Chapter 25. Sera and vaccines
LEARNING OBJECTIVES
At the end of this chapter, the reader should be able to:
• list the basic components of the immune system
• explain humoral and cell-mediated immunity
• explain active and passive immunization
• describe how these immunizations are achieved
• state the dangers and precautions associated with the administration of serum
• state what is meant by antiserum
• describe the immunization schedules used to protect against hepatitis A and B
The immune reaction
The human body is continually subjected to the risk of infection by microorganisms (bacteria, viruses, fungi) and to damage by toxins produced by bacteria. These foreign substances are known collectively as antigens.
The cells that recognize and react to antigens are called lymphocytes. They are distributed throughout the body in blood, lymph and lymphoid tissues (spleen, lymph nodes, tonsils and adenoids). All lymphocytes originate in the bone marrow, but there are two main groups, the B and T cells, which mature differently and help to defend the body against foreign antigens in different ways (Fig. 25.1).
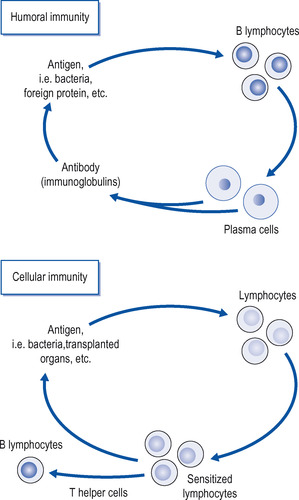 |
| Figure 25.1 The sequence of events in the production of humoral and cellular immunity. |
Cell-mediated immunity
Cell-mediated immunity is a property of the T lymphocytes, which mature in the thymus gland before they enter the circulation. T lymphocytes do not produce antibodies, but are an essential component of the immune response, as B lymphocytes require them to function properly. Some T lymphocytes (T helper cells) appear to play an important part by ‘switching on’ the immune response when antigens invade, while others ‘switch off’ the immune response when the body no longer requires it. Cell-mediated immunity is especially important in the rejection of foreign materials such as transplanted organs, and in chronic infections such as tuberculosis. People whose cell-mediated immunity is impaired by HIV infection, which destroys the T helper cells, become very prone to fungal and protozoan infections, which T lymphocytes usually keep in check.
Active immunization
The principle of this method is to promote the production by the patient of antibodies or sensitized lymphocytes to bacteria or toxins produced by bacteria before infection occurs. If the patient then becomes infected, the antibodies are quickly produced and are capable of rapidly dealing with the infecting organism or its toxin and thus preventing or minimizing the disease.
Antibodies are usually produced by injecting the patient with killed or modified bacteria, which, although harmless, are still capable of producing antibodies. These organisms are known as a vaccine. A good example of this method is the widespread immunization against poliomyelitis by the Sabin vaccine, which is a live virus that has been attenuated (rendered harmless).
Similarly, bacterial toxins may be modified to produce toxoids which are no longer harmful but which are capable of acting as antigens. They are then injected and protect against future damage from the particular toxin. Good examples of toxoids are the various diphtheria toxoids that produce immunity to the very dangerous toxin produced by the diphtheria organism ( Corynebacterium diphtheriae).
Following injection of the antigen, whether vaccine or toxoid, there is usually an interval of a few days before antibodies appear. These antibodies may then persist for varying periods, from a few months up to many years. It is often the practice to give two or more booster injections of the antigen to produce a higher level of immunity.
Active immunization is used in the prevention of the following diseases:
| measles | whooping cough |
| rabies | tetanus |
| pneumococcal | typhoid (not often) |
| infections | typhus |
| Anthrax | tuberculosis |
| meningitis | cholera |
| influenza | yellow fever |
| mumps | smallpox (rare) |
| rubella | hepatitis A and B |
| diphtheria | varicella |
Active immunization may take several weeks before enough antibodies are produced to be effective. This is satisfactory as a prophylactic measure, but is not much good to treat established disease. Under these conditions, passive immunization is used.
Passive immunization
In this method of immunization, the appropriate antibody against the invading organism or toxin is injected. In the past, this antibody was produced on a large scale in animals by injecting an antigen, either vaccine or toxoid, until a high blood level of antibody was obtained. Some of the blood was then removed and the antibody extracted and stored until required. Following the injection of antibody, immunity will last about 2 weeks. This method suffers from the disadvantage that it is not possible to purify the antibodies produced completely and there is therefore a risk of a hypersensitivity reaction. Nowadays, genetic engineering and cloning procedures mean that antibodies can be grown in vitro.
Certain types of antibody can be obtained from human blood, either after the subject has been actively immunized or has suffered a particular infection. These antibodies, usually called human immunoglobulins, are safer and rarely produce a serious reaction, although there may be discomfort at the injection site.
Common examples of animal- and human-derived antibodies are, respectively, diphtheria antitoxin, which was obtained from horse serum, and antitetanus immunoglobulin injection from human blood.
Administration of serum
Antitoxin raised in animals, often called antiserum, carries a real risk of a hypersensitivity reaction. This is particularly liable to occur in patients who have had previous serum injections or who suffer from allergic disorders (e.g. asthma). The reaction occurs because the antibody in the serum reacts with antigens already present in the patient, releasing histamine and other substances. Serum reactions take two forms:
Nursing point
• Immediate or anaphylactic reaction: within a few minutes of injection the patient collapses with difficulty in breathing, low blood pressure and, sometimes, widespread urticaria. Rarely it can be fatal.
• Serum sickness occurs about a week after injection of serum. This is a delayed reaction. The patient is pyrexial with a rash and arthritis. It clears up in a few days.
Nursing point
Sera and vaccines should be kept in a refrigerator at the correct temperature. Guidelines are given in Immunisation against infectious disease (Department of Health 1996).
Precautions when injecting serum
Ask the patient:




• Have you had serum before?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
