Chapter 4. The autonomic nervous system, asthma, 5-hydroxytryptamine and migraine
At the end of this chapter, the reader should be able to:
• give examples of sympathomimetic and parasympathomimetic drugs
• give examples of selective α and β agonists and antagonists
• describe the anatomy of the autonomic nervous system
• name the neurotransmitters and receptors of the autonomic nervous system
• describe the effects of sympathetic and parasympathetic stimulation on visceral organs
• explain the action and uses of drugs that block the action of acetylcholine
• describe the symptoms of migraine and how they may be prevented and treated
Introduction to the autonomic nervous system
The autonomic nervous system is that part of the nervous system which supplies the viscera as distinct from the voluntary muscles.
The viscera include:
• the gastrointestinal tract
• the respiratory and urogenital systems
• the heart and blood vessels
• the intrinsic muscles of the eyes
• various secretory glands.
The autonomic nervous system consists of two divisions, called the sympathetic and parasympathetic systems. Nerves from both these divisions supply most of the viscera. In general they have opposite effects on the various viscera which they supply, and they also differ in both their anatomical arrangement and mechanism of function.
Components of the autonomic nervous system
Sympathetic nervous system
The sympathetic nervous system consists of a chain of ganglia lying on either side of the vertebral column and extending from the cervical to the lumbar vertebrae. Sympathetic nerve fibres, after passing out from the spinal cord, leave the anterior nerve root and pass to one of these ganglia. Here they form a synapse or junction with further nerve cells whose fibres are distributed to the viscera.
Some sympathetic fibres, after leaving the spinal cord, pass through the ganglia and form their synapses in ganglia situated peripherally; the group of ganglia surrounding the coeliac artery is a good example of this arrangement.
Parasympathetic nervous system
The parasympathetic fibres leave the central nervous system (CNS) and are distributed with certain cranial nerves (III, VII, IX and X) and with the sacral nerves. The relay ganglia of the parasympathetic system are situated peripherally near the organs supplied (Fig. 4.1).
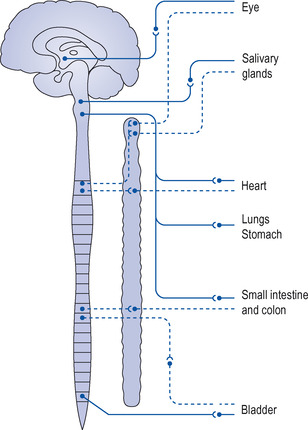 |
| Figure 4.1 The anatomy of the autonomic nervous system. Sympathetic, dashed line; parasympathetic, solid line. |
Sensory fibres
The autonomic system also carries a large number of sensory nerves, which supply the various organs. These nerves carry information from the organ to the CNS. They enter the spinal cord, where they may form a spinal reflex arc with the autonomic nerves leaving the cord or they may ascend to the brain where more complex reflexes are built up which may be influenced by impulses arising from the higher levels of the brain. Some visceral sensation may enter consciousness and events in consciousness may themselves stimulate various visceral effects. The rapid beating of the heart after a fright is a typical example.
Chemical transmission of nerve impulses
Stimulation of a nerve liberates a substance called a neurotransmitter at the nerve ending, which activates a receptor in the organ supplied or in another nerve cell. This is known as the chemical transmission of nerve impulses and is an important concept because many drugs act by interfering with this process. In the autonomic nervous system, transmission occurs in this way in both the sympathetic and parasympathetic divisions, but the neurotransmitter released onto the target organ differs, being acetylcholine in the parasympathetic division and noradrenaline in the sympathetic division.
The parasympathetic system (Fig. 4.2)
Following stimulation of a parasympathetic nerve, a neurotransmitter called acetylcholine (ACh) is liberated at the nerve ending; ACh acts on a receptor on the organ supplied by the nerve. To prevent the effect of acetylcholine being too prolonged and powerful, there is also present at the nerve ending an enzyme called acetylcholinesterase, which rapidly breaks down the acetylcholine and terminates its effect.
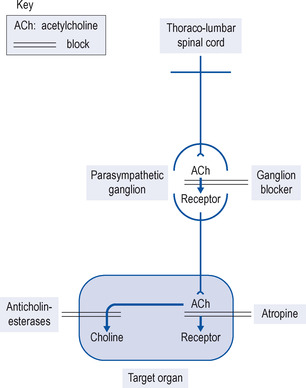 |
| Figure 4.2 Principal neurotransmitter and its receptors in the parasympathetic division of the autonomic nervous system and sites of receptor blocking drugs. |
The sympathetic system (Fig. 4.3)
The sympathetic nerves release the neurotransmitter noradrenaline from stores at the nerve endings in the peripheral tissues. In addition, the sympathetic system releases adrenaline (90%) and noradrenaline (10%) from the medulla of the adrenal gland; these substances enter the bloodstream and produce widespread effects. Noradrenaline and adrenaline produce these effects by combining with specific sympathetic adrenoceptors on the target organs. There are several types of sympathetic receptors:
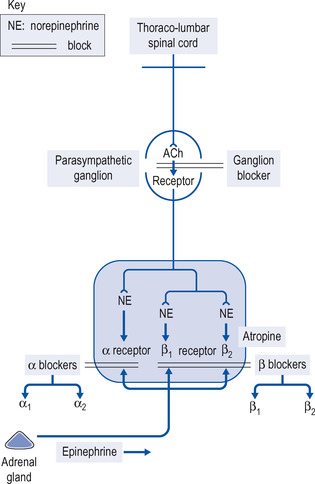 |
| Figure 4.3 Neurotransmitters and receptors of the sympathetic division of the autonomic nervous system and sites of receptor blocking drugs. |
Adrenoreceptors
Types of adrenoreceptors:
• α 1
• α 2
• β 1
• β 2
• β 3
α 1 Receptors
These receptors occur on target tissues opposite the nerve terminal and are stimulated by noradrenaline released at sympathetic nerve endings and by adrenaline. Stimulation produces constriction of blood vessels, causing a rise in blood pressure and reflex slowing of the heart, and dilatation of the pupil. Stimulation of α 1 receptors is blocked by several drugs (see p. 52).
α 2 Receptors
These receptors occur on the nerve terminal from which noradrenaline is released, and when noradrenaline binds them they limit further release of noradrenaline, thus forming a release control mechanism. α 2 Receptors are targets for drugs such as clonidine, which stimulate them selectively to inhibit further noradrenaline release, and are therefore useful to treat hypertension.
β 1 and β 2 receptors (Figure 4.4 and Figure 4.5)
These receptors are both stimulated by isoprenaline and adrenaline (epinephrine). In addition, the neurotransmitter noradrenaline (norepinephrine) acts as a β 1 stimulator on the heart, and the drug salbutamol produces a β 2 response largely on the bronchi. The effects are:
• β 1 responses – increase in rate and excitability of the heart with increased cardiac output
• β 2 responses – dilatation of bronchi and blood vessels.
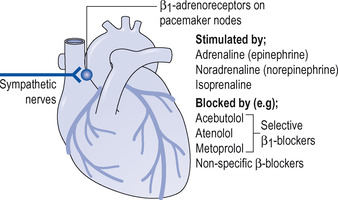 |
| Figure 4.4 Examples of β 1-adrenoceptor agonists and antagonists. |
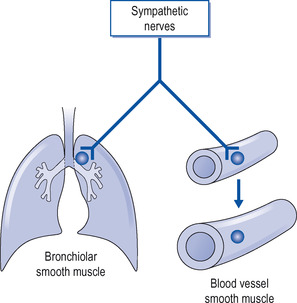 |
| Figure 4.5 β 2 Receptors are stimulated by β agonists, e.g. noradrenaline (norepinephrine), adrenaline (epinephrine) and selective β 2 agonists, e.g. sabutamol, causing dilatation. |
Overactivity of the sympathetic nervous system produced by fright or anger causes a mixed picture due to stimulation by noradrenaline and adrenaline of α 1, β 1 and β 2 receptors (see Table 4.1).
| Sympathetic activity | Parasympathetic activity | |
|---|---|---|
| Heart rate | Increased | Slowed |
| Blood vessels | Constricted | Dilated |
| Stomach and intestine | Decreased activity and secretion | Increased activity and secretion |
| Salivary and bronchial glands | Decreased secretion | Increased secretion |
| Urinary bladder | Body relaxed, sphincter contracted | Body contracted, sphincter relaxed |
| Bronchial muscle | Relaxed | Contracted |
| B lood sugar | Raised | |
| Eye | Pupils dilated | Pupils constricted Accommodates for near vision |
β 3 Receptors
These receptors have only recently been reported in cardiac muscle. They are negatively inotropic, i.e. they depress the rate and force of contraction (Moniotte & Balligand 2002).
