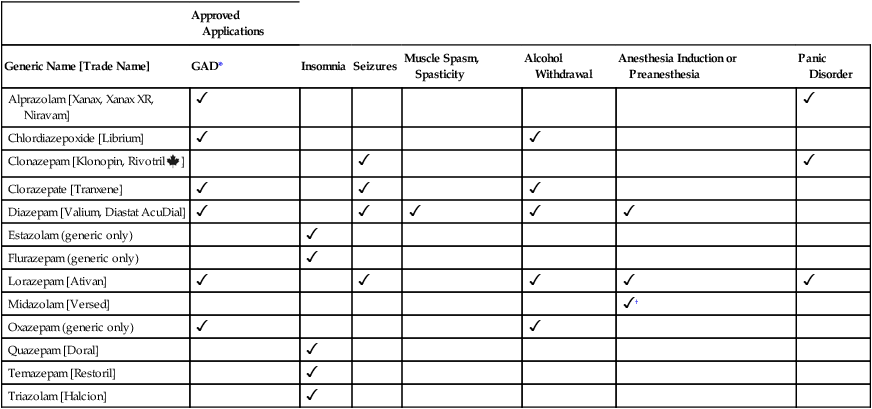
CHAPTER 34 We begin the chapter by discussing the basic pharmacology of the sedative-hypnotics, and end by discussing their use in insomnia. Use of these drugs for anxiety disorders is addressed in Chapter 35. The popularity of the benzodiazepines as sedatives and hypnotics stems from their clear superiority over the alternatives: barbiturates and other general CNS depressants. The benzodiazepines are safer than the general CNS depressants and have a lower potential for abuse. In addition, benzodiazepines produce less tolerance and physical dependence and are subject to fewer drug interactions. Contrasts between the benzodiazepines and barbiturates are summarized in Table 34–1. TABLE 34–1 Contrasts Between Benzodiazepines and Barbiturates *Although dependence is low in most patients, significant dependence can develop with long-term, high-dose use. Benzodiazepines potentiate the actions of gamma-aminobutyric acid (GABA), an inhibitory neurotransmitter found throughout the CNS. These drugs enhance the actions of GABA by binding to specific receptors in a supramolecular structure known as the GABA receptor–chloride channel complex (Fig. 34–1). Please note that benzodiazepines do not act as direct GABA agonists—they simply intensify the effects of GABA. The benzodiazepines have three principal indications: (1) anxiety, (2) insomnia, and (3) seizure disorders. In addition, they are used as preoperative medications and to treat muscle spasm and withdrawal from alcohol. Although all benzodiazepines share the same pharmacologic properties, and therefore might be equally effective for all applications, not every benzodiazepine is actually employed for all potential uses. The principal factors that determine the actual applications of a particular benzodiazepine are (1) the pharmacokinetic properties of the drug itself and (2) research and marketing decisions of pharmaceutical companies. Specific applications of individual benzodiazepines are summarized in Table 34–2. TABLE 34–2 Applications of the Benzodiazepines *GAD = generalized anxiety disorder. †Midazolam, in conjunction with an opioid analgesic, is also used to produce conscious sedation, a semiconscious state suitable for minor surgeries and endoscopic procedures. Benzodiazepines are drugs of first choice for anxiety. Although all benzodiazepines have anxiolytic actions, only six are marketed for this indication (see Table 34–2). Anxiolytic effects result from depressing neurotransmission in the limbic system and cortical areas. Use of benzodiazepines to treat anxiety disorders is discussed in Chapter 35.
Sedative-hypnotic drugs
Benzodiazepines

Area of Comparison
Benzodiazepines
Barbiturates
Relative safety
High
Low
Maximal ability to depress CNS function
Low
High
Respiratory depressant ability
Low
High
Suicide potential
Low
High
Ability to cause physical dependence
Low*
High
Ability to cause tolerance
Low
High
Abuse potential
Low
High
Ability to induce hepatic drug metabolism
Low
High
Molecular mechanism of action
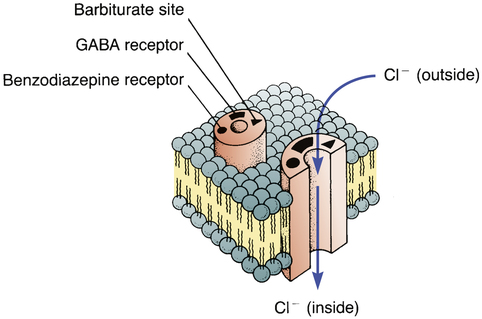
 Schematic model of the GABA receptor–chloride channel complex showing binding sites for benzodiazepines and barbiturates.
Schematic model of the GABA receptor–chloride channel complex showing binding sites for benzodiazepines and barbiturates.
The GABA receptor–chloride channel complex, which spans the neuronal cell membrane, can exist in an open or closed configuration. Binding of GABA to its receptor on the complex causes the chloride channel to open. The resulting inward flow of chloride ions hyperpolarizes the neuron (makes the cell highly negative inside) and thereby decreases its ability to fire. Hence GABA is an inhibitory neurotransmitter. Binding of a benzodiazepine to its receptor on the complex increases the frequency of channel opening, thereby increasing chloride influx. Hence, benzodiazepines enhance the inhibitory effects of GABA. In the absence of GABA, benzodiazepines have no effect on channel opening. The benzodiazepine-like drugs (zolpidem, zaleplon, and eszopiclone) have actions much like those of the benzodiazepines. Effects of barbiturates on the chloride channel are dose dependent: at low doses, barbiturates enhance the actions of GABA (by prolonging the duration of channel opening); at high doses, barbiturates directly mimic the actions of GABA.
Therapeutic uses

Approved Applications
Generic Name [Trade Name]
GAD*
Insomnia
Seizures
Muscle Spasm, Spasticity
Alcohol Withdrawal
Anesthesia Induction or Preanesthesia
Panic Disorder
Alprazolam [Xanax, Xanax XR, Niravam]


Chlordiazepoxide [Librium]


Clonazepam [Klonopin, Rivotril ![]() ]
]


Clorazepate [Tranxene]



Diazepam [Valium, Diastat AcuDial]





Estazolam (generic only)

Flurazepam (generic only)

Lorazepam [Ativan]





Midazolam [Versed]
 †
†
Oxazepam (generic only)


Quazepam [Doral]

Temazepam [Restoril]

Triazolam [Halcion]

Anxiety.
Sedative-hypnotic drugs
Get Clinical Tree app for offline access



