Chapter 7. Atheroma and thrombosis
Anticoagulants and thrombolytic agents
LEARNING OBJECTIVES
At the end of this chapter, the reader should be able to:
• list the key stages of the coagulation cascade
• discuss the causes of thrombosis and its prevention and treatment
• give an account of the anticoagulants, and their mechanism, uses and dangers
• describe the causes and treatment of atheroma and arterial thrombosis
• list the drugs used for angina of effort
• explain the cause and treatment of coronary thrombosis
• list the drugs used for fibrinolysis
• discuss the dangers of platelet clumping and how drugs may prevent this and lower plasma lipids
Coagulation and thrombosis
Coagulation
When the wall of a blood vessel is damaged, the blood coagulates and this arrests bleeding. Clotting is a complex process, which involves numerous enzymes and other chemicals called clotting factors. Most are present in the blood plasma, some are released by the platelets, and thromboplastin is released from damaged cells. When blood clots, each clotting factor is activated in sequence as part of a cascade of reactions, as shown in Figure 7.1.
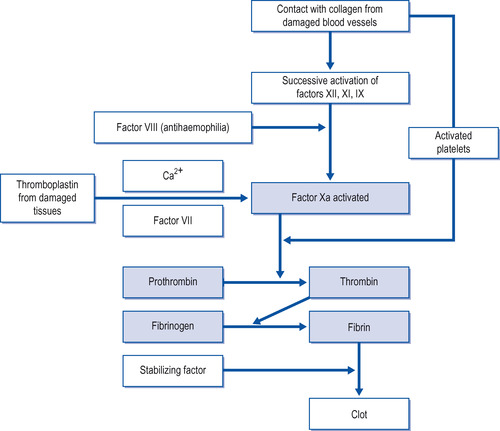 |
| Figure 7.1 The clotting cascade. |
The key stages of this series of reactions are:
• Thrombin forms fibrin strands from soluble fibrinogen, which then form a network over the damaged area.
• At the same time, platelets become activated, assisting in the clotting process and aggregate to form clumps which become enmeshed in the fibrin network. The resulting clot plugs the defect in the blood vessel.
Thrombosis
Coagulation or thrombosis may sometimes occur in blood vessels that have not been injured, and, in these circumstances, blockage of the vessel concerned may have serious consequences. There are two types of thrombosis:
• venous thrombosis (phlebothrombosis)
• arterial thrombosis.
Although both may result in obstruction to a blood vessel, they occur under different circumstances, have different mechanisms and differ in their treatment.
Venous thrombosis (phlebothrombosis)
This usually occurs in the deep veins of the legs. It is due to stagnation of blood in the veins when a patient is immobile after an operation (particularly if the pelvis or hip is involved), associated with pregnancy or during a severe illness. The risk is increased in obese patients, in patients with malignancy and in those with a history of previous thrombosis. Oral contraceptives containing estrogen are also a risk factor and should be stopped 6 weeks before a major operation or any surgery involving the pelvis or hip. It is also apparent that there are genetic factors that predispose to thrombosis. The danger of this type of thrombosis is that part of the clot may break off, forming an embolus which is swept back via the heart to the lungs, where it blocks a branch of the pulmonary artery, an event which can be fatal.
In atrial fibrillation, a thrombus may develop in the left atrium because of impaired blood flow and fragments can become detached, resulting in emboli to the brain and elsewhere. Anticoagulants, which interfere with the clotting (coagulation) of blood, can be used either to prevent the formation of thrombi or to treat an established venous thrombosis.
Anticoagulants
Anticoagulants are drugs that interfere with clotting and are used to prevent and treat venous thrombosis. They include:
• heparin and heparin-like compounds
• hirudin
• the coumarins:
warfarin
phenindione.
Heparin and heparin-like compounds
Heparin is a complex mixture of acidic substances. It occurs naturally, and is stored in mast cells and basophils. It is a very potent anticoagulant.
Mechanism of action of heparin
Heparin’s actions on the clotting mechanism are multiple and complicated. Briefly, heparin inhibits coagulation by binding to antithrombin III. Antithrombin III is part of the system that regulates clotting. It binds to certain clotting factors (see Fig. 7.1) and renders them inactive. When heparin binds to antithrombin III, this enhances antithrombin’s reaction with the clotting factors considerably. The end result is a prolongation of the clotting time. The clotting time is the time taken for blood or plasma to coagulate under controlled laboratory conditions.
