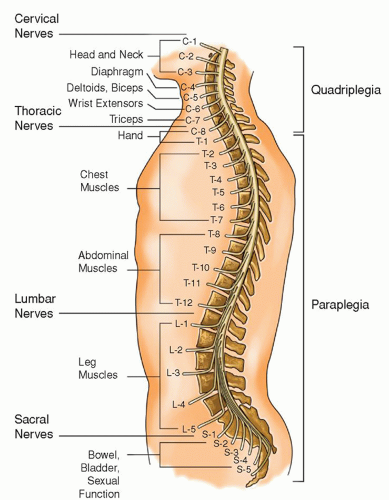
 Figure 17-1 ▪ Level of spinal cord injury and functional loss; the higher the spinal cord injury, the more motor, sensory, and autonomic functional losses are incurred. |
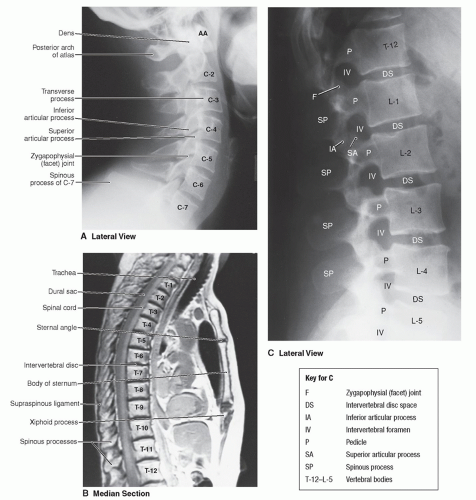
occur as a result of diving, sports, etc. Usual signs and symptoms include stiff neck, pain in the neck and shoulders, occasionally the arms, decreased cervical mobility, and muscle spasms. Other signs and symptoms may include headache that is generally described as occipital which may radiate to the forehead, paresthesias in the hands, nausea, dizziness, vertigo, and tinnitus. The findings on physical examination are normal except for the previously listed signs and symptoms. The radiologic examination is negative. If physical or radiographic examination reveals any abnormal findings, further evaluation is warranted. The diagnosis is based on the history of injury and the presence of the characteristic signs and symptoms. This is a common injury causing much pain and suffering to the patient, even though no abnormalities are noted on radiographic examination.
Mechanistic: flexion, extension, axial load, rotation, penetrating
Radiographic: compression, burst, teardrop, facet dislocation fractures
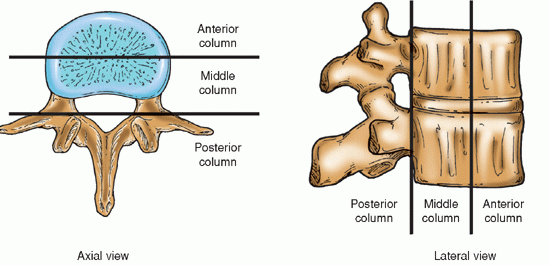
Stability or instability of injury: according to a two- or threecolumn framework
Segment of spinal column involvement: upper cervical, subaxial cervical, thoracic, thoracolumbar, lumbar, and sacral
Hyperflexion tends to produce compression of the vertebral bodies with disruption of the posterior longitudinal ligaments and the intervertebral discs. Motor vehicle crash is an example (Fig. 17-3).
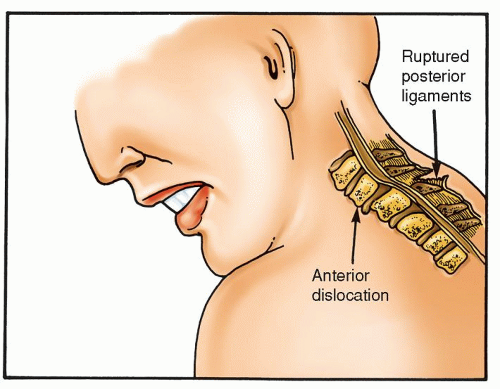
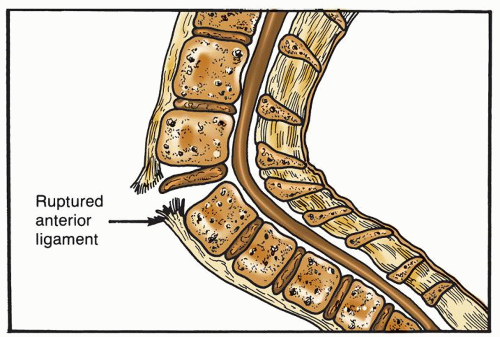
Figure 17-3 ▪ Hyperflexion injury. With hyperflexion to the cervical spine, there may be tearing of the posterior ligamentous complex, resulting in anterior dislocation.
