, keeping the bone ends separated and in alignment so healing can occur. External fixators also allow periodic changes in alignment and bone length. External fixation devices, such as the Ilizarov external fixator (Figure 50-3), consist of pins or wires inserted through skin, soft tissue, and bone and secured on the outer limb surface to a rigid metal frame. General anesthesia is necessary for placement and removal of external fixation devices.
Because pins or wires of the external fixator pass through the skin to anchor in the bone, meticulous assessment of entry sites for signs of inflammation, infection, or loose pins is necessary. Pin tract infection occurs in approximately 50% of cases (TSRHC, 2008). Pin site care, similar to pin site care for children in traction, is recommended. To prevent injury to the other limb or to others, sharp protrusions from the fixator need to be adequately covered.
Nursing Considerations
Before application of an immobilizing device, assess the child’s and parents’ knowledge about the procedure. Also assess the child’s skin and note the presence of any bruises or abrasions that may be covered by the device.
Neurovascular Status
After the device is applied, perform a neurovascular assessment (CSM—circulation, sensation, and motion) at least every 2 hours during the first 48 hours. Assess the strength of the pulse distal to the site, and compare it with the pulse in the uninvolved extremity. A sluggish capillary refill time may indicate neurovascular impairment.
Signs of circulatory impairment include coldness, pallor, blueness of the extremity, swelling, loss of motion, and numbness and tingling of the extremity. Touch the child’s skin proximal and distal to the device to assess temperature; ask the child to move the fingers or toes. Paresthesia, or numbness, burning, and tingling, can be assessed by touching the fingers or toes and noting any decrease or loss of feeling. Paresthesia is of serious concern because paralysis can result if the problem is not corrected. Report a child’s complaints of a pins-and-needles sensation or of the extremity “feeling asleep.” Young children are not always able to describe a feeling or sensation, so avoid questions such as “Do you feel this?” Instead, ask a child to wiggle the fingers or toes to appropriately determine motor impairment.
Special Considerations for the Child in Halo Traction
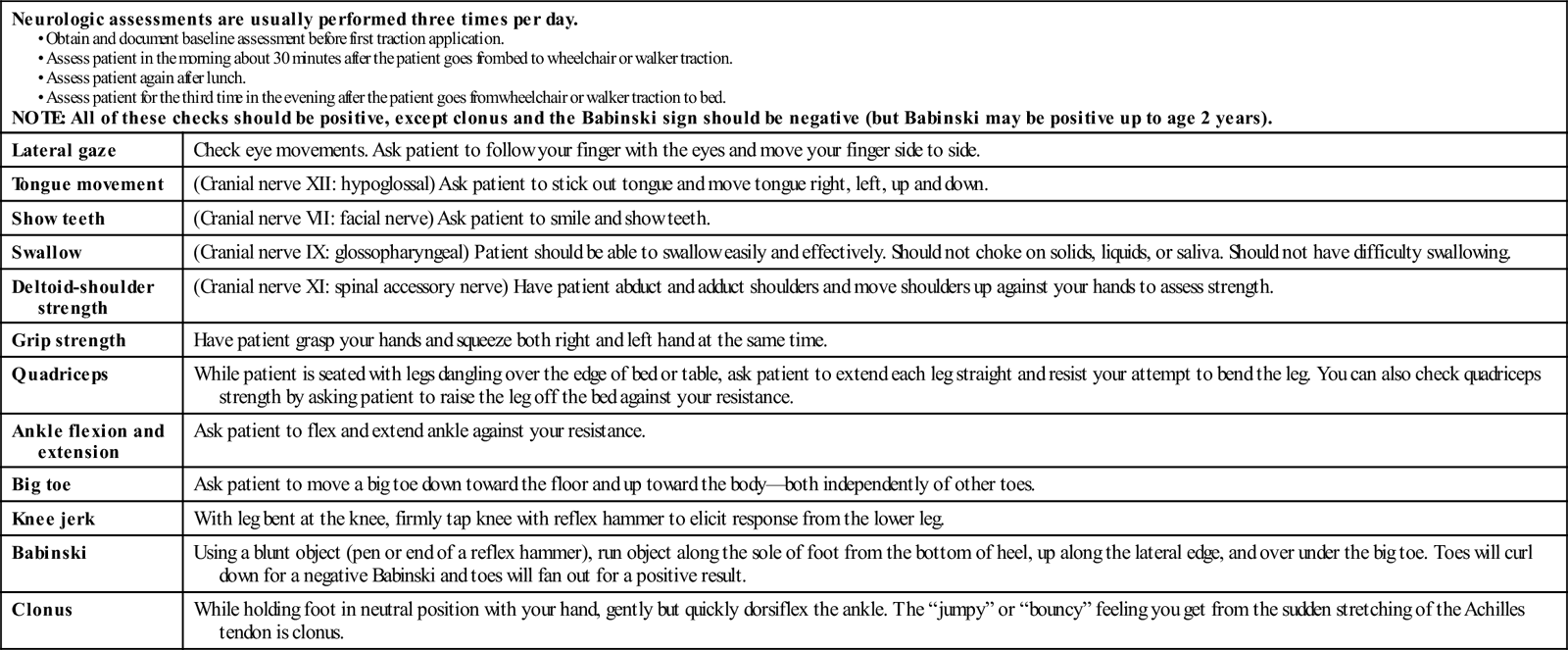
Children who must be in halo traction have additional neurovascular issues that need to be addressed (Table 50-1).
