CHAPTER 27 Respiratory Emergencies
I. GENERAL STRATEGIES
A. Assessment
1. Primary and secondary assessment/resuscitation (see Chapter 1)
C. Planning and Implementation/Interventions
F. Age-Related Considerations
II. SPECIFIC RESPIRATORY EMERGENCIES
A. Adult Respiratory Distress Syndrome
2. Analysis: differential nursing diagnoses/collaborative problems
3. Planning and implementation/interventions
4. Evaluation and ongoing monitoring (see Appendix B)
B. Asthma
Asthma is a chronic, reversible obstructive pulmonary disease that is caused by airway inflammation and increased airway responsiveness (bronchospasm) to stimuli. Ten to 15 million persons in the United States have asthma. The disease affects more male than female patients, and it is the most common chronic childhood illness. Asthma affects approximately 5% to 10% of children and is more prevalent among lower-income, inner-city black children, children with low birth weight, children of young mothers, and those with genetic atopic disease. Two thirds of patients with asthma are diagnosed by the age of 40 years. The morbidity and mortality of asthma are increasing, causing approximately 5000 deaths per year in the United States. The death rate for asthma is greater for female patients and for African Americans.
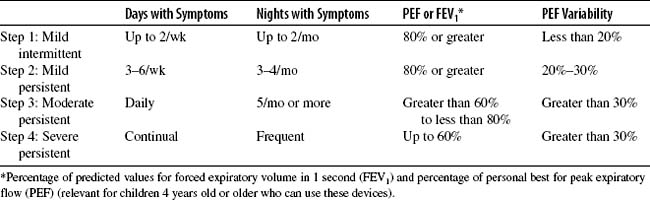
The Global Initiative for Asthma has developed a stepwise therapy model with guidelines for the successful management of long-term outpatient management of asthma. Management involves four strategies: (1) objective measures of lung function, (2) environmental control measures and avoidance of risk factors, (3) comprehensive pharmacologic therapy, and (4) patient education. Other strategies include management of exacerbations and regular follow-up care. Prior to treatment, asthma severity based on symptom prevalence and measurement of lung function needs to be established (Table 27-3).
2. Analysis: differential nursing diagnoses/collaborative problems
3. Planning and implementation/interventions
4. Evaluation and ongoing monitoring (see Appendix B)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree