CHAPTER 29 Jodie Flynn and Margaret Jordan Halter 1. Define sexual assault, sexual violence, rape, and attempted rape. 2. Discuss the implications for the underreporting of sexual assault. 3. Describe the profile of the victim and the perpetrator of sexual assault. 4. Distinguish between the acute and long-term phases of the rape-trauma syndrome, and identify some common reactions during each phase. 5. Identify five areas to assess when working with a person who has been sexually assaulted. 6. Analyze personal thoughts and feelings regarding rape and its impact on survivors. 7. Formulate two long-term outcomes and two short-term goals for the nursing diagnosis posttrauma syndrome. 8. Identify six overall guidelines for nursing interventions related to sexual assault. 9. Describe the role of the sexual assault nurse examiner to a colleague. 10. Discuss the long-term psychological effects of sexual assault that might lead a patient to seek psychological care. 11. Identify three outcome criteria that would signify successful interventions for a person who has suffered a sexual assault. Visit the Evolve website for a pretest on the content in this chapter: http://evolve.elsevier.com/Varcarolis The Federal Bureau of Investigation (FBI) (2008) considers rape to be the second-most violent crime in a group of crimes that includes murder, robbery, and aggravated assault. Victims are traumatized, both physically and emotionally, and are often seen in health care settings. Nurses are instrumental in providing holistic care for those who have been sexually assaulted and also in helping to preserve evidence. Preservation of evidence can lead to the prosecution of a crime or the exoneration of a person of interest; therefore, it is essential that nurses be informed adequately about their roles and responsibilities with regard to providing both medical and legal care and ensuring that nursing policies and procedures effectively manage the care of sexual assault patients. Nearly 1 in 5 women and 1 in 71 men in the United States have been raped at some time in their lives (Black, et al., 2011). According to the National Intimate Partner and Sexual Violence Survey (NISVS) (2011), most female victims will experience their first rape before the age of 25, with 42.2% reporting a rape before the age of 18 years. More than one quarter of male victims experienced their first rape when they were 10 years of age or younger. Each year, women experience about 4.8 million intimate partner-related physical assaults and rapes (Centers for Disease Control, 2011). Lifetime prevalence of rape is 18% among U.S. adult women, and few rape survivors seek immediate medical attention, even with serious injury (Tjaden & Thomas, 2008). For male victims, more than half (52.4%) reported being raped by an acquaintance and 15.1% by a stranger (Black et al., 2011). A male who is raped is more likely to experience physical trauma and to have been victimized by several assailants. Reports of male-to-male rape occur primarily in locked institutions, such as prisons and maximum-security hospitals. Males experience the same devastation, physical injury, and emotional consequences as females. Although they may cover their responses, they too benefit from care and treatment. Precise estimates of sexual violence are impossible since this crime is greatly underreported, but there is reason for optimism. According to the 2011 FBI Uniform Crime Reporting Program, there was a decrease of about 5% for a majority of population groups. A reduction of sexual assault cases is part of an overall trend that may be due to several factors: policies that support longer sentences for perpetrators, mandatory sentences, and trained health care providers who specialize in caring for victims of sexual assault. Women and men today may be willing to report sexual violence, which may be a deterring factor. Females know their offenders in almost 70% of all violent crimes committed against them; males know their offenders 45% of the time (Truman & Rand, 2010). Acquaintance (or date) rape has increased in incidence in the United States in recent years, with drugs, often combined with alcohol, being used to commit sexual assault. Date-rape drugs may render a woman incapable of resisting the attack and are purported to facilitate acquaintance rape. Often these drugs are given to the unknowing victim. Once the drugs are ingested, victims lose their ability to ward off attackers, develop amnesia, and become unreliable witnesses. Because the symptoms mimic those of alcohol, victims are not always screened for these drugs. The increase in prevalence and incidence of drug-assisted rape led to the passage of the Drug-Induced Rape Prevention and Punishment Act in 1996. This law allows up to 20 years imprisonment and fines for anyone who intends to commit a violent crime by administering a controlled substance to an unknowing individual (U.S. Department of Justice, 1997). Table 29-1 provides information about date-rape drugs. TABLE 29-1 DRUGS ASSOCIATED WITH DATE RAPE *Two other benzodiazepines, clonazepam (Klonopin) and alprazolam (Xanax), are also used. Data from Lehne, R. A. (2010). Pharmacology for nursing care (7th ed.). Philadelphia, PA: Saunders; U.S. Department of Health and Human Services. (2008). Date rape drugs. Retrieved from http://www.womenshealth.gov/faq/date-rape-drugs.cfm. Acute stress disorder is a psychological reaction to a serious trauma, such as witnessing a death, suffering a serious injury, or a sexual violation. Those who suffer from acute stress disorder following sexual assault are at an increased risk for psychological problems as a result of that trauma (Gaffney, 2011). Acute stress can lead to posttraumatic stress disorder (PTSD) if symptoms extend beyond 1 month. According to the National Institute of Mental Health (2009), PTSD symptoms can be grouped into three main categories: 1. Reexperiencing: Repeated reliving of the event that interferes with daily activity. This category includes flashbacks, frightening thoughts, recurrent memories or dreams, and physical reactions to situations that remind you of the event. 2. Avoidance: Changing routines to escape similar situations to the trauma. Victims might avoid places, events, or objects that remind them of the experience. Emotions related to avoidance are numbness, guilt, and depression. Some have a decreased ability to feel certain emotions, such as happiness. They also might be unable to remember major parts of the trauma and feel that their future offers fewer possibilities than other people have. 3. Hyperarousal: Difficulty concentrating or falling asleep, being easily startled, feeling tense, and angry outbursts. These can combine to make it difficult for victims to complete normal daily tasks. Most people who are raped suffer severe and long-lasting emotional trauma. Long-term psychological effects of sexual assault may include depression, suicide, anxiety, and fear; difficulties with daily functioning; low self-esteem; sexual dysfunction; and somatic complaints. Victims of incest may experience a negative self-image, depression, eating disorders, personality disorders, self-destructive behavior, and substance abuse. A history of sexual abuse in psychiatric patients is associated with a characteristic pattern of symptoms that may include depression, anxiety disorders, chemical dependency, suicide attempts, self-mutilation, compulsive sexual behavior, and psychosis-like symptoms (Read et al., 2007). According to the Centers for Disease Control and Prevention (2010), sexual assault represented 8% of all nonfatal violence-related injury visits to emergency departments for females in 2008. According to the U.S. Department of Justice, 32% of sexual assault victims seek help in a hospital emergency department. The attention the patient receives depends on the policy of the health care facility. The U.S. Department of Justice (2004) publishes A National Protocol for Sexual Assault Medical/Forensic Examinations to assist health care facilities in establishing protocols in caring for adult and adolescent sexual assault patients. This protocol has been instrumental in guiding care toward a more comprehensive approach to sexual assault care. According to the protocol, the medical exam should include the following: The Emergency Nurses Association (2010) position statement on care of sexual assault and rape victims suggests: 1. An individualized, multidisciplinary, multiagency approach. 2. A physical and social environment conducive to private, empathetic, and unbiased care by health care providers, family members, law enforcement officers, and members of the justice system. 3. A private and safe environment, with personnel limited to examining health care providers during sexual assault care. Translators must be available if needed. With the consent of the patient, a specially trained advocate also may be present. 4. Comprehensive, competent, and sensitive emergency health care. 5. Employment of SANE nurses in the emergency department is highly recommended. 6. Emergency nurses should collaborate to promote and establish ongoing community education focused on preparing the public and emergency nurses to better identify, prevent, care for, and report incidents of sexual assault and rape. 7. Emergency nurses should be involved in research concerning the identification, assessment, and treatment of victims of sexual assault and rape. The care of sexual assault victims varies from facility to facility. In one Midwestern study, researchers found that virtually all emergency departments provided acute medical care (Patel et al., 2008); however, only two thirds of these agencies offered rape counseling and sexually transmitted infection management. Counseling and emergency contraceptives were provided by 40% of facilities, and HIV management was provided by 30% of the facilities. Just 10% of the emergency departments provided all of these services to victims of sexual assault. Patients experiencing severe-to-panic levels of anxiety will not be able to problem solve or process information. Support, reassurance, and appropriate therapeutic techniques can lower the patient’s anxiety and facilitate mutual goal setting and the assimilation of information. Refer to Chapters 10 and 15 for more detailed discussions of the levels of anxiety and therapeutic interventions. If suicidal thoughts are expressed, ask direct questions, such as “Are you thinking of harming yourself?” or “Have you ever tried to kill yourself before or after this attack occurred?” If the answer is yes, the nurse conducts a thorough suicide assessment (plan, means to carry it out), as described in Chapter 25.