TABLE 50-1
NEUROLOGIC ASSESSMENT FOR PATIENTS REQUIRING HALO TRACTION
| Neurologic assessments are usually performed three times per day. NOTE: All of these checks should be positive, except clonus and the Babinski sign should be negative (but Babinski may be positive up to age 2 years). | |
| Lateral gaze | Check eye movements. Ask patient to follow your finger with the eyes and move your finger side to side. |
| Tongue movement | (Cranial nerve XII: hypoglossal) Ask patient to stick out tongue and move tongue right, left, up and down. |
| Show teeth | (Cranial nerve VII: facial nerve) Ask patient to smile and show teeth. |
| Swallow | (Cranial nerve IX: glossopharyngeal) Patient should be able to swallow easily and effectively. Should not choke on solids, liquids, or saliva. Should not have difficulty swallowing. |
| Deltoid-shoulder strength | (Cranial nerve XI: spinal accessory nerve) Have patient abduct and adduct shoulders and move shoulders up against your hands to assess strength. |
| Grip strength | Have patient grasp your hands and squeeze both right and left hand at the same time. |
| Quadriceps | While patient is seated with legs dangling over the edge of bed or table, ask patient to extend each leg straight and resist your attempt to bend the leg. You can also check quadriceps strength by asking patient to raise the leg off the bed against your resistance. |
| Ankle flexion and extension | Ask patient to flex and extend ankle against your resistance. |
| Big toe | Ask patient to move a big toe down toward the floor and up toward the body—both independently of other toes. |
| Knee jerk | With leg bent at the knee, firmly tap knee with reflex hammer to elicit response from the lower leg. |
| Babinski | Using a blunt object (pen or end of a reflex hammer), run object along the sole of foot from the bottom of heel, up along the lateral edge, and over under the big toe. Toes will curl down for a negative Babinski and toes will fan out for a positive result. |
| Clonus | While holding foot in neutral position with your hand, gently but quickly dorsiflex the ankle. The “jumpy” or “bouncy” feeling you get from the sudden stretching of the Achilles tendon is clonus. |
Assessing and Managing Compartment Syndrome
Serious complications, such as nerve compression, circulatory impairment, or compartment syndrome, can result from swelling caused by trauma or an immobilizing device. The muscles and nerves of the upper and lower extremities are enclosed in compartments that are surrounded by tough, inelastic fascia (comparable to sausage casing). Compartment syndrome occurs when swelling causes pressure within these closed fascial compartments to rise, compromising vascular perfusion to the muscles and nerves (Bakody, 2009). Compartment syndrome is a true surgical emergency that requires prompt diagnosis and intervention to prevent paralysis and necrosis of tissues (Bakody, 2009; TSRHC, 2008).
Signs of compartment syndrome include severe pain, often unrelieved by analgesics, and signs of neurovascular impairment (TSRHC, 2008). If extending the fingers or wiggling the toes produces pain, and/or the quality of the radial or pedal pulse is poor to absent, notify the physician. In addition, assess for pallor, paresthesia, and pulselessness as previously described. Paresis and paresthesias are late findings, typically a sign of permanent damage (TSRHC).
