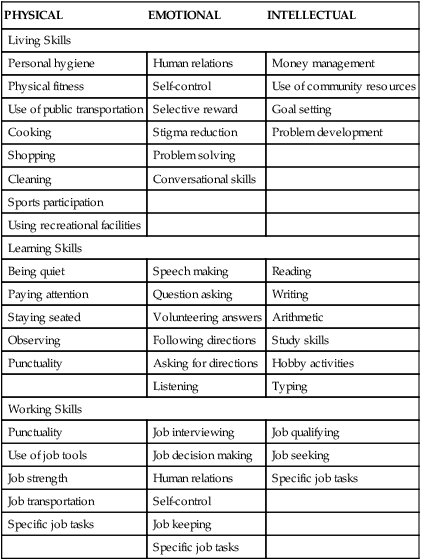
1. Define recovery and rehabilitation in psychiatric care. 2. Assess the nursing care needs of people in recovery and how families and communities respond to their needs. 3. Plan and implement recovery support of psychiatric nursing interventions with individuals, families, and communities. 4. Examine approaches to evaluate recovery support interventions related to individuals, families, and programs. Individuals who have serious mental illnesses, with the provision of appropriate and individualized supports, can recover from their illnesses and lead satisfying and productive lives. One of the eight Strategic Initiatives identified in the 2011–2014 plan of the federal Substance Abuse and Mental Health Services Administration (SAMHSA) is “Recovery Support” (SAMHSA, 2011). One-third of individuals with severe mental illnesses who receive community mental health services after lengthy stays in a state hospital fully recover, and another third improve significantly (SAMHSA, 2009). Recovery is a journey of healing and transformation enabling a person with a mental health problem to live a meaningful life in a community of his or her choice while striving to achieve his or her full potential (USDHHS, 2006). The components of recovery are described in Box 14-1. Recovery is the process in which people are able to live, work, learn, and participate fully in their communities. For some individuals, recovery is the ability to live a fulfilling and productive life despite a disability. For others, recovery implies the reduction or complete remission of symptoms. Recovery also involves connectedness, or the capacity for mutual interpersonal relationships, and citizenship, which includes the rights, privileges, and responsibilities of membership in a democratic society (Ware et al, 2007, 2008). Self-determination is the foundation of person-centered and consumer-driven recovery supports and systems. The most important aspects of recovery are defined by each individual with the help of mental health care providers and the people who are most important in each person’s life. Having hope plays an essential role in an individual’s recovery (Stuart, 2010). It grew out of a need to create opportunities for people diagnosed with severe mental illness to live, learn, and work in their own communities. Psychiatric rehabilitation uses a person-centered, people-to-people approach that differs from the traditional medical model of care as seen in Table 14-1. TABLE 14-1 COMPARISON OF PSYCHIATRIC REHABILITATION AND TRADITIONAL MEDICAL MODELS OF CARE Some mental health care providers have concerns that the focus on recovery is not realistic. However as individuals participate in recovery-oriented programs and mental health professionals observe the progress that they make, these concerns are addressed and corrected (Delaney, 2010). For example, a recovery-oriented approach to providing nursing care to individuals who are taking psychiatric medication would take into account the fact that reluctance to take medication is often related to the person’s illness or refusal to acknowledge a need for medication. The recovery-oriented response is focused on learning about the patient’s reasons for not taking medication and then working with the patient to identify ways to make medication more acceptable based on the patient’s life goals (Roe and Swarbrick, 2007). There are a number of evidence-based practices that support and enhance recovery including: assertive community treatment, supported employment, illness management and recovery, integrated treatment for co-occurring mental illness and substance abuse, family psychoeducation, medication management, and permanent supported housing. All these practices except integrated treatment for co-occurring mental illness and substance abuse (see Chapter 23) and medication management (see Chapter 26) are addressed in this chapter. The exact causes of these characteristics have not been identified. Some could be related to primary and secondary symptoms or disabilities of the illness and others to society’s reaction to the person with mental illness (Pope, 2011). Attitudes that could contribute to this reaction are illustrated by the list of myths and facts about people with mental illness seen in Box 14-2. None of these myths is true, but they are commonly believed and stigmatize people with mental illness. They also can prevent people with mental illness from gaining access to needed services and opportunities. The nursing assessment of a patient with a serious mental illness should include an analysis of the physical, emotional, and intellectual components of the skills needed for living, learning, and working in the community. Table 14-2 presents skills required for successful functioning in the community. TABLE 14-2 POTENTIAL SKILLS NEEDED IN RECOVERY SUPPORT From Anthony WA: Principles of psychiatric rehabilitation, Baltimore, 1999, University Park Press. Families and other caregivers can be a major source of support for individuals who have serious mental illnesses. They can help by identifying potential problem areas and enhancing the patient’s adherence to the treatment plan. Caregivers should be educated about the patient’s condition and involved in the treatment process. Families should be viewed as resources, caregivers, and collaborators by psychiatric nurses (see Chapter 10). • Family structure, including developmental stage, roles, responsibilities, norms, and values • Family attitudes toward the mentally ill member • The emotional climate of the family (fearful, angry, depressed, anxious, calm) • The social supports available to the family, including extended family, friends, financial support, religious involvement, and community contacts • Past family experiences with mental health services • The family’s understanding of the patient’s problem and the plan of care
Recovery Support
Recovery
ASPECT OF CARE
PSYCHIATRIC REHABILITATION
TRADITIONAL MEDICAL REHABILITATION
Focus
Focus on wellness and health, not symptoms
Focus on disease, illness, and symptoms
Basis
Based on person’s abilities and functional behavior
Based on person’s disabilities and intrapsychic functioning
Setting
Caregiving in natural setting
Treatment in institutional settings
Relationship
Adult-to-adult relationship
Expert-to-patient relationship
Medication
Medicate as appropriate and tolerate some illness symptoms
Medicate until symptoms are controlled
Decision making
Case management in partnership with patient
Physician makes decisions and prescribes treatment
Emphasis
Emphasis on strengths, self-help, and interdependence
Emphasis on dependence and compliance
Assessment
The Individual
Behaviors Related to Serious Mental Illness
Living Skills Assessment
PHYSICAL
EMOTIONAL
INTELLECTUAL
Living Skills
Personal hygiene
Human relations
Money management
Physical fitness
Self-control
Use of community resources
Use of public transportation
Selective reward
Goal setting
Cooking
Stigma reduction
Problem development
Shopping
Problem solving
Cleaning
Conversational skills
Sports participation
Using recreational facilities
Learning Skills
Being quiet
Speech making
Reading
Paying attention
Question asking
Writing
Staying seated
Volunteering answers
Arithmetic
Observing
Following directions
Study skills
Punctuality
Asking for directions
Hobby activities
Listening
Typing
Working Skills
Punctuality
Job interviewing
Job qualifying
Use of job tools
Job decision making
Job seeking
Job strength
Human relations
Specific job tasks
Job transportation
Self-control
Specific job tasks
Job keeping
Specific job tasks
The Family
Components of Family Assessment.
Recovery Support
Get Clinical Tree app for offline access