Transmission at autonomic ganglia
The nerve that arrives at an autonomic ganglion from the CNS is termed a preganglionic nerve. The nerve with which it synapses in the ganglion, and which carries the impulse away to the target organ, is called the postganglionic nerve. Acetylcholine is liberated by the preganglionic nerve at the synapses in both sympathetic and parasympathetic ganglia, binds to its receptors on the postganglionic nerve and is thus responsible for the transmission of the nerve impulse.
Sympathomimetic drugs
Sympathomimetic drugs have effects similar to those produced by activity of the sympathetic nervous system and comprise:
• adrenaline (epinephrine)
• noradrenaline (norepinephrine)
• isoprenaline
• selective β 2 agonists.
Adrenaline (Epinephrine)
Adrenaline is released from the medulla of the adrenal gland when the sympathetic system is activated. For clinical use, however, it is prepared synthetically. It acts on the sympathetic receptors of the visceral organs. Adrenaline (epinephrine) is destroyed by gastric acid and is therefore not effective if taken orally. It is usually given by subcutaneous or intramuscular injection, its effects being produced more rapidly from the latter site. Following injection, its various actions become apparent within a minute. They are:
• An increase in the force and rate of contraction of the heart (β 1 effect), so that the patient may report palpitation.
• A rise in systolic blood pressure due to the increased cardiac output (β 1 effect). The diastolic pressure shows little change as adrenaline (epinephrine) produces vasoconstriction only in the skin and in the splanchnic area (mixed α 1 and β 2 effects) and vasodilatation in arteries in muscle (β 2 effect).
• Adrenaline (epinephrine) relaxes smooth muscle, including that of the bronchial tree (β 2 effect).
• Adrenaline (epinephrine) raises blood sugar by mobilizing glucose from tissues.
Following injection, adrenaline (epinephrine) is rapidly broken down in the body by the enzymes monoamine oxidase and methyl-O-transferase, and its effects last for only a few minutes.
Adrenaline (epinephrine) is used less now than in former times. It is still the best immediate treatment for serious anaphylactic reactions (see p. 424). In anaphylactic reactions, adrenaline (epinephrine) causes constriction of blood vessels and thus relieves oedema and swelling and stimulates the heart in cardiac arrest.
Noradrenaline (Norepinephrine)
Noradrenaline (norepinephrine) is chemically closely related to adrenaline (epinephrine) and is the neurotransmitter released from sympathetic nerves at the target organs and tissues. Its most important action is to produce widespread vasoconstriction and thus a rise in both systolic and diastolic blood pressure (α 1 effect). The body rapidly inactivates noradrenaline (norepinephrine); to produce a continuous effect on the blood pressure, it is given by intravenous infusion.
Noradrenaline (norepinephrine) has been used in the treatment of various forms of shock, which is usually associated with a very low blood pressure.
Opinion has moved against using noradrenaline (norepinephrine) to raise blood pressure except in extreme circumstances, for although a satisfying rise in blood pressure can be obtained due to vasoconstriction, this also reduces the blood flow in essential organs, particularly the kidney, with troublesome results.
Isoprenaline
Isoprenaline is a synthetic drug related to adrenaline (epinephrine); however, unlike adrenaline (epinephrine), which stimulates all sympathetic receptors, isoprenaline stimulates β 1 and β 2 receptors but not α receptors. It is well absorbed from the oral mucosa and following inhalation. It relaxes smooth muscle, including that of the bronchial tree, and also stimulates the heart, but has little or no effect on the blood pressure. It is important to avoid overdosage as it can cause dangerous cardiac arrhythmias. It is rapidly inactivated after absorption and its effects are short lived.
Isoprenaline was formerly used in the treatment of asthma, both by inhalation and orally. Because it stimulates both β 1 and β 2 receptors, its action of cardiac stimulation can precipitate fatal arrhythmias. It has now been replaced for this purpose by safer β 2 agonists such as terbutaline and salbutamol (see below).
Isoprenaline can also be given by infusion in severe bradycardia. Adverse effects include palpitation, nausea, headaches and tremors.
Selective β 2 AGONISTS
These drugs stimulate predominantly β 2 receptors, so that although they are effective bronchodilators, they have minimal effects on the heart. This is an important improvement over drugs such as isoprenaline, as the risk of cardiac arrhythmias is removed.
Salbutamol
Salbutamol is the most widely used β 2 agonist. It is a powerful bronchodilator. Salbutamol can be given by various routes, but if given orally a considerable proportion is broken down in the liver (first pass effect). Its action lasts about 4 hours. In large doses it may cause tremor and tachycardia and occasionally night cramps.
Salbutamol is used to treat bronchospasm due to asthma or bronchitis. It may be taken to relieve an attack or, on a regular basis, to control the spasm. It can be given via various routes:
• Inhalation is the most commonly used route of administration, and given in this way in the treatment of bronchospasm it is possible to get the maximum effect on the bronchi with minimal effects elsewhere. Even so, only 10% of the dose reaches the bronchial tree if the patient inhales directly from the aerosol puffer, the rest being swallowed during self-dosage (Fig. 4.6).
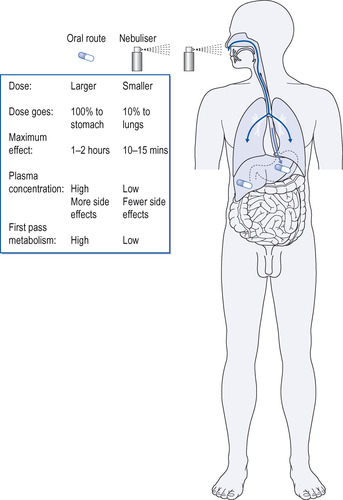 |
| Figure 4.6 Comparison of inhalation and oral dose of (e.g.) salbutamol for asthma. |
• Orally three or four times daily. Note that a relatively large dose is required because of the large first pass effect (metabolism in the liver; see p. 9), and side-effects are frequent.
• Slowly by the intravenous (I.V.) route to treat a severe asthmatic attack. This is rarely necessary, as a nebulizer is usually very effective. Salbutamol through the I.V. route requires careful monitoring for cardiac arrhythmias, and the nurse has an important role to play in monitoring the patient for cardiac arrhythmias when salbutamol is administered I.V.
In addition to its use in asthma, salbutamol is used to inhibit premature labour (see p. 225), and for treatment of hyperkalaemia. There are other selective β 2 agonists, which are very similar to salbutamol, e.g. terbutaline, fenoterol, reproterol and bambuterol.
Salmeterol and eformoterol
These drugs are long-acting β 2 agonists. They are effective after about 30 minutes and their action lasts for about 12 hours; therefore they should not be used for rapid effect in treating an acute attack, but given twice daily, by inhalation, as a preventative. It has been claimed they have some anti-inflammatory action as well as relieving bronchospasm, but this is controversial. They may be combined with an inhaled steroid.
Inhalation delivery systems
Inhalation is a useful and effective way of giving some of the drugs used to treat asthma and other forms of bronchospasm (Fig. 4.7).
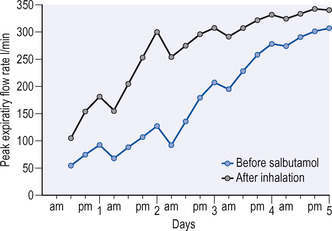 |
| Figure 4.7 The effect of inhalations of salbutamol on a patient with severe asthma. Note the progressive improvement in respiratory function and the morning dips which are characteristic of asthma. |
There are various delivery systems for inhalation. These delivery systems are:
• pressurized aerosol inhalers
• nebulizers
• delivery systems for children.
Pressurized aerosol inhalers
These are the most convenient systems for routine use by patients. The drug is dissolved or suspended in a propellant and on pressing the plunger a standard amount is released in the form of fine particles measuring 2–5 μm. It is essential that the patient be taught the technique of using the inhaler if the treatment is to be effective (Fig. 4.8).




Many patients require repeated instruction in the use of aerosols, particularly the young and elderly. Inhalers containing a placebo are available for teaching.
1. Remove the cap from the mouthpiece and shake the inhaler.
2. Breathe out slowly but not fully.
3. Place the mouthpiece in the mouth and close the lips around it.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