Preparations of heparin
There are two preparations of heparin:
• unfractionated heparin
• low molecular weight heparins.
Heparin is a large molecule that can be broken down into a number of fragments, not all of which have anticoagulant properties. Those fragments that do have anticoagulant activity are known as low molecular weight heparins. Unfractionated heparin may vary in its potency, depending on batches and sources of supply, because of variations in the relative amounts of active and inactive fragments in its structure.
Emerging advantages of low molecular weight fragments of heparin
• Low molecular weight heparins may be better than ordinary low-dose unfractionated heparin in preventing the venous thrombosis that may complicate surgery, particularly hip and knee replacement.
• Given subcutaneously, they are as effective as intravenous unfractionated heparin in the prevention and treatment of venous thrombosis and pulmonary embolism.
• They have also been used with success in unstable angina.
• As they do not cross the placental barrier, they can be used during pregnancy.
• Since their activity can be more consistently controlled during preparation, patients may not need the same degree of monitoring.
• The mechanism of anticoagulant action of active fragments is very similar to that of unfractionated heparin but the effect is more prolonged than that of unfractionated heparin.
• Lower doses can sometimes be used: for example, for prevention of thrombosis.
Preparations of low molecular weight fragments of heparin
Preparations available at present include:
• dalteparin
• enoxaparin
• tinzaparin.
Administration
Heparin is not absorbed by mouth and is given by intravenous infusion or subcutaneous injection. The anticoagulant effect of heparin is seen within a minute or two of injection, but passes off within a few hours. Heparin is often used at the beginning of anticoagulant treatment because its effects are so rapid. Low molecular weight heparins are given once or twice daily by subcutaneous injection and the dose can be calculated from the weight of the patient.
Infusion
Infusion is given via a syringe pump. If a pump is not available, the heparin can be added to 1 litre of saline or 5% dextrose and given as an infusion. Whichever method is used, the infusion rate must be carefully controlled. The rate of infusion is monitored by measuring the kaolin cephalin time or activated partial thromboplastin time (APTT) 6 hours after starting infusion and then at least once daily; these should be kept between 1.5 and 2.5 times the control value.
The kaolin cephalin time is a method of measuring the clotting time. Platelet-poor citrated plasma is pre-incubated with kaolin, which is a surface activating agent, and a phospholipid such as cephalin, and calcium. The time taken for clotting is measured.
Subcutaneous injection
When used to prevent thrombosis, heparin is given subcutaneously twice daily.
Nursing point
Nursing point
Heparin is injected into the subcutaneous tissue of the abdominal wall via a fine needle (gauge 25, length 16 mm). An inch of skin should be picked up at the site of injection and the needle inserted perpendicularly to its full length. Local pressure is applied for 5 minutes after injection to prevent excessive bruising. Cleansing the skin before injection with isopropyl alcohol (a vasodilator) increases the chance of haematoma formation.
Adverse effects of heparin
• The only common adverse effect from heparin is bleeding due to overdose. As with all anti-coagulants, this often first appears as haematuria, but may occur from any site. The treatment is to stop the heparin.
• Prolonged use may lead to osteoporosis.
• Very rarely, severe thrombocytopenia develops, and a platelet count should be carried out if the patient receives heparin for more than 5 days.
Osteoporosis and thrombocytopenia are less commonly seen with the use of low molecular weight heparins.
Protamine sulphate, an antidote to heparin
Protamine sulphate, a basic protein, which reverses the action of heparin, can be given intravenously. This protein neutralizes the acidic heparin.
Heparinoids
The term heparinoids refers to substances similar to heparin in structure and action, and the only heparinoid in use in the UK is danaparoid sodium, which was originally extracted from porcine gut mucosa. It contains as active ingredients a low molecular weight heparin, dermatan and chondroitin. Like heparin, it acts mainly through inhibition of coagulation factor Xa. It is used to prevent deep venous thrombosis in, for example, patients undergoing orthopaedic or general surgery and for patients with a history of heparin-induced thrombocytopenia.
Fondaparinux
Fondaparinux is a cleverly designed synthetic pentasaccharide (i.e. a sugar) which is identical to the binding site for antithrombin III and acts by selectively inhibiting activated factor X. It has a significantly lower risk of thrombocytopenia than that posed by heparin. It is used, for example, in patients undergoing abdominal or major orthopaedic surgery. Fondaparinux is contraindicated in patients with impaired renal function, as it is excreted via the kidneys.