The diagnosis of compartment syndrome is made primarily on physical findings, but if physical findings provoke any question, diagnosis can be aided by measurement of the pressure within the affected compartment. The intracompartmental pressure at which a compartment syndrome exists is unknown, and pressure may vary with the technique of measurement (TSRHC, 2008). If compartment syndrome is suspected, the nurse should immediately elevate the extremity only to the level of the child’s heart, loosen any restrictive bandages or dressings (if able), split the cast (if able), notify the physician immediately, and administer pain medication as ordered (Bakody, 2009). The child will need to be kept on nothing-by-mouth (NPO) status for possible emergent surgical management.
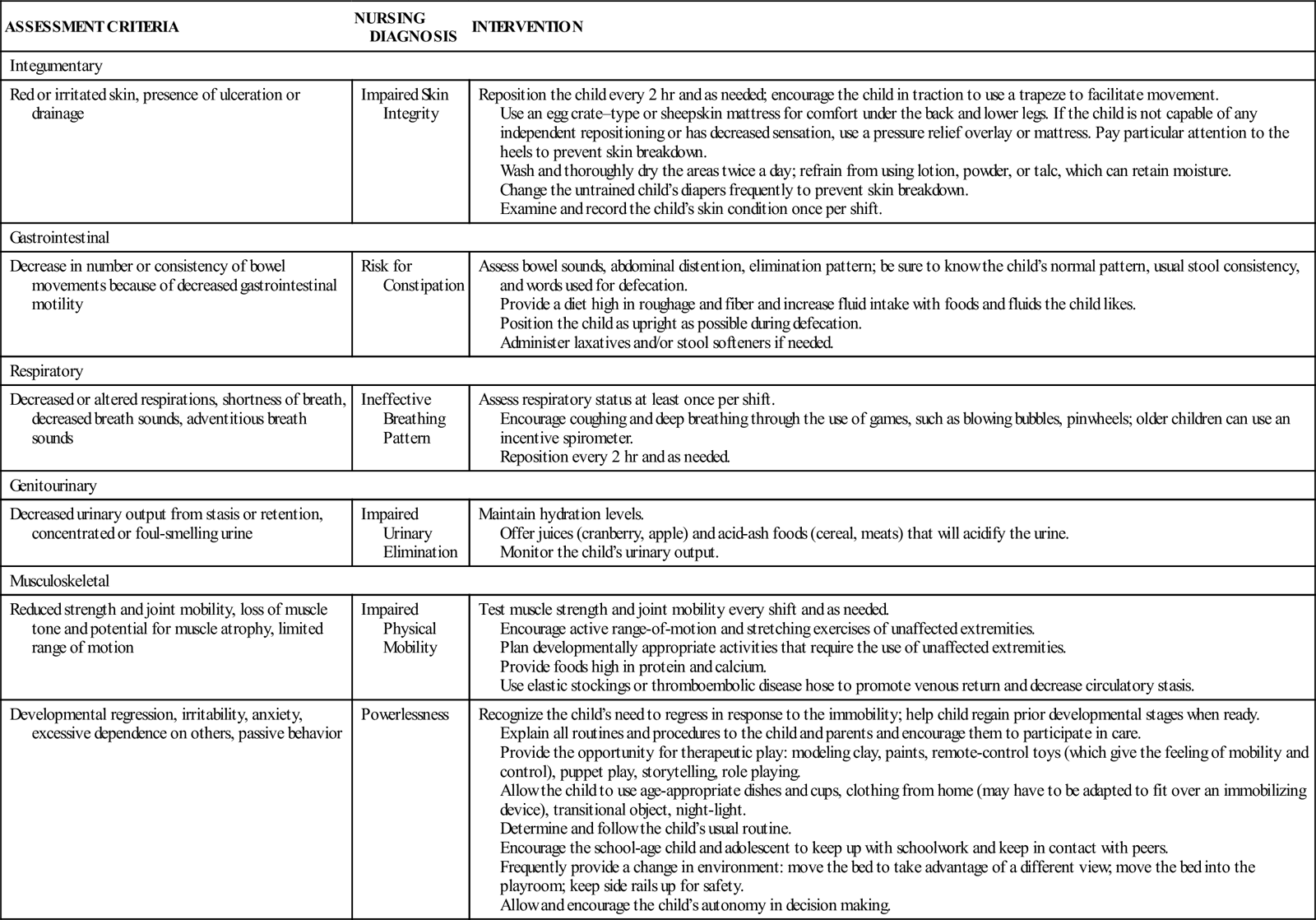
Immobility
Children in immobilizing devices are subject to the consequences of immobility. Immobility can affect several body systems. Appropriate assessment and intervention can prevent adverse effects (Table 50-2).
