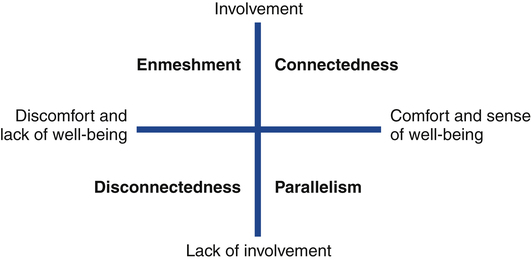
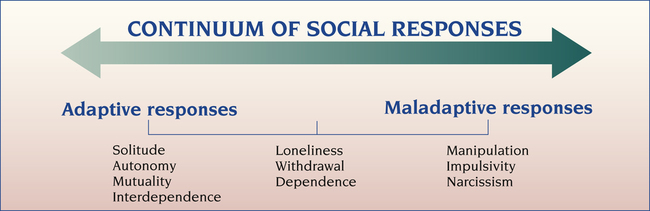
1. Describe the continuum of adaptive and maladaptive social responses. 2. Identify behaviors associated with social responses. 3. Analyze predisposing factors, precipitating stressors, and appraisal of stressors related to social responses. 4. Describe coping resources and coping mechanisms related to social responses. 5. Formulate nursing diagnoses related to social responses. 6. Examine the relationship between nursing diagnoses and medical diagnoses related to social responses. 7. Identify expected outcomes and short-term nursing goals related to social responses. 8. Develop a patient education plan to promote adaptive social responses. 9. Analyze nursing interventions related to social responses. A person’s relationships with others can be analyzed based on the degree of involvement, comfort, and well-being (Figure 21-1): • Connectedness indicates that the person is actively involved in satisfying relationships. It involves high levels of belonging, mutuality, reciprocity, and interdependence. • Disconnectedness relates to a lack of involvement that is not satisfactory to the person. • Parallelism is a lack of involvement that is comfortable and acceptable to the individual. • Enmeshment occurs when the person is involved in relationships but is unable to maintain a unique sense of self and ego boundaries. Interpersonal relationship behaviors may be represented on a continuum that ranges from healthy interdependent interactions to those involving no real contact with other people (Figure 21-2). At the midpoint of the continuum, a person experiences loneliness, withdrawal, and dependence. The maladaptive end of the continuum includes the behaviors of manipulation, impulsiveness, and narcissism. People with these responses often have a history of problematic relationships in the family, on the job, and in the social arena. Change continues during late adulthood. Losses occur, such as the physical changes of aging, the death of parents, loss of occupation through retirement, and later the deaths of friends and one’s spouse. This can result in loneliness or eccentric behavior (Magoteaux and Bonnivier, 2009; Theeke, 2009). The need for relatedness still must be satisfied. The mature person grieves over these losses and recognizes that the support of others can help resolve the grief. Personality is a set of deeply ingrained, enduring patterns of thinking, feeling, and behaving. A personality disorder is a set of patterns or traits that hinder a person’s ability to maintain meaningful relationships, feel fulfilled, and enjoy life (Newton-Howes et al, 2008). It begins in adolescence or early adulthood, is stable over time, and leads to distress or impairment (Oldham, 2005). The following are three key features of personality disorders: 1. The individual has an inflexible and maladaptive approach to relationships and the environment. 2. The individual’s needs, perceptions, and behavior tend to foster cycles that promote unhelpful patterns and provoke negative reactions from others. 3. The individual’s coping skills are unstable and fragile, and there is a lack of resilience when faced with stressful situations. It is estimated that about 4% of the general population and as many as 20% in clinical populations have personality disorders, often with significant morbidity (Kernberg and Michels, 2009). Some of these disorders are associated with a high mortality rate because of suicide. Suicide victims with personality disorders almost always also have a depressive illness, substance use disorder, or both. Many individuals with a current alcohol use disorder have at least one personality disorder, and the association is even stronger with a current drug use disorder. A comorbid personality disorder also prolongs the course of major depression (Skodol et al, 2011). Personality disorders are characterized by chronic, maladaptive social responses. The DSM-IV-TR (American Psychiatric Association, 2000) has grouped personality disorders into three clusters: 1. Cluster A includes personality disorders of an odd or eccentric nature (paranoid, schizoid, and schizotypal personality disorders). 2. Cluster B disorders are of an erratic, dramatic, or emotional nature (antisocial, borderline, histrionic, and narcissistic personality disorders). 3. Cluster C includes disorders of an anxious or fearful nature (avoidant, dependent, and obsessive-compulsive personality disorders). Antisocial personality disorder is a complex disorder that is difficult to diagnose and treat. To meet DSM-IV-TR criteria, an individual must be at least 18 years old but must demonstrate a pattern of breaking rules since the age of 15 (American Psychiatric Association, 2000). The diagnosis is applied when an individual consistently ignores social rules; is manipulative, exploitative, or dishonest; lacks remorse for actions; and is involved in criminal activity. Although this diagnosis occurs in only 3% of men and 1% of women, these individuals are responsible for a large proportion of crime, violence, and social distress. The diagnosis of borderline personality disorder occurs in 1% to 6% of the general population and is the most prevalent personality disorder (15% to 25%) in mental health settings (Gunderson, 2009). The diagnosis is made more often in women than in men. Developmental theory suggests that the borderline person does not achieve object constancy during the separation-individuation stage of psychosocial development. People who fail to complete separation from the mother (or primary caretaker) and develop autonomy in childhood often repeat this developmental crisis at adolescence. Behaviors characteristic of this phase include the following: People with narcissistic personality disorders have fragile self-esteem, driving them to search constantly for praise, appreciation, and admiration (Kay, 2008; Ronningstam, 2011). The following clinical example demonstrates narcissistic entitlement, which describes an egocentric attitude, envy, and rage when others are seen as critical or not supportive. The behaviors related to maladaptive social responses are summarized in Table 21-1. Patients often exhibit combinations of these behaviors. The nurse should be able to identify the complex behaviors associated with high levels of stress and anxiety. In some cases a usual mode of behavior, such as manipulation, may be exaggerated or combined with a change in behavior. TABLE 21-1 BEHAVIORS RELATED TO MALADAPTIVE SOCIAL RESPONSES
Social Responses and Personality Disorders
Continuum of Social Responses
Adaptive and Maladaptive Responses
Development Through the Life Cycle
Late Adulthood
Assessment
Behaviors
Manipulation
Narcissism
BEHAVIOR
CHARACTERISTICS
Manipulation
Others are treated as objects
Relationships center around control issues
Person is self oriented or goal oriented, not other oriented
Narcissism
Fragile self-esteem
Constant seeking of praise and admiration
Egocentric attitude
Envy
Rage when others are not supportive
Impulsivity
Inability to plan
Inability to learn from experience
Poor judgment
Unreliability
Social Responses and Personality Disorders
Get Clinical Tree app for offline access