Sexual assault
Epidemiology
Sexual offenders and relationships with victims
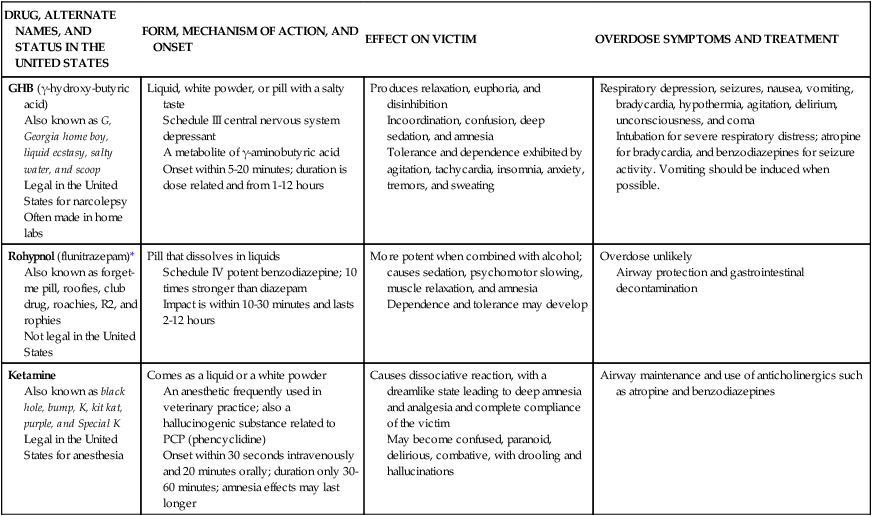
DRUG, ALTERNATE NAMES, AND STATUS IN THE UNITED STATES
FORM, MECHANISM OF ACTION, AND ONSET
EFFECT ON VICTIM
OVERDOSE SYMPTOMS AND TREATMENT
GHB (γ-hydroxy-butyric acid)
Also known as G, Georgia home boy, liquid ecstasy, salty water, and scoop
Legal in the United States for narcolepsy
Often made in home labs
Liquid, white powder, or pill with a salty taste
Schedule III central nervous system depressant
A metabolite of γ-aminobutyric acid
Onset within 5-20 minutes; duration is dose related and from 1-12 hours
Produces relaxation, euphoria, and disinhibition
Incoordination, confusion, deep sedation, and amnesia
Tolerance and dependence exhibited by agitation, tachycardia, insomnia, anxiety, tremors, and sweating
Respiratory depression, seizures, nausea, vomiting, bradycardia, hypothermia, agitation, delirium, unconsciousness, and coma
Intubation for severe respiratory distress; atropine for bradycardia, and benzodiazepines for seizure activity. Vomiting should be induced when possible.
Rohypnol (flunitrazepam)*
Also known as forget-me pill, roofies, club drug, roachies, R2, and rophies
Not legal in the United States
Pill that dissolves in liquids
Schedule IV potent benzodiazepine; 10 times stronger than diazepam
Impact is within 10-30 minutes and lasts 2-12 hours
More potent when combined with alcohol; causes sedation, psychomotor slowing, muscle relaxation, and amnesia
Dependence and tolerance may develop
Overdose unlikely
Airway protection and gastrointestinal decontamination
Ketamine
Also known as black hole, bump, K, kit kat, purple, and Special K
Legal in the United States for anesthesia
Comes as a liquid or a white powder
An anesthetic frequently used in veterinary practice; also a hallucinogenic substance related to PCP (phencyclidine)
Onset within 30 seconds intravenously and 20 minutes orally; duration only 30-60 minutes; amnesia effects may last longer
Causes dissociative reaction, with a dreamlike state leading to deep amnesia and analgesia and complete compliance of the victim
May become confused, paranoid, delirious, combative, with drooling and hallucinations
Airway maintenance and use of anticholinergics such as atropine and benzodiazepines
Clinical picture
Psychological effects of sexual assault
Application of the nursing process
Assessment
General assessment
Level of anxiety
Signs and symptoms of emotional trauma
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Sexual assault
Get Clinical Tree app for offline access