Hirudin
Hirudin was originally obtained from leeches and has been recognized as an anticoagulant for many years. It can now be made synthetically using recombinant technology. It differs from heparin in its mode of action, being a specific inhibitor of thrombin. It is given by intravenous injection or infusion. Although experience is still limited, it appears to be as effective as low molecular weight heparin, although bleeding may be a problem. The hirudins in use in the UK are bivalirudin and lepirudin.
Oral anticoagulants: the coumarins
There are two substances in this group that are used in anticoagulant treatment, namely warfarin and phenindione. Historically, this group was discovered when cows developed haemorrhage after eating spoiled sweet clover silage. The active principles were isolated and this led to the synthesis and introduction of warfarin and phenindione. They are often referred to as the oral anticoagulants, since they are active via this route of administration.
Mechanism of action of warfarin and phenindione
Warfarin and phenindione exert their anticoagulant effects by interfering with the synthesis of vitamin K-dependent clotting factors, namely factors VII, IX, X and XI.
Administration
Warfarin and phenindione are given orally in tablet form. This makes them very convenient for the patient, who can take anticoagulants at home. Their onset of action is delayed by several hours since they will only be effective after the existing stores of the vitamin K-dependent clotting factors have been depleted. For this reason, anticoagulant therapy is usually initiated with heparin, which acts immediately, followed by oral anticoagulants. Phenindione is shorter-acting than warfarin and is now rarely used.
Monitoring anticoagulant therapy
The initial stages of anticoagulation have been traditionally carried out in hospital, and thereafter controlled on an outpatient basis, but much more is now done in the community. Patients on anticoagulation therapy need to be carefully and regularly monitored for the levels of anticoagulant activity, since excessive activity can result in haemorrhage and insufficient activity can result in clotting.
The prothrombin time should be measured before starting treatment, then daily, and the dose adjusted until the INR (see below) is stabilized. The ratio:
 is known as the international normalized ratio (INR) and the dose is adjusted to keep this between 2.0 and 3.5 (depending on the clinical situation), which gives effective anticoagulation with minimal risk of bleeding.
is known as the international normalized ratio (INR) and the dose is adjusted to keep this between 2.0 and 3.5 (depending on the clinical situation), which gives effective anticoagulation with minimal risk of bleeding.
Precautions to be taken when prescribing warfarin
• The effectiveness of the drug in interfering with coagulation is measured by prothrombin time estimations.
• The patient’s age and state of health must be taken into account. For example, patients with liver disease are more sensitive to oral anticoagulants, because these are inactivated in the liver.
• Poor nutrition, heart failure, previous surgery and concurrent drugs will increase the patient’s sensitivity to warfarin and require smaller dosage.
The prothrombin time (PT) is the time taken for clotting to occur in a sample of blood to which thromboplastin and calcium have been added. (Thromboplastin is formed naturally during the early stages of coagulation, and it converts the inactive prothrombin to thrombin.)
Contraindications
Contraindications to the use of warfarin include active peptic ulcer, severe liver disease and renal failure.
Adverse effects of warfarin and phenindione
The adverse effects are:
• haemorrhage
• skin rashes, fever and jaundice (phenindione)
• teratogenic effects (fetal abnormalities).
Haemorrhage may result from overdosage, and is the most important side-effect of the coumarin group of drugs. An INR of above 5 suggests a risk of bleeding. It is best treated by withdrawal of the drug. If necessary, the effect of the anticoagulant can be reversed rapidly by an infusion of fresh frozen plasma. Alternatively, phytomenadione (vitamin K) intravenously can be given, but takes about 12 hours to become effective. Larger doses of phytomenadione interfere with further anticoagulation for some days. Very rarely, transfusion with fresh blood is required if blood loss has been excessive.
Use in pregnancy
Warfarin crosses the placenta and may cause fetal abnormalities if given in the first 3 months of pregnancy. If anticoagulation is required during pregnancy, heparin can be used throughout, or heparin used up to 16 weeks, warfarin from 16 to 36 weeks and heparin until delivery. Pre-filled syringes of heparin calcium are available for self-injection by pregnant women at home.
Drug interactions with warfarin
Interactions of oral anticoagulants with other drugs are important because even a small increase or decrease in their effectiveness may render them dangerous or useless.
Warfarin activity is increased by:




• antibiotics
• aspirin
• alcohol
• cimetidine
• dipyridamole
• phenytoin.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