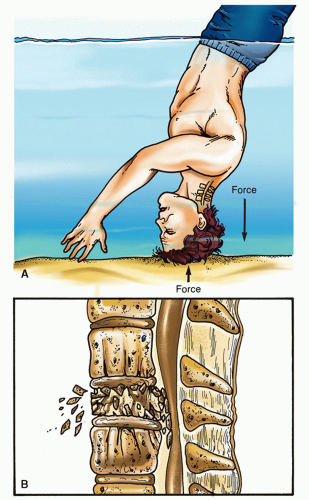
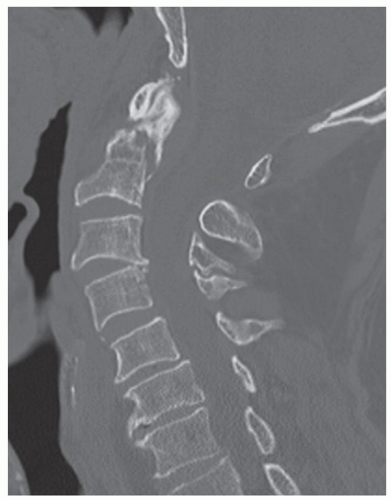
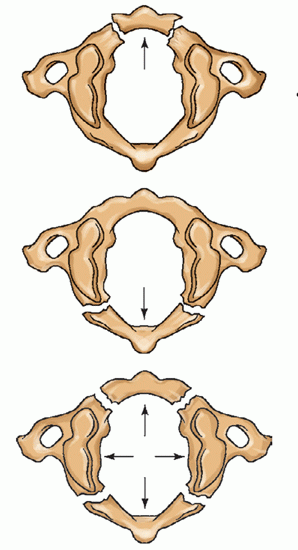
Axial loading, also known as vertical compression, occurs when a vertical force is exerted on the spinal column. Axial loading is seen in injuries resulting from diving accidents, landing on the feet when jumping from a height, or landing on the buttocks when falling from a height (Fig. 17-4).
Hyperextension usually causes fractures of the posterior elements of the spinal column and disruption of the anterior longitudinal ligaments. Falling downstairs is an example of an event leading to a hyperextension injury.
Excessive rotation refers to turning of the head beyond the normal range on the horizontal axis. This can result in compression fractures, tearing or rupture of the posterior ligament, dislocation at the facet joint, and fracture at the articular processes.
Penetrating injuries occur when missiles, such as bullets or shrapnel, or impalement instruments (knives, ice picks) penetrate the spinal column. The object may shatter bone, create bone fragments, or transect a portion or complete plane of the spinal cord or soft tissue.
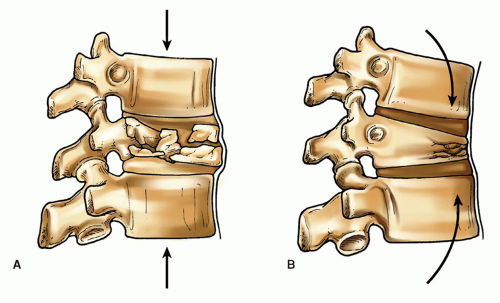
A simple compression fracture is caused by forceful axial loading or flexion and may involve the upper or the lower vertebral end plates. With a more significant injury, may involve both upper and lower endplates. There is no ligament disruption, facet injury, or subluxation. No surgery is required. These fractures heal well with a semirigid collar immobilization for about 2 months.15
Burst fractures (severe compression/axial compression injuries) are the result of axial loading with various flexions under significant forces/high energy. The result is crush injury and possible retropulsion of bone into the spinal canal. The posterior bony arch and ligamentous complex remains intact. If there is no neurological damage and if the posterior ligaments are stable, wearing a hard collar for 2 months may be adequate therapy (Fig. 17-5). However, burst fractures may require neurosurgical procedure for the removal of bone fragments, cord decompression, and spinal stabilization. Stabilization is accomplished by insertion of instrumentation, such as rods and screws to hold the spine in alignment, so that bony healing can take place. See section on surgical management for further discussion.
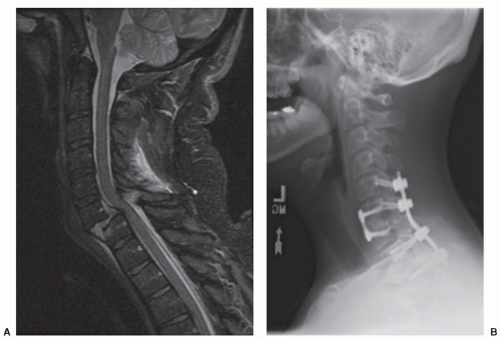
Teardrop fractures (severe compression flexion injuries) are caused by extreme flexion with axial loading. With this fracture, a vertebral body is crushed by the vertebral body superior to it, causing the anterior portion of the compressed body to break away with disruption of the posterior elements at the same time. These unstable fractures have a high rate of neurological injury and require surgical decompression and stabilization15 (Fig. 17-6 A,B).
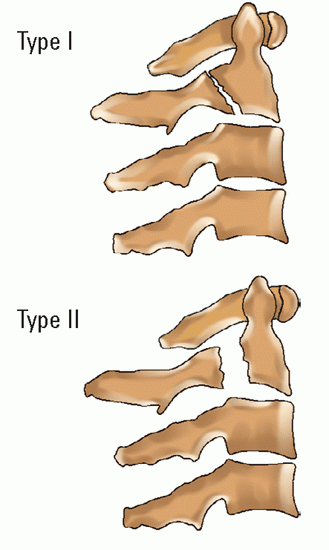
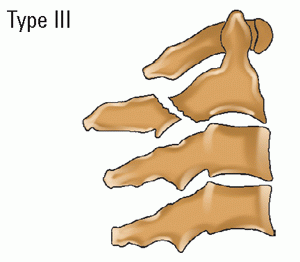
Cervical facet dislocations (distraction flexion injuries) can be unilateral or bilateral. Unilateral cervical facet dislocations usually result in approximately 25% subluxation of the upper vertebral body over the lower one. Bilateral facet dislocations often demonstrate 50% or greater subluxation. There may be associated facet fracture, disruption of the posterior ligaments, and musculature from the high-energy impact of this injury. This is an unstable injury with neurological injury common in bilateral facet dislocation. Subluxation is a partial or incomplete dislocation of one vertebra over another. Damage to the cord and supporting ligaments may or may not be present. With dislocation, re-establishment of alignment is necessary. This may be accomplished by traction followed by surgical stabilization with internal stabilization and fusion.15, 16
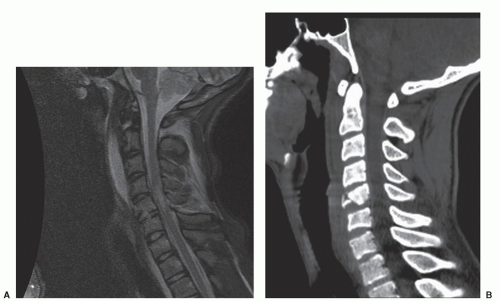
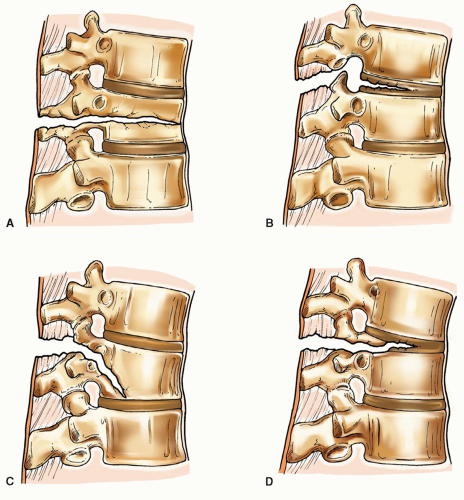
Hyperextension injuries (distraction extension injuries) demonstrate disruption of the anterior longitudinal ligament and disc from forced hyperextension. This is often seen in elderly patients who have a stiff spine, and a low energy fall places forces to the injury site. In more severe cases, there may also be posterior element disruption. Most require surgical stabilization15, 16 (Fig. 17-7).
nurses will hear much discussion about the clinical stability or conversely instability of the spinal column, which influences the medical and surgical management of the patient.
CHART 17-1 The Two- and Three-Column Frameworks: Spinal Stability and Instability | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||
Wedge compression fractures, caused by axial load in flexion, are common in the thoracic and upper lumbar spine. Wedge compression fractures involve the anterior column. Typically, neurologically intact, bracing, and pain management is generally the treatment.
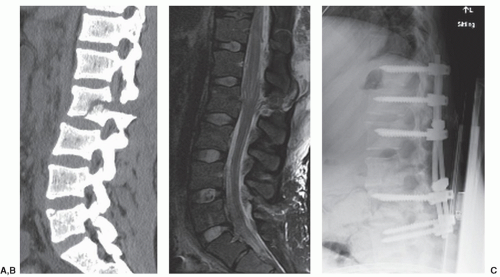
Burst fractures, caused by axial loads, involve the anterior and middle column with varying amounts of retropulsed bone fragments into the spinal canal. If the posterior column is also involved, the injury is unstable and warrants surgical intervention. Neurological injury is variable. If neurological deficits are present, emergent surgical decompression and stabilization is warranted.
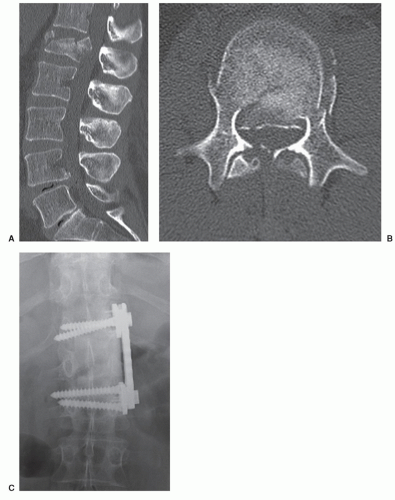
Flexion-distraction injuries (also called Chance fractures) involve the middle and posterior columns with sparing of the anterior longitudinal ligament. The fracture can extend through the posterior elements, pedicle, and vertebral body or can be a ligamentous injury through the posterior ligamentous complex and the disc annulus complex. The mechanism of injury is acute flexion of the torso, for example, while restrained with only a lap belt. The flexion-distraction injuries (Chance fractures; Fig. 17-13) are classified according to the involvement of bone and soft-tissue components. These fractures are unstable and require surgical stabilization.
Fracture-dislocations are the result of high energy rotational forces, translational forces, or a combination of both. Fractures of this type are unstable, and involve all three columns. Patients generally suffer neurological sequela. In addition, abdominal organ and vascular injury are associated with this fracture type.
