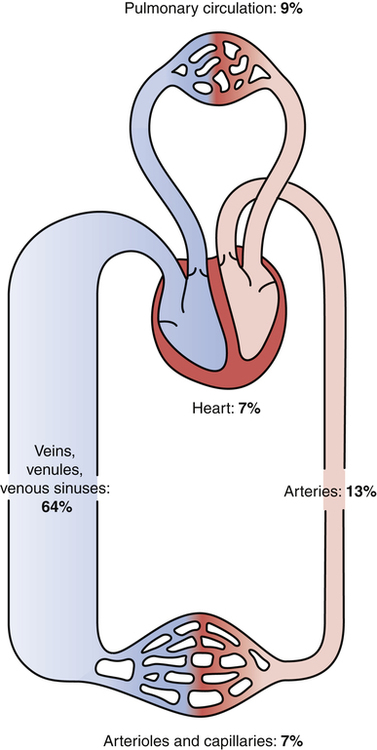
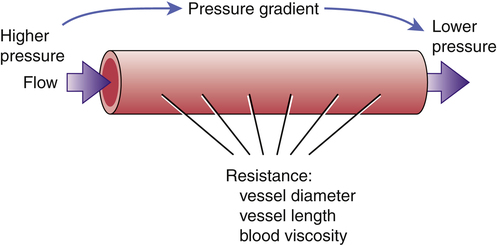
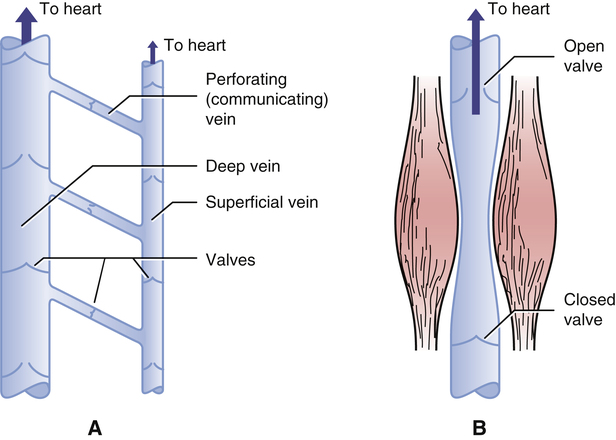
CHAPTER 43 • Arteries transport blood under high pressure to tissues. • Arterioles are control valves that regulate local blood flow. • Capillaries are the sites for exchange of fluid, oxygen, carbon dioxide, nutrients, hormones, wastes, and so forth. • Venules collect blood from the capillaries. • Veins transport blood back to the heart. In addition, veins serve as a major reservoir for blood. The adult circulatory system contains about 5 L of blood, which is distributed throughout the system. As indicated in Figure 43–1, 9% is in the pulmonary circulation, 7% is in the heart, and 84% is in the systemic circulation. Within the systemic circulation, however, distribution is uneven: most (64%) of the blood is in veins, venules, and venous sinuses; the remaining 20% is in arteries (13%) and arterioles or capillaries (7%). The large volume of blood in the venous system serves as a reservoir. Blood moves within vessels because the force that drives flow is greater than the resistance to flow. As indicated in Figure 43–2, the force that drives blood flow is the pressure gradient between two points in a vessel. Obviously, blood will flow from the point where pressure is higher toward the point where pressure is lower. Resistance to flow is determined by the diameter and length of the vessel, and by blood viscosity. From a pharmacologic viewpoint, the most important determinant of resistance is vessel diameter: The larger the vessel, the smaller the resistance. Accordingly, when vessels dilate, resistance declines, causing blood flow to increase—and when vessels constrict, resistance rises, causing blood flow to decline. In order to maintain adequate flow when resistance rises, blood pressure must rise as well. As indicated in Figure 43–3, pressure falls progressively as blood moves through the systemic circulation. Pressure is 120 mm Hg when blood enters the aorta, 30 mm Hg when blood enters capillaries, and only 18 mm Hg when blood leaves capillaries, and then drops to negative values (0 to −5 mm Hg) in the right atrium. (Negative atrial pressure is generated by expansion of the chest during inspiration.) Given that pressure is only 18 mm Hg when blood leaves capillaries, we must ask, “How does blood get back to the heart? After all, a pressure of 18 mm Hg does not seem adequate to move blood from the feet all the way up to the thorax.” The answer is that, in addition to the small pressure head in venules, three mechanisms help ensure venous return. First, negative pressure in the right atrium helps “suck” blood toward the heart. Second, constriction of smooth muscle in the venous wall increases venous pressure, which helps drive blood toward the heart. Third, and most important, the combination of venous valves and skeletal muscle contraction constitutes an auxiliary “venous pump.” As indicated in Figure 43–4A, the veins are equipped with a system of one-way valves. When skeletal muscles contract (Fig. 43–4B), venous blood is squeezed toward the heart—the only direction the valves will permit. The basic equation for cardiac output is
Review of hemodynamics
Overview of the circulatory system
Components of the circulatory system
Distribution of blood
What makes blood flow?
How does blood get back to the heart?
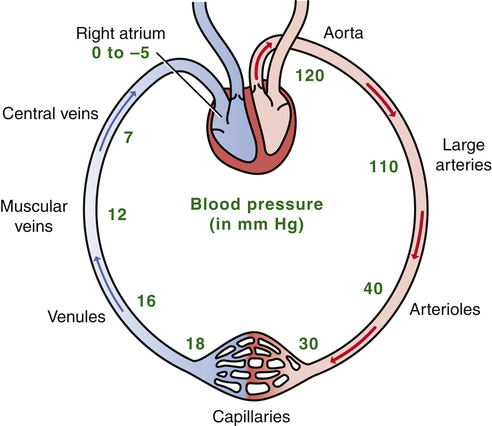
 Distribution of pressure within the systemic circulation.
Distribution of pressure within the systemic circulation.
Note that pressure is highest when blood leaves the left ventricle, falls to only 18 mm Hg as blood exits capillaries, and reaches negative values within the right atrium.
Regulation of cardiac output
Determinants of cardiac output
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Review of hemodynamics
CO = HR × SV
Only gold members can continue reading. Log In or Register to continue
Get Clinical Tree app for offline access