TABLE 50-2
| ASSESSMENT CRITERIA | NURSING DIAGNOSIS | INTERVENTION |
| Integumentary | ||
| Red or irritated skin, presence of ulceration or drainage | Impaired Skin Integrity | Reposition the child every 2 hr and as needed; encourage the child in traction to use a trapeze to facilitate movement. Use an egg crate–type or sheepskin mattress for comfort under the back and lower legs. If the child is not capable of any independent repositioning or has decreased sensation, use a pressure relief overlay or mattress. Pay particular attention to the heels to prevent skin breakdown. Wash and thoroughly dry the areas twice a day; refrain from using lotion, powder, or talc, which can retain moisture. Change the untrained child’s diapers frequently to prevent skin breakdown. Examine and record the child’s skin condition once per shift. |
| Gastrointestinal | ||
| Decrease in number or consistency of bowel movements because of decreased gastrointestinal motility | Risk for Constipation | Assess bowel sounds, abdominal distention, elimination pattern; be sure to know the child’s normal pattern, usual stool consistency, and words used for defecation. Provide a diet high in roughage and fiber and increase fluid intake with foods and fluids the child likes. Position the child as upright as possible during defecation. Administer laxatives and/or stool softeners if needed. |
| Respiratory | ||
| Decreased or altered respirations, shortness of breath, decreased breath sounds, adventitious breath sounds | Ineffective Breathing Pattern | Assess respiratory status at least once per shift. Encourage coughing and deep breathing through the use of games, such as blowing bubbles, pinwheels; older children can use an incentive spirometer. Reposition every 2 hr and as needed. |
| Genitourinary | ||
| Decreased urinary output from stasis or retention, concentrated or foul-smelling urine | Impaired Urinary Elimination | Maintain hydration levels. Offer juices (cranberry, apple) and acid-ash foods (cereal, meats) that will acidify the urine. Monitor the child’s urinary output. |
| Musculoskeletal | ||
| Reduced strength and joint mobility, loss of muscle tone and potential for muscle atrophy, limited range of motion | Impaired Physical Mobility | Test muscle strength and joint mobility every shift and as needed. Encourage active range-of-motion and stretching exercises of unaffected extremities. Plan developmentally appropriate activities that require the use of unaffected extremities. Provide foods high in protein and calcium. Use elastic stockings or thromboembolic disease hose to promote venous return and decrease circulatory stasis. |
| Developmental regression, irritability, anxiety, excessive dependence on others, passive behavior | Powerlessness | Recognize the child’s need to regress in response to the immobility; help child regain prior developmental stages when ready. Explain all routines and procedures to the child and parents and encourage them to participate in care. Provide the opportunity for therapeutic play: modeling clay, paints, remote-control toys (which give the feeling of mobility and control), puppet play, storytelling, role playing. Allow the child to use age-appropriate dishes and cups, clothing from home (may have to be adapted to fit over an immobilizing device), transitional object, night-light. Determine and follow the child’s usual routine. Encourage the school-age child and adolescent to keep up with schoolwork and keep in contact with peers. Frequently provide a change in environment: move the bed to take advantage of a different view; move the bed into the playroom; keep side rails up for safety. Allow and encourage the child’s autonomy in decision making. |
Special Considerations for the Child in Traction
Children who are placed in traction are hospitalized from several days to weeks depending on the underlying condition. It is imperative that the nurse check the amount of traction the patient is receiving against the physician’s orders; all weights should be hanging free and not touching the floor or bed, and all ropes need to be appropriately on the pulleys. Elevate the head or foot of the bed as indicated to maintain countertraction. It may be necessary to draw a line on the child’s bed sheet and ask the parents to keep the child above that line. An older child can pull on an overhead trapeze to maintain proper position and alignment.
Home Care
Most children are discharged home shortly after a cast application. The box, Parents Want to Know: Home Care for the Child in a Cast, presents basic principles for caring for a child in a cast at home. Care for children discharged with an external fixator may involve frequent neurovascular assessments and possibly pin site care. Parents must be able to describe how to care for the cast or fixator, when they need to contact their physician, and how to contact any needed resources in the community (e.g., physical therapy, occupational therapy, school district personnel). The nurse can also help the parents select appropriate clothing and adaptive devices if appropriate. Encourage the parents to promote the child’s self-care whenever possible.
Fractures
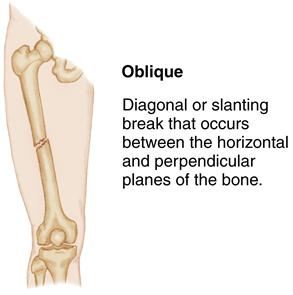
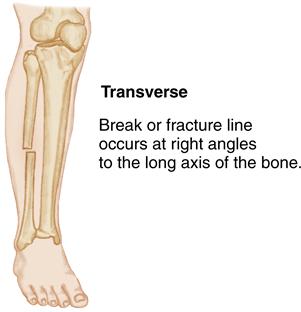
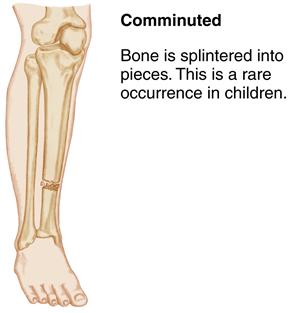
Fractures in children are common and can vary in severity from benign to life threatening. A fracture is a break or disruption in a bone’s continuity. Generally fractures occur when excessive or traumatic force exceeds the strength of the bone.
Etiology
Fractures in children usually result from increased mobility and inadequate or immature motor and cognitive skills. They may result from accidental trauma (e.g., falls, motor vehicle crashes, sports injuries), nonaccidental trauma (e.g., child abuse), or pathologic conditions that result in abnormally fragile bones (e.g., osteogenesis imperfecta, tumors, cysts).
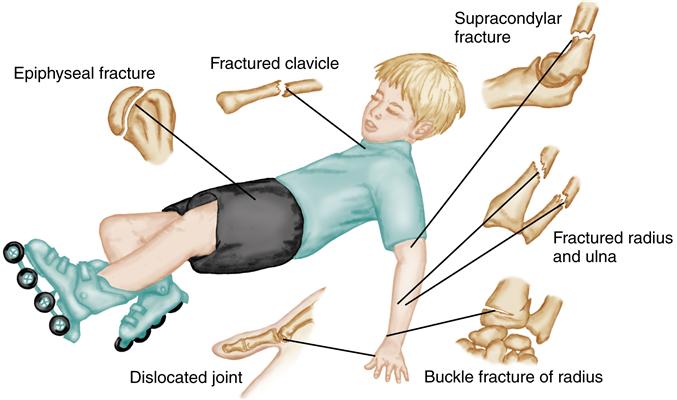
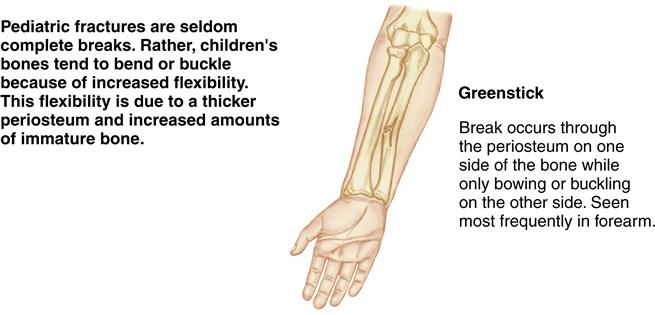
Many biochemical and physiologic properties of pediatric bones differ from those of adults. Three essential differences contribute to the understanding of injury, fracture patterns, healing, and treatment (Firmin & Crouch, 2009). First, children’s bones are less brittle with a higher collagen-to-bone ratio. This difference is protective, making incomplete fractures more likely. Secondly, children have a stronger periosteum. This also makes complete fractures less likely or at least limits fracture displacement. The third essential pediatric bone difference is the epiphyseal plate or growth plate. The epiphyseal plate is the weakest part of the growing bone, but often bears the brunt of children’s bone injuries.
An understanding of growth and development is helpful when assessing trauma in specific age-groups. For example, fractures in infancy are generally rare because of the cartilaginous quality of the skeleton. Fractures in infants are usually the result of trauma during birth or nonaccidental trauma. Therefore, fractures that occur after the birthing process warrant further investigation to rule out the possibility of child abuse.
Clavicle fractures can occur at any age. Lack of movement or a pseudoparalysis of the upper extremity may be the only sign in an infant who has sustained a fractured clavicle during birth. It is important to assess the infant with clavicle fracture for brachial plexus palsy because the two may be associated. An older child will report pain and show swelling on the clavicle at the site of the fracture. A common mechanism of clavicle injury in older children is blunt trauma from contact sports.
Another major cause of children’s fractures is falls. The outstretched arm often receives the full force of the fall, even
though this action is the result of the child’s protective reflexes (Figure 50-4). Although this force of impact can involve any part of the arm (wrist, elbow, shoulder), the supracondylar humeral fracture of the elbow is most commonly seen with this type of fall. Secondary complications of this injury include circulatory impairment, cellular necrosis, neurovascular damage, ischemic contracture (Volkmann contracture), or compartment syndrome.
A thorough and timely assessment for a fracture is important to prevent loss of function and disturbance to the bone growth of the pediatric patient regardless of age or type of skeletal injury. Understanding the etiology and location of the fracture is important to prevent complications.
Incidence
Pediatric trauma is the leading cause of death and disability in children and one of the largest challenges to their health (Vitale, 2010). The United States has the highest incidence of pediatric trauma among developing nations; musculoskeletal trauma makes up the largest portion of pediatric injuries, with 25% of children sustaining an injury annually and 10% to 25% of those injuries being fractures (Vitale, 2010).
Fractures are common in children and adolescents because numerous gross motor activities place them at risk for injury. Young children are acquiring new motor skills, whereas older children and adolescents are participating in risk-taking behaviors as part of their normal growth and development. It is estimated that 40% of boys and 25% of girls will sustain a fracture by 16 years of age (Vitale, 2010). The distal forearm is the most common site to be fractured in children; the clavicle is second.
Manifestations
Presentation of fractures vary with location, type, and cause of injury. General signs and symptoms include pain or tenderness at the site, immobility or decreased range of motion, deformity, and swelling. Other signs and symptoms include crepitus, ecchymosis, erythema, muscle spasm, and inability to bear weight.
The periosteum of children’s bones is thicker and stronger than that of adults, and therefore, fractures are less likely to be displaced. Local signs and symptoms of a fracture are not always present, which may make diagnosis of a fracture difficult. Radiography is the most effective tool for determining the type and location of a fracture. Fractures may not be visible on radiographs until healing begins. A radiograph of the unaffected extremity may be obtained for comparison purposes, especially when trying to determine whether a line on the radiograph represents a fracture or merely an epiphyseal line. Radiographs are also obtained after fracture reduction and during the healing process to assess progress.
Therapeutic Management
The goal for managing fractures in children is to maintain function without affecting growth. The key to healing is correct fracture reduction and retention. Reduction is the repositioning of the bone fragments into normal alignment. Retention entails the application of a device or mechanism that maintains alignment until healing occurs.
Reduction Methods
Fractures are treated by either closed or open reduction. Closed reduction is accomplished by manual alignment of the fragments followed by immobilization. Simple or closed fractures are treated by closed reduction. Hospitalization is seldom necessary for closed reduction, and most of these fractures heal without complications.
Open reduction entails the surgical insertion of internal or external fixation devices, such as rods, wires, or pins that help maintain alignment while healing occurs. When open reduction is used, hospitalization may be required to assess the child for postoperative complications. Complications after open reduction include delayed healing, nonunion, and infection. Close assessment by the health care team and strict adherence to sterile technique during dressing changes can decrease the risk of postoperative problems and promote healing.
Retention
Once the bone is aligned, the fracture site must be protected and the position of the fragments maintained. This is accomplished through the application of a splint, cast, external fixation device, or traction, which effectively immobilizes the area while healing occurs.
Nursing Considerations
Initial Trauma Assessment
Nursing assessment of the child with a traumatic fracture should begin with a thorough primary survey (see Chapter 34). A complete history of the circumstances surrounding the fracture should be obtained to identify the mechanism of injury and rule out nonaccidental trauma.
Examine the fracture site for bruising, skin lacerations, and swelling. Generally the child will favor the extremity, by cradling or guarding the limb. Often the child will report numbness and tingling distal to the fracture site. Movement and range of motion may be limited. The five Ps of neurovascular status should be assessed carefully and interventions initiated appropriately to prevent impairment.
Assessing and Managing Complications
Fat embolism and resultant respiratory distress are commonly seen in adults with multiple or long-bone fractures but are rare in children (Farley & Kay, 2010). Although the cause of fat embolism is unclear, particles of fat escape from the fracture site, are carried through the circulatory system, and lodge in the lung capillaries. Signs and symptoms of fat embolism are the same in a child as in adults. These include axillary petechiae, hypoxemia, and radiograph changes showing pulmonary infiltrates of the lungs (Farley & Kay, 2010). These changes appear within several hours after the fractures. Rarely, fat emboli can lodge in the small capillaries in the brain or other vital organs. Hypoxemia and mental status changes are typically caused by other injuries or from overmedication with opioid analgesics rather than fat embolism. Minimal movement of fractured extremities can prevent or lessen the effects of fat embolism. Treatment is primarily supportive and includes volume resuscitation, respiratory support, and adequate oxygenation.
Another complication that can occur with an orthopedic injury is deep vein thrombosis. The incidence of deep vein thrombosis in children is between 0.2 and 3.3 per 1000 pediatric trauma discharges (O’Brien, Haley, Kelleher, et al., 2008). Risk factors include prolonged immobility, obesity, increasing age, and long-bone trauma (Goel, Buckley, deVries, et al., 2009). Prevention includes elevation of the fractured extremity, early ambulation with support, and prompt initiation of postoperative physiotherapy. Pain management is an important adjunct for meeting this goal, as well as for promoting healing and shortening hospital stay. Currently, there is no standard of care for deep vein thrombosis prophylaxis in the pediatric or adolescent trauma patient (O’Brien et al., 2008).
Soft Tissue Injuries: Sprains, Strains, and Contusions
Soft tissue injuries are common among children and are usually related to play or athletic activities.
Etiology
Sprains occur as a result of trauma to a joint in which ligaments are stretched or are partially or completely torn. Strains, also known as pulls, tears, or ruptures, result from an excessive stretch of muscle. Contusions occur when soft tissue, muscle, or subcutaneous tissues are damaged. Sprains and contusions frequently accompany each other. Dislocation occurs when a joint is disrupted in such a way that articulating surfaces are no longer in contact.
Incidence
Sprains are not frequently seen in young children because of their poorly developed epiphyseal plates. A twisting or turning injury will more likely result in a fracture at the weak epiphyseal location than a sprain. Sprains and strains are more common in adolescents and are frequently the result of athletic injuries. Anterior cruciate ligament (ACL) tears are one of the most common types of knee injury, especially in adolescent athletes.
Rising participation in sports has been associated with an increase in sports-related injury in young children (Table 50-3). It has been estimated that 3.5 million children age 14 years or younger have received medical treatment for a sports-related injury each year (Andrews, Baker, Bergfeld, et al., 2010).
TABLE 50-3
| LOW | LOW TO MODERATE | MODERATE | MODERATE TO HIGH | HIGH | VERY HIGH |
| Swimming Tennis | Running Inline skating Strength training | Ballet Baseball Basketball Gymnastics Soccer | Ice hockey Horseback riding Skiing Snowboarding | Cycling Diving American football Skateboarding Wrestling | Trampoline |
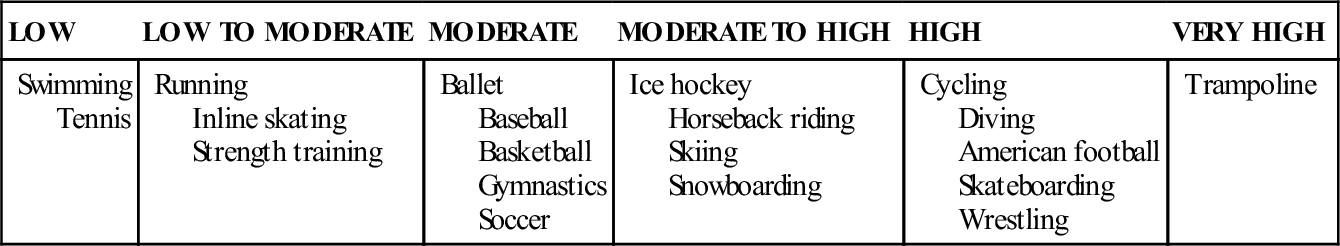
Data from Staheli, L. T. (Ed.). (2008). Fundamentals of pediatric orthopedics (4th ed., pp. 90-92). Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins.
Manifestations and Diagnostic Evaluation
Manifestations of soft tissue injuries include pain, swelling, localized tenderness, limited range of motion, poor weight bearing, and a pop or snapping sound (sprain). The diagnosis is made on the basis of the clinical picture. A radiographic examination, however, may be ordered to rule out a fracture. Magnetic resonance imaging (MRI) or arthroscopy may be necessary to diagnose knee ligament tears.
Therapeutic Management
The primary goal in managing a soft tissue injury is to control swelling and prevent further injury. External pressure (compression) is most beneficial before edema has accumulated (Draper & Knight, 2010). Swelling can inhibit healing by keeping the ligament ends separated and increasing fibrous scarring. The earlier treatment is initiated, the less severe the swelling and immobility.
The injured area should be immediately wrapped with a compression bandage to support the joint and control the swelling. Ice should be applied to the injured area to reduce swelling for no longer than 20 minutes at a time. The effects of the ice can last as long as 5 to 6 hours, and ice should be used repeatedly for several days. Nonsteroidal antiinflammatory drugs (NSAIDs) help to alleviate pain and reduce inflammation.
For more severe soft tissue injuries, the child should avoid weight bearing for 3 days. Crutches may be necessary to ensure that the child does not bear weight. An air cast, which is a plastic, air-filled pressure cuff, may be used over the elastic wrap to support the joint and reduce swelling. The air cast or compression bandage should be worn for several weeks while the joint is healing. The child can begin stretching and isometric exercises to improve joint stability after the swelling and pain have diminished.
Immobilization of the injured joint and cold application are generally effective in the treatment of incomplete ligament tears. A complete rupture could require surgery to prevent excessive scar formation and long-term joint stability problems. Application of a cast or splint for 4 to 5 weeks may also be necessary, especially for knee injuries.
Nursing Considerations
One of the major nursing functions when assessing a sprain is to determine the severity of the injury. Assess the child for neurovascular impairment and for diminished range of motion. The initial examination may reveal localized tenderness over the injured joint, as well as limited joint mobility.
Analgesics, such as ibuprofen or acetaminophen, are appropriate for pain management. Distraction and age-appropriate play activities can be effective in helping children cope with pain.
The nurse needs to keep the extremity elevated at the level of the heart. This position enhances venous return and aids in reducing the swelling. Pillows placed beneath the extremity provide support and comfort. Support and immobilization devices should be snug but not tight. Assess neurovascular status before and after application of any splint, compression wrap, or cast.
For the child who has undergone surgery for any type of knee ligament reconstruction, immediate postoperative use of a cold compression cuff and a continuous passive motion (CPM) machine—a machine that continuously moves the knee joint in flexion and extension—will likely be used. Nursing measures involve regular emptying and refilling of the cuff to maintain the cold temperature. The nurse must also check the settings on the CPM machine to ensure that they match the ordered degree of flexion and extension. Pain control is most important.
Stretching and strengthening exercises are helpful in maintaining joint and muscle integrity. These exercises are done passively at first. As healing progresses, teach the child active stretching and strengthening exercises. The effectiveness of parent and family teaching should be evaluated by return demonstration. Physical therapy referrals may be helpful as well.
The amount of time needed for healing is determined by the severity of the injury. Weight bearing is gradually increased as the pain subsides. More severe injuries may require partial weight-bearing exercises, with full weight bearing introduced once the swelling has resolved. Activities may be restricted as directed by the health care provider.
Review the principles of rest, support, and the application of ice with the parents and child. If wraps, splints, or air casts are used, teach the parents and child how to assess neurovascular status. If crutches are required, review the principles of crutch walking with both the parents and the child. Make sure all family members understand activity and sports restrictions. Discuss follow-up appointments and the importance of adhering to activity restrictions until the injury has healed and the child has been cleared for participation in sports.