low-energy falls from standing height have been implicated in sacral and coccyx fractures in the elderly and those with osteoporosis. Nerve injury in this region can range from a single nerve root to the entire cauda equina. Neurological sequela can cause bladder, bowel, or sexual dysfunction and saddle anesthesia.21
TABLE 17-1 CERVICAL VERTEBRAL INJURIES | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||
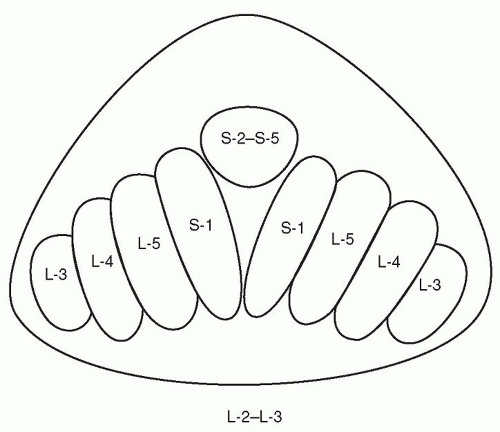
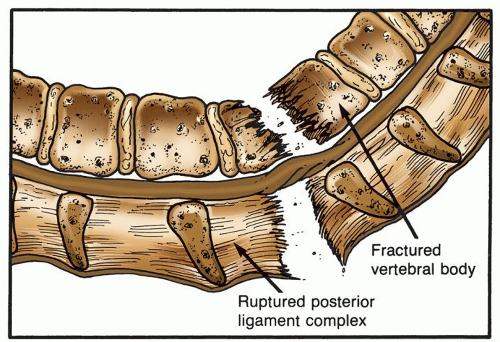 Figure 17-10 ▪ Rotational injury. High-energy forces are applied from multiple directions creating a severe, unstable injury. Spinal cord and/or cauda equina injury often accompanies this injury. |
TABLE 17-2 THORACIC/THORACOLUMBAR/LUMBAR | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
incontinence. Further examination in bed demonstrated diminished rectal tone and perianal sensation. He underwent emergent L-1 corpectomy to decompress the conus medullaris and cauda equina, and stabilization with instrumentation spanning T-12 to L-2. At discharge, he had continued weakness in bilateral lower extremities with hip strength 3/5; knee extensors, dorsiflexion and plantarflexion 4/5. His sensation was intact, however, he had continued urinary retention. At 2 weeks after surgery, lower extremity strength was full, he was ambulating without difficulty. Bowel management was improved, however, a self-catheterization program continued. At 1 year after injury, he was working full time at his usual with adequate sexual and bowel function. However, self-catheterization continued to be necessary (Fig. 17-14).
those who do not. Chronic conditions, such as cervical spondylosis, spinal stenosis, arthritis, and scoliosis, are examples of conditions that increase the probability of injury.
Concussion: causes a transient paralysis and/or sensory changes that subside within 2 to 3 days.23 No identifiable macro-neuropathological changes are noted on examination of the cord.
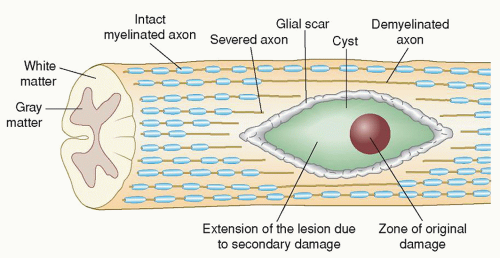
Contusion: results from direct, acute compression of the spinal cord from bone or disc depending on the severity and factors such as continued compression, which leads to the secondary injury described below. The complex cascade of secondary injury includes vascular dysfunction, edema, ischemia, excitotoxicity, inflammation, electrolyte imbalance and shifts, free radical production, and delayed apoptotic cell death. The events of secondary injury spread in all directions within the spinal cord.8
Compression: can occur from distortion of the normal curvatures, ligaments, disc herniation, or bone fragments putting direct pressure onto the spinal cord subsequent to SCI.
Shear: results from forces applied in a horizontal (anteroposterior) plane as with subluxation (one vertebral body moving forward on the one below it). It also occurs in sudden forceful hyperextension (an elderly person falling and hitting their chin). A “pincer-like” action of the spinal cord being pulled over a spondylotic spine can occur, creating shear (horizontal) stresses in the center of the cord.9
Laceration: an actual tear in the cord results in permanent injury to the cord; may be the result of penetration of an object, or overstretching of the spinal cord. Secondary injury accompanies a laceration.
Transection: a more severe form of laceration, severing of the cord can be complete or incomplete. Actual complete transection is rare. However, clinical presentations, which mimic complete transection, are frequently seen.
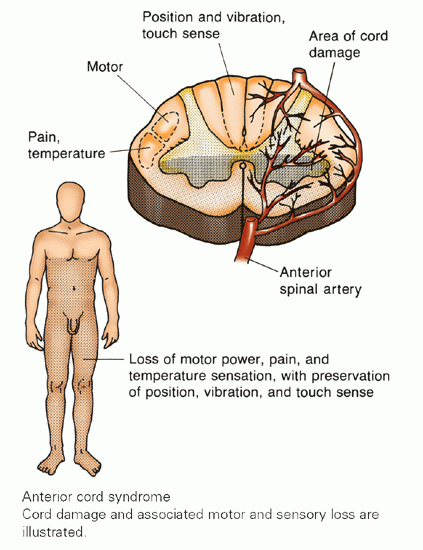
Injury to the blood vessels that supply the cord: interference with or injury to the vessels that supply the spinal cord, the anterior spinal artery, or the two posterior spinal arteries results in ischemia and secondary injury.
endothelial damage in vessels that were damaged all contribute to the deleterious secondary injury cascade. The release of proteolytic and lipolytic enzymes from the injured cells causes vasospasm, delayed swelling, and necrosis in the spinal cord.
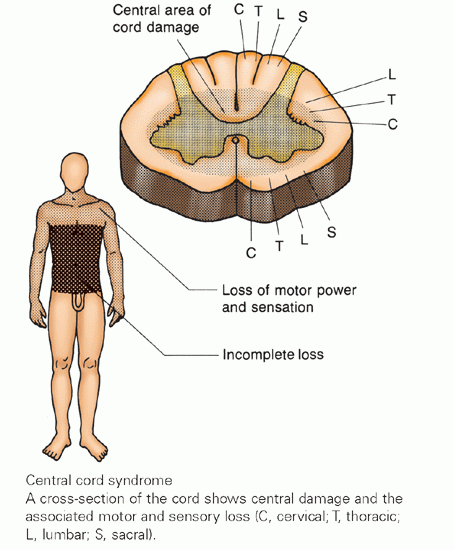
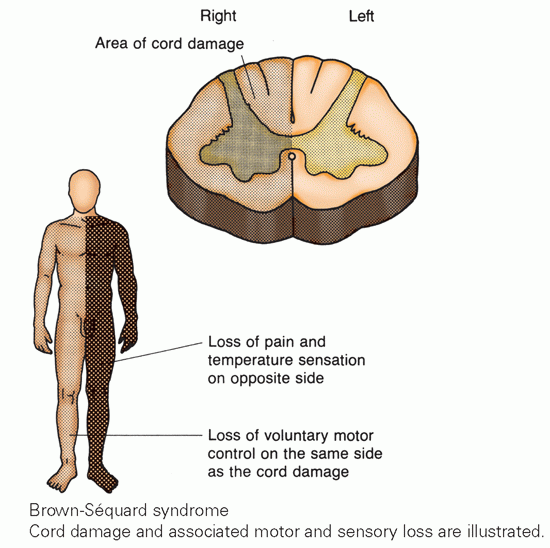
CHART 17-2 Spinal Cord Injury Syndromes | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||
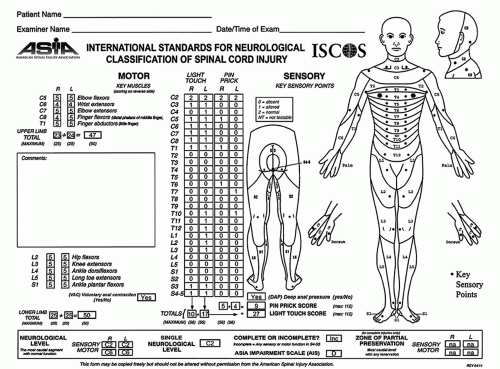
TABLE 17-3 ASIA IMPAIRMENT (AIS) SCALE | |||
|---|---|---|---|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree